Purpose
In the management of bulky chest wall recurrence of breast cancer, where there is no standard or clearly superior therapy, it is important to individualize patient care and treatment strategies [1]. Surgical resection of loco-regional recurrence should be expected if it may be safely administered with adjuvant systemic chemotherapy or hormonal therapy. Radiation therapy is also used to treat loco-regional recurrence in breast cancer patients after mastectomy [1, 2], especially in patients with unresectable tumors. In breast cancer patients with local recurrence, who have a long disease-free interval after mastectomy, long-term survival is often expected [3, 4]. In such cases, loco-regional salvage therapy should be administered with a curative intent.
Breast interstitial brachytherapy (ISBT) can be used as a boost after external beam radiotherapy (EBRT) or as monotherapy. A few studies have evaluated breast ISBT. Syed et al. reported that ISBT plus EBRT without surgery provides effective loco-regional control as an initial treatment in patients with locally advanced breast cancer [5]. Wu et al. demonstrated a re-irradiated case of high-dose-rate (HDR) ISBT alone for a bulky chest wall recurrence of breast cancer [6]. Roddiger et al. reported on 53 patients treated with HDR ISBT as neoadjuvant radiotherapy [7]. However, little is known about the clinical value of computed tomography (CT)-guided breast ISBT, especially for breast cancer patients with unresectable bulky tumors, even though CT-guided ISBT is a safe and feasible treatment approach for many cancer types [8-10]. Here, we describe the technique of CT-guided HDR ISBT and the efficacy of ISBT plus EBRT with hormonal therapy as a therapeutic option in patients with unresectable chest wall recurrence of breast cancer.
Case report
Patient presentation
We report the case of a 70-year-old woman who underwent HDR ISBT combined with EBRT as a radical treatment for unresectable bulky chest wall recurrence of breast cancer with bone and parietal pleura invasion. The patient was firstly diagnosed with a tumor in the right breast in 1998. The time elapsed from initial treatment was very long (20 years) and information about the initial histopathology or tumor stage was unavailable. She underwent a total mastectomy with adjuvant chemotherapy, followed by hormonal therapy for 5 years, with no adjuvant radiotherapy given. In 2008, 10 years after total mastectomy, follow-up confirmed the absence of recurrent disease. In 2018, the patient reported pain and swelling near the surgical scar and visited the hospital for a check-up. Ultrasound (US) revealed a bulky tumor; fine-needle biopsy confirmed the presence of malignant cells. Pathological evaluation indicated invasive pleomorphic lobular carcinoma positive for estrogen receptor (ER), and negative for progesterone receptor (PR) and HER2. This patient was clinically suspected to have recurrent breast cancer based on the tumor location. Ki-67 index was 22%, and 18F-labeled fluoro-2-deoxyglucose (18F-FDG) positron emission tomography (PET) with CT showed no lymph node or distant metastases (rT4N0M0). Plain and dynamic magnetic resonance imaging (MRI) was also performed to evaluate the local lesion. There were no tumors in the left breast on mammography, US, and dynamic MRI. Radiotherapy and hormonal therapy were recommended for the chest wall recurrence, which was approximately 10.5 cm × 7.3 cm × 4.5 cm, including erythematous skin involvement (approx. 1 cm). Surgery was not recommended due to the bone and pleura invasion. Written informed consent for EBRT plus HDR brachytherapy as curative radiotherapy was obtained.
Treatment
Hormonal therapy with anastrozole was initiated, followed by EBRT. During EBRT, the gross tumor volume (GTV) was contoured. No margin was added to the GTV to create clinical target volume (CTV). The CTV was expanded by 5 mm for planning target volume (PTV) as a margin to compensate for uncertainties in treatment delivery. During EBRT, 50 Gy in 25 fractions was delivered to the PTV using 3D conformal radiotherapy (Figure 1). The lungs and heart dosimetric parameters are described in Table 1. The patient was treated with 10-MV photons with a 5 mm bolus using an Elekta Synergy linear accelerator (Elekta; Stockholm, Sweden). ISBT was performed after completion of EBRT.
