Introduction
Dysmenorrhoea is a condition frequently reported by women of childbearing age. It occurs in 50–90% of women of childbearing age, with the highest incidence between 19 and 23 years of age. Based on its aetiopathogenesis, we distinguish primary and secondary dysmenorrhoea. Secondary dysmenorrhoea is associated with the occurrence of pathologies in the pelvis, which include, among others, endometriosis. In contrast, primary dysmenorrhoea is associated with the presence of ovulatory cycles and the overproduction of prostaglandins in the endometrium. It may be accompanied by a number of other symptoms, such as back pain, nausea, diarrhoea, fatigue, mood disorders, or fainting [1–6].
Primary dysmenorrhoea mainly affects young women with no history of pregnancy or childbirth. In the past, this problem was less widespread than it is today, due to the relatively young age of giving birth to the first child. According to EUROSTAT data, in Poland, the median age of giving birth to the first child is just over 27 years, which means that a woman may suffer from these symptoms for a considerable period of her life. Factors that increase the risk of dysmenorrhoea of primary aetio-logy include early menarche age, heavy and prolonged menstrual bleeding, exposure to stress, mood disorders, anxiety disorders, weight loss, low physical activity, or use of stimulants (tobacco, alcohol) [2, 7–9].
The severity of the symptoms of dysmenorrhoea may significantly affect the scientific and professional activity of women, as well as their family and social life. The symptoms occurring during menstruation also affect the woman’s emotional state, which may contribute to the occurrence of premenstrual syndrome, premenstrual dysphoric disorder (PMDD), depression, or other mood disorders [4].
Dysmenorrhoea is a significant interdisciplinary problem that requires the intensified activities of specialists, mainly in the fields of health sciences, gynaecology, and pharmacology. Proper diagnosis and the implementation of effective treatment are the key to women’s coping with this condition and may result in increased psychological comfort, professional performance, improved relationships with close friends and relatives, and their overall well-being [1, 4].
Aim of the study
The aim of the study is to learn about the experiences of women reporting dysmenorrhoea, including ways of coping with it and its impact on daily life activities.
Material and methods
The study was conducted between January and March 2020 using a diagnostic survey in the form of a questionnaire developed for the purpose of the study, which was then distributed via social media. The questionnaire consisted of 26 questions concerning the symptoms of dysmenorrhoea, ways of dealing with it, its impact on one’s personal, family, and professional life, as well as the demographic and social situation of the study participants. Participation in the survey was voluntary and anonymous.
The study group was selected based on the following criteria:
inclusion: women between 18 and 45 years of age, who experienced dysmenorrhoea lacking confirmed diagnosis of pelvic pathology, indicating a secondary cause of the symptoms,
exclusion: women below 18 years of age and women aged 18–45 years, who had not had periods in the previous 12 months or had reported pelvic pathology that may cause secondary dysmenorrhoea, or had not reported painful periods.
The questionnaire was completed by 192 respondents, with 9 women declaring painless periods, and 17 women reporting pelvic pathologies. After applying the exclusion criteria, a total of 166 questionnaires were analysed.
The analysis of collected data was performed with the aid of Microsoft Office Excel 2007 and Statistica 13.1. The statistical significance was 0.05 and, the test power was 0.80. The distribution of variables was tested with the Shapiro-Wilk test. Qualitative variables were compared using the χ2 test with correction for low frequencies, and quantitative variables were compared using the Mann-Whitney U test (with continuity correction).
Results
Study group characteristics
Most of the study group were women between 18 and 25 years of age, with higher education, living in a large city, and not having children. Detailed characteristics of the study group are presented in Table 1.
Table 1
Study group characteristics (n = 166)
Women’s experience analysis
According to over three-fourths of the surveyed women, menstrual pain should not occur at all, and at the same time it does not have to be indicative of any pathological symptoms. Most of the study participants experienced severe menstrual pain. Nearly half of the study participants consulted their symptoms with a doctor or midwife (Table 2).
Table 2
Incidence of menstrual pain (n = 166)
First menstrual pain was noticed from menarche by 43.98% of surveyed women, and by 56.02% after a few years and later in life. Statistically significantly, the women who experienced their first menstrual pain after a few years and later experienced menstrual pains that lasted 1 or 2 days more often than the respondents who had struggled with the pain since menarche. More often, the women surveyed with first pain from menarche were afflicted with a pain lasting 3 or more days and had a higher average assessment of the severity of pain than other respondents. Those surveyed also often consulted their condition with a doctor or midwife (Table 3).
Table 3
Assessment of menstrual pain in terms of the first time of incidence of pain symptoms (n = 166)
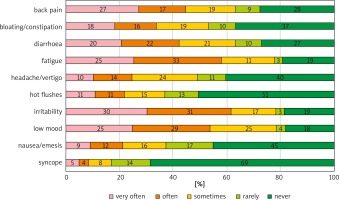
The women were asked to indicate the symptoms that accompany dysmenorrhoea and the frequency of their occurrence. The most common symptoms listed were depressed mood, irritability, and fatigue. Most of the study participants experienced these symptoms “very often” or “often”. A total of 69% of the study participants never experienced fainting with painful menstruation (Fig. 1).
