Purpose
According to the guidelines of the National Comprehensive Cancer Network [1] and the European Association of Urology [2], the recommended standard therapy for low-risk prostate cancer includes low-dose-rate brachytherapy (LDR-BT) alone or external-beam radiation therapy (EBRT) alone. For intermediate-risk prostate cancer, the guidelines suggest either LDR-BT, EBRT, or a combination of these therapies. However, temporary worsening after LDR-BT in terms of international prostate symptom score (IPSS), a measure of lower urinary tract symptoms (LUTS) [3], and seven-grade urinary quality of life (uQoL), a measure of satisfaction with LUTS [3], has been reported [4-9]. Correlations between IPSS and uQoL after LDR-BT have also been reported [10]. In a previous study, patients who underwent LDR-BT alone were more likely to experience worsening of urinary incontinence and irritative symptoms after 6 months and 1 year when compared with patients who underwent EBRT alone [11]. Therefore, patients must be monitored for worsening of LUTS and decrease in uQoL after undergoing LDR-BT. IPSS consist of seven lower urinary tract symptoms, including incomplete emptying, frequency, intermittency, urgency, weak stream, straining, and nocturia. Although the importance of uQoL in patients undergoing LDR-BT for prostate cancer has been established, few reports are available, in which all seven LUTS were associated with uQoL following LDR-BT. Moreover, no study has identified LUTS that must be considered to improve uQoL after LDR-BT.
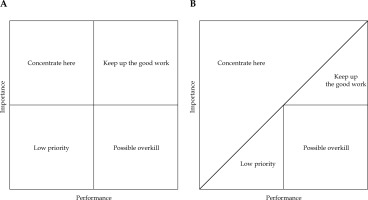
Importance–performance analysis (IPA), developed by Martilla and James in 1977, helps understand the prioritization of services for improving customer satisfaction [12]. IPA has been used in business domain as well as medical and public health fields, as an approach to enhance patient satisfaction and health [13, 14].
The current study aimed to investigate IPSS and uQoL scores of patients with prostate cancer who underwent LDR-BT alone, and to determine the period during which the uQoL score declined. IPA was performed with the period of uQoL decline to identify LUTS that should be prioritized for improvement in post-operative urinary quality of life. Furthermore, the clinical and dosimetric factors associated with each of these LUTS were investigated.
Material and methods
Study design and patients
This retrospective study was approved by the Institutional Review Board of our hospital (approval No.: 2022-321 [114217]), and conducted in accordance with the principles of the Declaration of Helsinki. Between March 2011 and January 2022, 268 patients diagnosed with prostate cancer classified as low-risk or intermediate-risk disease according to D’Amico risk classification underwent LDR-BT using permanent iodine-125 (125I) seed implantation. Only patients who could be followed for at least 1 year after LDR-BT were included in this analysis.
LDR-BT protocol
Patients with intermediate-risk prostate cancer or large prostate volume received neoadjuvant hormonal therapy 3-4 months prior to LDR-BT.
Day 0. A previously reported real-time intra-operative planning technique was applied to implant 125I seeds permanently [15]. Intra-operative real-time peripheral loaded implant technique outlined by Stock et al. was used in this study [16]. Seed activity value was 11.0 or 13.1 MBq, and prescribed implantation dose was 145 Gy. Intra-operative planning aimed to maintain the dose covering 90% of the prostate (D90) at a level of ≥ 160 Gy, the prostate receiving 100% of the dose (V100) at ≥ 95%, the prostate receiving 150% of the dose (V150) at ≤ 60%, the dose covering 30% of the urethral volume (uD30) at ≤ 200 Gy, and the urethral volume receiving 150% of the dose (uV150) at ≤ 0.0 cc. The patient was transferred from the operating room to the hospital room post-implantation with urinary catheter in place.
Day 1. Computed tomography (CT) was performed with urinary catheter in place to verify seed placement and presence of hematomas. The urinary catheter was removed if no issue was identified. Administration of α1-blocker (0.2 mg/day of tamsulosin, or 8 mg/day of silodosin) was initiated according to clinical protocol. Patients who have been taking an α1-blockers prior to implantation were instructed to continue taking them.
Day 2. The patient was discharged.