Fig. 1
Dose distribution in external beam radiotherapy (EBRT) planning. In this EBRT plan, the lung V5Gy and V20Gy (i.e., the percent volumes of both lungs receiving 5 Gy and 20 Gy, respectively) were 20% and 13%, respectively, and the mean heart dose was 5.6 Gy
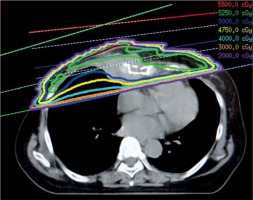
Table 1
Dose-volume histograms of the gross tumor volume (GTV), lungs, and heart during external beam radiotherapy (EBRT) and the first and second interstitial brachytherapy (ISBT) boost
Before the first implantation, repeated CT revealed a slight reduction in the tumor volume (9.0 cm × 6.5 cm × 3.5 cm). The first implant was performed 1 week after EBRT, and the second implant was done 4 weeks after the first implant. There was no evidence of lung invasion because the lung did not move with the tumor on US imaging under natural respiration. Before implantation, the insertion points and catheters’ paths were determined based on CT. To minimize the area of skin affected by high-dose, in the second implant, we selected different insertion points and catheters’ paths from those used in the first implant. The catheters were implanted under local anesthesia and after the administration of intravenous non-steroidal anti-inflammatory drugs in our outpatient clinic. During catheter implantation, the patient was placed in a supine position in an HDR room with a dedicated CT system (Figure 2A). Flexi-guide catheters (outer diameter, 5 French; length, 24 cm) were used as brachytherapy catheters. Sixteen-gauge needles were used to puncture the skin. The needles were replaced with the flexi-guide catheters after skin puncture. This process was repeated for each flexi-guide catheter. After penetrating the skin, the flexi-guide catheters were advanced using free-hand technique under serial CT imaging. We advanced each flexi-guide catheter carefully and slowly from the skin, lateral medially across the lesion, and toward anterior portion of the sternum under CT guidance to avoid puncturing the blood vessels and lungs. CT guidance provides good bone and soft tissue visualization. Therefore, CT enabled the brachytherapist to visualize the entire tumor with sternum invasion, and the catheters were placed just anterior of the sternum (Figure 3). The CT dose index and dose-length product from CT imaging for the implants were 475 mGy and 7081 mGy * cm, respectively. Once the catheter was properly inserted, the inner obturators were removed while maintaining the position of flexible catheters. The catheters were secured using dental putty (Exafine putty type®; GC Corporation, Tokyo, Japan). We used a similar catheter fixation technique for prostate brachytherapy [11]. After the dental putty hardened, it was sutured to the chest skin to hold the catheters in place (Figure 2B). Instant glue was applied to the catheters to secure them to the putty.
Fig. 2
Implantation of brachytherapy flexible catheters (A) and flexible catheters fixed with dental putty (light blue) (B). The putty was sutured to the skin using a thread (white arrow) to avoid catheter’s displacement. Catheters were attached to the putty using instant glue (tip of black arrow) to strengthen the fixation further
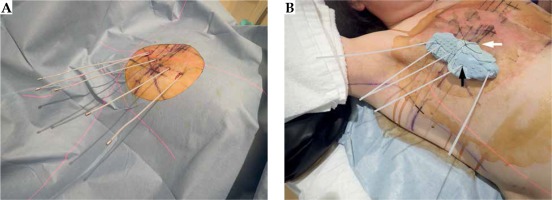
Fig. 3
Axial (A) and coronal (B) CT images of the gross tumor volume (GTV; red dashed lines), including the sternum lesions receiving 4 Gy (blue lines), 8 Gy (red lines), and 12 Gy (white lines). The catheters were implanted, penetrating the tumor and reaching the front of the sternum. The dental putty can also be seen (white arrows)
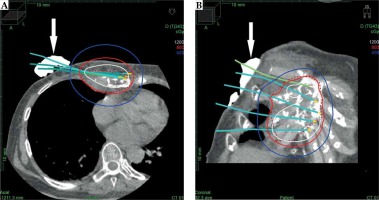
Brachytherapy planning CT was performed with a 1 mm slice thickness, and the GTV was contoured. Organs at risk (OARs) included the skin, ribs, lung, and heart. The prescription dose was set to 8 Gy per fraction. Three-dimensional brachytherapy plans were generated using Elekta Nucletron Oncentra treatment planning system version 4.5, with the inverse planning simulated annealing (IPSA) algorithm. Total equivalent dose of 2 Gy (EQD2) was calculated based on the assumption an α/β of 4 for breast carcinoma [12]. IPSA was used to achieve optimal dose distribution to the GTV D90% (i.e., minimum dose delivered to 90% of the GTV). The GTV was adjacent to the lung and heart due to the pleura invasion, so the