Mechanical small bowel ileus may have several causes. In this Letter to the Editor we would like to remind of its rare cause, i.e. the gallstone ileus – Bouveret’s syndrome, based on our case. Bouveret’s syndrome is a relatively rare variant of intestinal obstruction [1] caused by a gallstone migrating through the bilio-duodenal fistula. Proper treatment can be delayed due to the nonspecific symptoms, which may cause a considerable mortality [2, 3]. Radiological signs, known as Rigler’s triad for gallstone ileus, include pneumobilia, an ectopic gallstone, and small bowel obstruction. Imaging of the abdomen by plain X-rays or computer tomography (CT) is recommended [4]. The mainstay of management is surgical removal of the impacted stone [5].
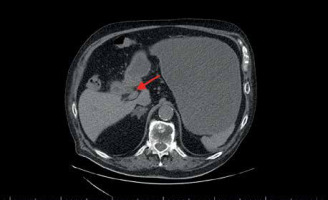
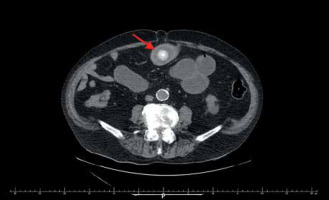
A 79-year-old man presented to the Emergency Department with a 5-day history of abdominal pain and persistent vomiting. His medical history included a type 2 diabetes mellitus, hypertension, cholecystolithiasis, and obesity. His initial laboratory evaluation revealed a high white blood cell count (15.3 × 103/µl) and elevated C-reactive protein (44.3 mg/l). The patient was referred for an abdominal CT scan, and radiological findings suggested a small bowel obstruction. CT showed a distended, liquid-filled stomach and the ectopic gallstone in the proximal jejunum, which appeared large and round (Figure 1). Proximal small bowel loops were liquid filled and dilatated and distally collapsed. In addition, the thickening of the gallbladder wall, pericholecystic fat stranding, pneumobilia, and bilio-duodenal fistula were visualized (Figure 2). The patient underwent an emergency surgery, and a 6-cm stone was successfully retrieved (Figure 3). The surgery and initial postoperative course have been uneventful.
Figure 1
Abdominal CT. The red arrow points to the ectopic gallstone in the first part of the duodenum
Bouveret’s syndrome is rare and represents less than 5% of all cases of gallstone ileus [6]. The common risk factors are female sex, older age, with frequent associated comorbidities, obesity, and gallstones size greater than 2.5 cm. Common clinical symptoms are abdominal pain, nausea, and vomiting. Rigler’s triad in radiologic examination are necessary to confirm the diagnosis. Although, there are no definitive guidelines on the approach and management of this condition, the most common is surgical treatment [7]. The tailored procedure must be considered individually, based on the patient’s condition and age. Moreover, optimal time of surgery and sometimes a restrictive surgical approach are crucial for satisfactory patient outcomes.