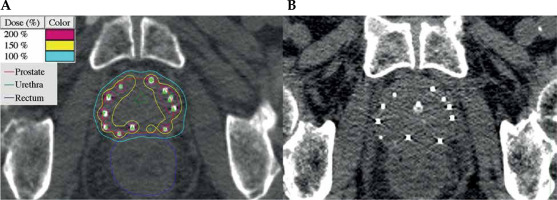
Day 30. Post-implantation dosimetry was performed using CT and magnetic resonance imaging (MRI) results. CT imaging and MRI fusion was performed, followed by prostate contouring predominantly with MR images. Urethral positioning for post-implantation dosimetry was determined based on CT image acquired on the day after implantation. Urethral contour for post-implantation dosimetry was established as an equilateral triangle of 7 mm on CT image (Figure 1A, B). CT images were used to identify the implanted seeds, and dosimetric parameters for the prostate and urethra were calculated. Dosimetric parameters investigated included D90, V100, V150, the dose covering 5% of the urethral volume (uD5), the dose covering 10% of the urethral volume (uD10), uD30, the dose covering 90% of the urethral volume (uD90), uV150, and the urethral volume receiving 200% of the dose (uV200).
Fig. 1
Computed tomography (CT) images acquired for post-implantation dosimetry (A). CT image obtained on the day after implantation (B). Urethral region of interest is delineated on CT image for post-implantation dosimetry (A) based on CT image acquired on the day after implantation with an indwelling urethral catheter (B)
Assessment of LUTS and urinary QoL
LUTS and uQoL scores were assessed using IPSS and the seven-grade uQoL score before implantation, at 1 and 3 months post-implantation, and every 3 months thereafter.
Importance–performance analysis
In the original IPA, importance and performance are derived via customer surveys, where importance indicates the significance of attribute to the customer, and performance is customer satisfaction with the attribute. A two-dimensional matrix-grid is constructed, with importance on the vertical axis and performance on the horizontal axis [12]. After evaluating performance and importance of various attributes, their means are plotted on four quadrants of the matrix-grid. Attributes with low performance but high importance are prioritized for improvement and classified into ‘concentrate here’ quadrant. The other quadrants are ‘keep up the work’, ‘low priority’, and ‘possible overkill’ (Figure 2A). Several modifications have been made to the IPA methodology [17, 18]. One popular modification is the diagonal line model [18-21] that involves adding an iso-priority or iso-rating line, a diagonal line at a 45-degree angle to IPA grid. Bacon reported that the diagonal line model outperformed the original IPA, and strongly recommended its use for IPA [22]. In 2007, Abalo et al. improved the diagonal model further and divided it into four quadrants [23]. Attributes above the diagonal line are categorized into ‘concentrate here’ region. Regions below the diagonal line are further divided based on the midpoint of importance and performance scale: ‘low priority’ for the low performance region, ‘keep up the work’ for the high performance and high importance region, and ‘possible overkill’ for the high performance and low importance region. Building on these findings, the IPA grid modified by Abalo et al. was applied for this analysis (Figure 2B). IPSS score of each symptom was used for performance on the horizontal axis. Regression coefficients from a multiple regression analysis were used as indirect importance in the vertical axis [24, 25]. Regression coefficient calculated from a multiple regression analysis between each LUTS score and uQoL score was utilized as the measure of importance. LUTS situated above the diagonal line were considered candidate LUTS for intensive improvement to enhance uQoL, as their importance level exceeded their corresponding performance rating.
Statistical analysis
Urinary QoL scores were compared pre-implantation and at each post-implantation time point using Wilcoxon rank-sum test to identify the period of uQoL post-implantation deterioration. The afore-mentioned IPAs were conducted pre-implantation, during periods of uQoL declining, and during periods of uQoL improving. Univariate analysis (UVA) of the association between each of the seven LUTS scores and each factor was performed using Student’s t-test or simple regression analysis, as appropriate. Statistical significance was set at p < 0.05, and all variables demonstrating statistical significance in UVA were selected and incorporated into multivariate analysis (MVA) using multiple regression analysis. LUTS scores during periods of uQoL deteriorating were summed for each patient, and utilized as an objective variable in UVA and MVA. Receiver operating characteristic (ROC) curve analysis was performed using dosimetric parameters significantly related to LUTS score to predict an average score of ≥ 3. Cut-off values were determined with Youden’s index [26]. All statistical analyses were performed using EZR software (Saitama Medical Center, Jichi Medical University, Saitama, Japan) [27].
Results
Clinico-pathological characteristics of patients
Table 1 presents patient characteristics. Among 268 patients screened initially, 75 were lost to follow-up within 1 year, and were excluded from the analysis. A total of 193 patients were included in the analysis. The median age of the participants was 68 years (range, 50-80 years), and the median follow-up period after implantation was 30 months (range, 12-120 months; 142, 19, and 32 patients were followed up for ≥ 24, 18, and 12 months, respectively). According to D’Amico risk classification, seventy patients had low-risk disease, whereas 123 patients had intermediate-risk disease.