prescription isodose line was intended to be positioned at the boundary between the GTV and the lung/heart. Lungs and heart dosimetric parameters in the first and second ISBT are described in Table 1. Not all of the lungs were scanned in the ISBT planning CT, therefore dosimetric parameters of the lungs were calculated using the total lung volume in the EBRT planning CT. GTV coverage was prioritized over skin-sparing, while the irradiated skin volume was kept as low as possible. The total GTV D90%, including the EBRT dose, was 82 Gy EQD2. Dose distribution is presented in Figure 3. CT was performed just before irradiation to confirm that the implanted catheters were not displaced. The patient was treated on the CT table without moving after the implantation. Two single-fraction implants of 8 Gy (interfractional interval of 28 days) were delivered to the GTV using MicroSelectron-HDR® (Nucletron B.V., Veenendaal, The Netherlands) with an 192Ir source. Five and seven catheters were used in the first and second ISBT, respectively. On the day of implantation, the patient received a single-fraction, after which the implant was removed. The patient was discharged after removing the catheters. No complications occurred during the whole brachytherapy procedure. After radiotherapy, hormonal therapy was administered until the last follow-up.
A blood tumor marker test was performed every month. Enhanced CT was done after 6 months, and 18F-FDG-PET/CT was performed after 14 and 26 months. Chest MRI was also completed after 28 months. Adverse events were evaluated using the common terminology criteria for adverse events version 4.0 (CTCAE v.4) [13]. Before and after salvage treatment, the levels of breast cancer antigen 225 (BCA225) and carbohydrate antigen 15-3 (CA15-3) were within normal physiological range. Serum level of the breast cancer marker carcinoembryonic antigen (CEA), which was 19.5 ng/ml pre-treatment, gradually decreased at 3 months after the first day of treatment; serum CEA levels remained within normal ranges through the last follow-up (CEA at the last follow-up of 30 months, 2.6 ng/ml). Enhanced CT examination at 6 months demonstrated that the size of the tumor was considerably reduced (Figure 4). Furthermore, MRI at 28 months and 18F-FDG-PET/CT at 26 months indicated that the bulky tumor had disappeared (Figures 4 and 5). There was no evidence of tumor recurrence at the 30-month follow-up. The patient exhibited acute dermatitis (grade 2) in the irradiated area (EBRT and ISBT) for nearly 2 weeks after irradiation, which was managed with a steroid ointment. White petroleum (Vaseline) was used to moisturize the irradiated skin. Telangiectasia was apparent from 1 year after radiotherapy, until the last follow-up (Figure 6). CT and 18F-FDG-PET/CT revealed a radiation-induced inflammatory change in the lungs (grade 1). There were no severe (grade 3 or higher) complications. The pre-treatment pain near the surgical scar disappeared after irradiation.
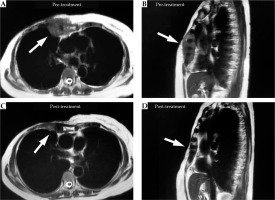
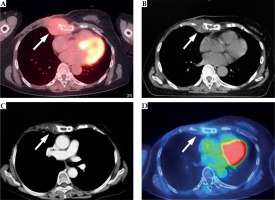
Fig. 4
Axial 18F-FDG-PET/CT image before radiotherapy (A), axial plain CT image before the second interstitial brachytherapy (ISBT) (B), enhanced axial CT image at 6 months (C), and axial 18F-FDG-PET/CT image at 26 months (D). The bulky tumor with bone invasion (A, white arrows) on the right chest wall decreased in size (B and C, white arrows) and finally disappeared (D, white arrows)
Discussion
Radiation oncologists are often asked to manage patients with localized, yet unresectable disease. Local control is essential for quality of life and survival of these patients. The optimal tumor control dose for unresectable bulky breast tumors and optimal irradiation method remain to be determined, although NCCN guidelines [2] state that radiotherapy may be considered for unresectable local recurrence in post-mastectomy patients with no prior radiotherapy. In the absence of established standard therapy, a radiation oncologist needs to individualize treatment and provide personalized care. Brachytherapy can provide the most conformal and precise radiotherapy. Based on the case described here, we believe that outpatient CT-guided ISBT boost is a beneficial therapeutic option for breast cancer patients with unresectable chest wall recurrence.