The severity of pain was statistically significantly correlated with symptoms such as nausea (r = 0.44, p < 0.000), headache and dizziness (r = 0.41, p < 0.000), and syncope (r = 0.41, p < 0.000). The degree of severity is pain correlated with the resignation from simplifying sports (r = 0.45, p < 0.000) and reorganization (r = 0.39, p < 0.000) and consultation with the procedure/midwife (r = 0.46, p < 0.000). Pain duration was significantly correlated with headaches and dizziness (r = 0.41, p < 0.000).
Among the study participants, 86.14% used pharmacological methods for relieving menstrual pain. The most frequently chosen analgesics were those containing ibuprofen, drotaverine, and paracetamol. Most study participants declared that they were satisfied with the effects of pharmacotherapy (Table 4).
Table 4
Use of pharmacotherapy for menstrual pain (n = 143)
Among the respondents, non-pharmacological methods of relieving menstrual pain, chosen by 74.10% of women, were also popular. Most of the study participants chose warm compresses and taking a bath/shower. They were least likely to use aromatherapy. More than half of the study participants were satisfied with the positive effects of non-pharmacological methods on the relief of menstrual pain (Table 5).
Table 5
Use of non-pharmacological treatments for menstrual pain (n = 123)
The respondents reported that dysmenorrhoea affected their everyday lives. For almost half (48.19%) of the study participants, the occurrence of dysmenorrhoea involved the reorganization of previous arrangements. Statistically significantly, women with first menstrual pain after a few years later experienced less cancellation of classes or appointments associated with dysmenorrhoea than other respondents. Among women with first menstrual pain from menarche, dysmenorrhoea was more often related to cancelling classes, or appointments, at least once a month. There was no difference between women in the issue of giving up sports (Table 6). A total of 67.47% of the study participants reported receiving understanding from their relatives (Table 7).
Table 6
Assessment of women’s functioning with menstrual pain in terms of the first time of incidence of pain symptoms (n = 166)
Discussion
Dysmenorrhoea is a condition that affects various aspects of a woman’s life. Early diagnosis of the problem and a holistic approach to treatment contribute to the use by women of appropriate methods for coping with this condition, as well as better well-being and the possibility of self-realization.
In our study, 183 out of 192 women (95%) experienced pain during menstruation, and in most cases (86.5%) it was not entirely diagnosed or not recognized as a secondary dysmenorrhoea. The problem of dysmenorrhoea affects women all over the world, as shown by the results obtained by other researchers. In a study by Unsal et al., dysmenorrhoea occurred in 72.7% of Turkish female students. Söderman et al. found that 89% of Swedish teenagers reported dysmenorrhoea. In the study by Omidvar et al., 70.2% of young women from the southern part of India suffered from dysmenorrhoea of primary aetiology [6, 10, 11].
For most of the women who participated in the study, pain started with the menarche or a few years after the menarche. However, in 5.42% of women the pain appeared later in life, which may indicate a secondary cause of the symptoms. Therefore, one should assume some underestimation of the incidence of secondary dysmenorrhoea, which may result from insufficient diagnostics [1].
Following the criteria adopted in our study, 63.25% and 24.7% of women assessed the level of experienced menstrual pain as severe or moderate, respectively. In other works, divergent results were obtained. In the study by Kazama et al., conducted among Japanese schoolgirls, very painful menstruation was reported only by 17.7% of the study participants, and 46.8% of women experienced pain described as “moderate”. In the study by Unsal et al., about 66.2% of the study participants described their ailments as severe and moderate [10, 12].
In addition to pain, women noticed several other symptoms accompanying menstruation. In our study, most of the study participants reported low mood, irritability, and fatigue. Other common complaints included diarrhoea (73%), back pain (72%), and bloating/constipation (63%). The least frequently reported symptoms were hot flushes (59%) and syncope (31%). By comparison, in a study by Fernandez-Martinez et al. on the experiences of menstruation among Spanish nursing students, the most common symptoms were bloating (87.3%), irritability (76.3%), and fatigue (70.6%). In the study by Söderman et al., the dominant symptoms in young Swedish women were fatigue (83%) and headaches (82%). Similarly to the results of our own study, Swedish women were least likely to experience syncope (10.7%). Young South Indian women, apart from fatigue and irritability, most often complained of back pain. On the other hand, young Turkish women most frequently reported irritation, fatigue, anxiety, and breast tenderness [6, 11, 13, 14].