Table 1
Patient characteristics (N = 193)
Longitudinal changes in LUTS and uQoL
Figure 3 presents longitudinal changes in IPSS and uQoL scores. IPSS exhibited a significant increase from the baseline (BL) value at 1 month post-implantation (mean score, 15.9 vs. 6.8 [BL]; p < 0.001); however, it returned to the BL value by 18 months post-implantation (mean, 7.3 vs. 6.8 [BL]; p = 0.380). The uQoL score reached its highest level at 1 month post-implantation (mean: 3.6 vs. 2.3 [BL], p < 0.001), and returned to the BL value by 12 months post-implantation (mean: 2.5 vs. 2.3 [BL]; p = 0.077). The IPSS and uQoL scores showed similar trends, increasing significantly from the BL values at 1 month post-implantation and then gradually returning to the BL values.
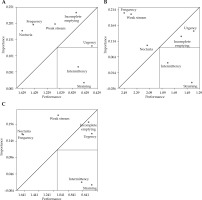
Importance–performance analysis
Importance–performance analysis was conducted across three time periods, such as pre-implantation, 1-9 months post-implantation during uQoL deterioration, and 12-24 months post-implantation during uQoL improvement (Figure 4). LUTS, including frequency, nocturia, and weak stream were targeted for intensive improvement across all the time periods. In addition, incomplete emptying was targeted for intensive improvement pre-implantation. The performance of frequency and weak stream decreased noticeably during the period of uQoL deterioration, whereas their importance increased noticeably. The performance of weak stream improved during the period of uQoL improvement; however, the importance remained high. In contrast, the performance of frequency did not improve during the period of uQoL improvement, but its importance decreased.
Identification of factors associated with LUTS scores
Table 2 presents results of UVA and MVA comparing LUTS scores during the period of uQoL deterioration with clinical and dosimetric factors. As the uQoL scores were at their lowest in 1-9 months post-implantation (Figure 3), each LUTS score was summed during these periods and used as an objective variable. Each LUTS score and its BL value were significantly associated in MVA (each p < 0.001, positive correlation). LUTS, such as frequency, incomplete emptying, urgency, and straining scores were significantly associated with the prostate volume (p = 0.028, 0.009, 0.002, and 0.005, respectively, positive correlation). The weak stream score was associated with D90 (p = 0.032, positive correlation), whereas the intermittency score was associated with uD90 (p = 0.042, positive correlation).
Table 2
Association of each lower urinary tract symptom score with each factor
[i] UVA – univariate analysis, MVA – multivariate analysis, Dxx – dose covering xx% of the organ volume, Vxx – the organ receiving xx% of the dose, * statistically significant; objective variables – combined scores at 1, 3, 6, and 9 months post-implantation (i.e., the urinary quality of life deterioration period)
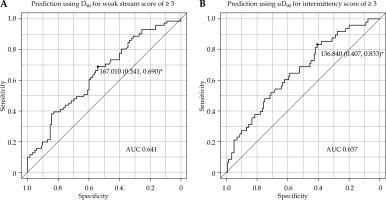
Identification of dosimetric cut-off values for prediction of ≥ 3 average score
ROC curve analysis was applied to predict average score of ≥ 3 for each LUTS score during the period of uQoL deterioration (Figure 5). The cut-off value for D90, predicting an average score of ≥ 3 for weak stream, was 167.01 Gy (specificity, 0.541; sensitivity, 0.690), yielding an area under the curve (AUC) of 0.641 (95% CI: 0.56-0.721%). The cut-off value for uD90, predicting an average score of ≥ 3 for intermittency, was 136.84 Gy (specificity, 0.407; sensitivity, 0.833), resulting in an AUC of 0.657 (95% CI: 0.57-0.745%).
Fig. 5
Receiver operating characteristic curve of D90 for the prediction of an average weak stream score of ≥ 3 (A), and uD90 for the prediction of an average intermittency score of ≥ 3 (B). D90 – dose covering 90% of the prostate, uD90 – dose covering 90% of the urethra, AUC – area under curve, * cut-off point (specificity, sensitivity)
Discussion
This study revealed that a period of 1-9 months after LDR-BT for prostate cancer is the period, in which the uQoL score deteriorates, and LUTS, such as frequency, nocturia, and weak stream should be considered intensively to improve uQoL scores during this period. The LUTS scores tend to increase mainly in patients with low BL scores or large prostate volume. D90 and uD90 are associated with frequency and intermittency, respectively, and should not exceed 167.01 Gy and 136.84 Gy, respectively, to prevent significant deterioration in LUTS.