We found CT guidance useful in this case. CT can visualize the entire tumor, including bone invasion. Wu et al. reported the use of US-guided HDR ISBT to treat a bulky chest wall recurrence in a breast cancer patient [6]. In our case, the additional information provided by CT was helpful in accurately placing the catheters. Therefore, if a resource is available, we believe this approach should be considered.
The application of brachytherapy may achieve improvement of loco-regional control of bulky unresectable breast tumor, as brachytherapy can deliver a higher internal dose, which may improve control of radio-resistant tumor cells and reduce the risk of viable residual disease. In patients with bulky unresectable tumors, EBRT alone may not provide adequate loco-regional control [14]. Fröhlich et al. [15] demonstrated that EBRT plus ISBT after breast surgery allowed for delivery of higher doses compared with EBRT alone.
Brachytherapy permits for precise dose delivery despite chest movements due to respiration. The implanted catheters can retain a stable position in relation to the tumor. Fixation of the catheters is essential to reduce the risk of catheter displacement. Here, we used dental putty to custom-fit patient’s anatomy and the implanted catheters. Alternative method of implant using a template may be also feasible. However, we found free-hand method technically simple, with additional benefit of being very adaptable for a variety of different clinical presentations. Also, we accomplished our goal of securing the catheters with a custom-fitted mold, which we believe, further minimized the patient’s discomfort. Furthermore, the implantation and treatment were performed in the same position without moving the patient, which further reduced the risk of catheter displacement. A HDR room with a dedicated CT system facilitated this approach.
The total number of catheters may depend on not only target size and shape, but also dose distribution from prior treatment fractions. In the outpatient setting, we used 5 catheters during the first ISBT, whereas more catheters were applied in the second ISBT to further improve dose distribution. Using more catheters provided a better dose distribution at the expense of increased operating time. However, more catheters may also cause more patient’s discomfort. To further minimize hot spots in the treatment volume, we shifted catheters’ positions between the first and the second ISBT by selecting different insertion points and catheters’ paths to reduce higher dose volumes as much as possible. Fortunately, our patient did not suffer from severe skin toxicity associated with brachytherapy hot spots. In general, due to close proximity between treatment volume and the skin, it may be difficult to accomplish strict skin sparing without compromising tumor coverage. It is especially challenging if there is a gross tumor invasion of the skin. Application of stricter skin dose constraints may result in missing the target and local recurrence. More data is needed to resolve this issue. The optimal dose for treatment of bulky breast tumor recurrence has not been established. The total dose for the GTV D90% was intended to be ≥ 80 Gy (EQD2), and therefore, the total dose was 82 Gy. Syed et al. reported results of 90-100 Gy using EBRT plus ISBT for T3 and T4 breast tumors [5], and we believe that this is a useful guideline until more data become available. Currently, there are few specific radiotherapeutic recommendations for unresectable loco-regional recurrence in breast cancer patients after mastectomy with no prior radiotherapy [2]. Neoadjuvant radiotherapy using HDR ISBT may be a treatment option for unresectable breast tumors. Roddiger et al. demonstrated the possibility of neoadjuvant HDR ISBT for breast cancer patients, who could not be treated with breast-conserving surgery due to the initial tumor size or unfavorable breast-tumor ratio [7]. Neoadjuvant radiotherapy may be a treatment option if it is not for a bone or parietal pleura invasion case.
It is always important to maximize loco-regional control and to minimize the treatment burden for our patients. Our treatment was delivered with EBRT and two outpatients’ implants. It may be possible to deliver multiple fractions or whole treatment with a single-implant; however, we selected single-fraction implants to re-distribute high-dose volume by slightly varying catheters’ positions with each implant. Moreover, two implants were chosen to deliver the treatment, a reasonable number for the patient in our outpatient setting. It may be possible to further reduce the treatment time by modifying the fractionation and contribution of the total dose by modality. Further investigation is warranted.