Despite the occurrence of various symptoms during menstruation, more than half of the women did not consult with a gynaecologist or midwife regarding their condition. The works of other researchers show that the respondents rarely attended medical appointments for this reason. Subasinghe et al. studied the incidence and severity of dysmenorrhoea in Australian women. Their results indicate that only 34% of the respondents visited a doctor. In the study by Söderman et al., 7% of young women consulted a doctor and 33% discussed their complaints with other healthcare professionals (midwife, school nurse). In a study conducted in southern India, every fifth respondent attended a doctor’s appointment [6, 11, 15]. Failure to report the problem to medical staff may stem from women’s misconception that these symptoms are related to the physiological condition of having a period.
Most respondents (86.14%) took both prescription and over-the-counter analgesics. The most frequently chosen ones were those containing ibuprofen. This substance, like ketoprofen and nimesulide, belongs to the group of non-steroidal anti-inflammatory drugs, which are effective in the treatment of dysmenorrhoea. Apart from ibuprofen, the respondents often reported the use of paracetamol and drotaverine, which are not indicated in the treatment of primary dysmenorrhoea. Women took these drugs without consulting a doctor; they often took incomplete, sub-therapeutic doses, which may bring about an unsatisfactory therapeutic effect [2, 16, 17].
In our study, less than 75% of women used alternative methods for dealing with dysmenorrhoea, and more than half of them were satisfied with their use. The most preferred pain relief methods were warm compresses (70%) and taking a bath/shower (66.67%). Every fourth respondent did physical exercises. The results of the study by Chaudhuri et al. indicate that physical exercise and the use of warm compresses contribute to the reduction of menstrual pain, as assessed by the respondents. A study by Armor et al. demonstrated the positive effect of lifestyle changes during dysmenorrhoea, including doing low-intensity physical activity. In the examined patients, pain was less severe and it lasted for shorter periods. A study by Bavil et al. proved that women who are physically active report less pain than those who are inactive. The results of a study by Dehnavi et al. confirm that regular aerobic exercise of moderate intensity can reduce or prevent the occurrence of some menstrual pain disorders; therefore, this type of exercise is recommended in the treatment of primary dysmenorrhoea [18–21].
Symptoms related to dysmenorrhoea negatively affect a woman’s social life. As a result, women limit their scientific and professional activity and give up social meetings. Almost half of the respondents admitted reorganizing their previous arrangements due to the occurrence of symptoms. Over one-third of the respondents claimed that pain did not affect their plans. Most of the respondents (71.69%) gave up practicing sports at that time. In a study by Pitangui et al. on the impact of dysmenorrhoea on daily life, most of the respondents (66%) stated that dysmenorrhoea affected their everyday life. Fernandez-Martinez et al. noted that dysmenorrhoea is one of the main causes of school/work absence, and absenteeism was more common in women who also experienced symptoms other than abdominal pain. The results of the study by Omidvar et al. indicate that 51.1% of Indian women missed classes due to symptoms related to menstruation [6, 13, 22].
Most of the surveyed women met with an understanding of their condition on the part of their relatives. However, 13.85% of the respondents did not receive support from their immediate environment. According to Chen et al., menstruation is still taboo in some cultures and can be embarrassing. Symptoms that are not often treated seriously enough can lead to downplaying of the problem by both relatives and healthcare professionals [23].
Dysmenorrhoea affects a woman’s physical well-being, mental health, and social life. Although this condition occurs in many women, it is often downplayed and underdiagnosed, and therefore untreated. The consequences of dysmenorrhoea affect the quality of life, which has been demonstrated in the results presented by various researchers. Unsal et al. found a correlation between dysmenorrhoea and its accompanying symptoms and lower health-related quality of life values. In a study by Iacovides et al., women experiencing primary dysmenorrhoea showed lower life satisfaction [10, 24].
Medical personnel who care for women and are aware of the problems related to dysmenorrhoea and its aetiology may play a crucial role in the correct diagnosis of this condition. Initiating a conversation with women about their symptoms during menstruation and collecting a thorough medical history allows to use diagnostic methods and implement effective pharmacotherapy or other treatment procedures for suffering patients. Furthermore, due to appropriate education on methods of alleviating menstrual pain other than medicinal treatment, the women acquire the ability to cope with dysmenorrhoea. Support on the part of medical personnel contributes to better daily functioning of their patients, significantly improving the quality of women’s lives [16, 24, 25].
Conclusions
Women with menstrual pain prefer using analgesics. Pharmacotherapy often used by women is outside the treatment regimen of dysmenorrhoea, and as such may not bring the desired therapeutic effect.
In most cases, the symptoms of dysmenorrhoea lead to changes in daily functioning, which can have a negative impact on the academic, professional, and social lives of affected women.
Despite the pain they experience during menstruation, most women do not consult a doctor or midwife, perhaps because they believe the symptoms appear naturally as part of menstruation. Furthermore, some symptoms declared by respondents suggest a secondary aetiology of dysmenorrhoea.
The early diagnosis of dysmenorrhoea is of key importance. Therefore, women who have menstrual pain and other accompanying symptoms during menstruations should be referred to experienced gynaecologists for differential diagnosis.