Studies on longitudinal changes in the IPSS and uQoL scores after LDR-BT reported that IPSS returned to the BL value after 12-36 months [5-8, 28, 29], and uQoL returned to the BL value after 12 months [5, 7, 8], which is consistent with the results of the present study. Frequency, nocturia, and weak stream were LUTS to be improved in IPA at any phase. In addition, incomplete emptying was also an important LUTS to be improved pre-implantation. Among the seven LUTS, nocturia, incomplete emptying [30-32], frequency [31], and weak stream [32] were shown to be associated with worse uQoL, although these studies did not focus specifically on patients who underwent radiation therapy for prostate cancer. These four LUTS are consistent with the ‘concentrate here’ symptoms in the pre-implantation IPA. The importance of weak stream increased in the period of uQoL deterioration (1-9 months); however, the performance of weak stream decreased noticeably. During the uQoL improvement period (12-24 months), the performance of frequency remained low, but its importance decreased. In other words, the symptoms to be focused on for improvement vary in each phase, so an approach tailored to each phase is required. Yoshimura et al. reported that weak stream, incomplete emptying, and nocturia were associated with worse uQoL in Japanese patients with benign prostatic hyperplasia (BPH) [32]. Although newly diagnosed patients with BPH suffered from frequency, urgency had the strongest impact on uQoL in pre-operative patients with BPH [32]. In a French community-based study, urgency was the most bothersome LUTS [33]. This may be due to the differences in study populations, ethnicity, or cultural differences.
An association was observed between D90 and weak stream during the uQoL deterioration period, and the cut-off value was 167.01 Gy in the present analysis. Stock et al. reported that D90 > 180 Gy was associated with increased urinary symptoms [34]. Tanimoto et al. reported that V100 of the prostate was linked to urinary toxicities [7]. Although prostate treatment intensity and dose coverage are associated with urinary toxicities, a significant reduction in biochemical recurrence has also been reported after receiving prostate D90 > 180 Gy [35, 36]. Stock et al. suggested that optimal 125I prostate implants should deliver a D90 of 140-180 Gy to balance urinary toxicity and biochemical recurrence [34]. In the present study, an association was observed between uD90 and the intermittency score during the period of uQoL deterioration. UD90 has been reported to be associated with IPSS increment [29] and urinary toxicities [37]. Furthermore, uD90 is associated with obstructive urination among LUTS [38]. Intermittency is a symptom of ‘possible overkill’ in IPA; therefore, little improvement in uQoL can be achieved by maintaining uD90 below 136.84 Gy. However, it is also associated with weak stream in UVA that may lead to lower weak stream scores and improved uQoL.
Recent systematic reviews have shown that α1-blockers improve LUTS and uQoL after brachytherapy [39]. However, all patients started receiving them internally immediately post-implantation.
Other approaches, such as adequately considering patient’s LUTS during consultation, empathic attitude, and positive approach (being positive about the problem and when it would settle) may lead to improved patient satisfaction, i.e., better uQoL [40]. Adequate patient education about the causes of symptoms and effects of alcohol and caffeine intake is also important to improve LUTS and uQoL [41, 42].
The present study is limited by its retrospective design. IPSS was calculated based on the frequency of each symptom, with a maximum score of 5 for each symptom. Patients with a high frequency of pre-implantation symptoms will already have a maximum score of 5; therefore, post-implantation evaluation may not capture potential worsening of symptoms. As a potential solution, IPSS evaluations should be conducted using a visual analog scale in the future [31]. In addition, patients who declined to complete the IPSS questionnaire or were subsequently followed up at a different institution within 1 year of post-implantation were excluded from this study, potentially introducing selection bias. It is important to note that such bias may have affected the study results, as patients with more severe symptoms could have been more willing to complete the questionnaire, whereas those with no or mild symptoms may have opted for follow-up at a nearby facility. Furthermore, D90 and uD90 were evaluated as predictors for weak stream and intermittency scores using ROC curves. However, the obtained AUC values were 0.641 and 0.657, indicating limited predictive capability. These modest AUC values highlight the limitations of D90 and uD90 as standalone dosimetric predictors, suggesting the need for further research to identify stronger dosimetric predictors.
Conclusions
In conclusion, this study utilized IPA during the period of uQoL deterioration (1-9 months) after LDR-BT for prostate cancer to prioritize LUTS improvement in prostate cancer patients based on performance and importance ratings. Frequency, nocturia, and weak stream were identified as the priority areas for improvement during the period of uQoL deterioration. The factors associated with these symptom scores were also identified. As for the dosimetric factors, LUTS, such as weak stream and intermittency were associated with D90 and uD90, respectively. The results of this analysis can be used to prioritize LUTS that need to be improved in daily medical care. The results of this analysis can be used to plan treatment with a greater awareness of uQoL following LDR-BT, thus helping patients and healthcare professionals to determine goals.