PURPOSE
Anti-N-methyl-D-aspartate receptor encephalitis (NMDA-R) is the most common among autoimmune encephalitis caused by antibodies developed against surface antigens [1-3]. It was first identified in 2007 as presenting with seizures, autonomic dysfunction, and movement disorders, in addition to acute or subacute onset neuropsychiatric symptoms [1, 3, 4]. Multifocal, nonspecific white matter lesions can be seen on cranial magnetic resonance imaging (MRI). Since paraneoplasia is usually found in the etiology, malignancy should be investigated in the patient with NMDA-R encephalitis [1, 2, 6].
CASE DESCRIPTION
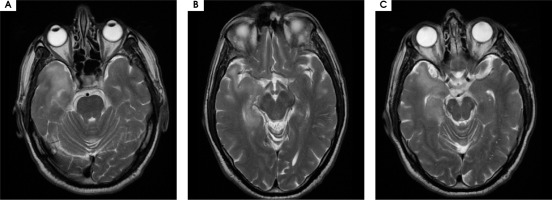
A 48-year-old male patient was admitted to the outpatient neurological clinic with complaints of numbness on the left side of his face, instability, spasms in all four extremities lasting for about 45 seconds, insomnia, and excessive talkativeness. In neurological examination, his general condition was good, he was conscious but showed psychomotor agitation, with difficulty concentrating and excessive talkativeness. He had dysarthria; his muscle strength and gait were normal. Sensory examination was normal, cerebellar examination was normal. Deep tendon reflexes (DTR) were normoactive in both upper and lower extremities, plantar response was flexor. There was no sign of meningeal irritation. In brain magnetic resonance imaging (MRI), an iso-hyperintense appearance was recorded in the hippocampus trace in the medial part of the right temporal lobe, and in the hyperintense ADC map in DWI. At this level, hyperintense cortical-subcortical and periventricular signal changes are accompanied on T2 images. Faint sulcal-like enhancements were observed. MRI findings were evaluated in favor of encephalitis (Figure I).
Figure I
Hyperintense signal changes in the right temporal lobe hippocampal region on brain MRI T2 sequence
The patient, who had no known disease, took no medication, suffered no trauma, and had no history of febrile illness, was admitted to the Neurology service for further examination and treatment.
On physical examination, his temperature was 36.6°C; he had blood pressure of 110/70 mmHg and heart rate of 107/minute; his respiration was 18/minute, with oxygen saturation at 96%.
Routine blood tests, biochemistry, whole blood, vitamin B12 tests, thyroid function tests, HbA1c, erythrocyte sedimentation rate, serum electrophoresis, autoantibody screening (antinuclear antibody, anti-SSA, anti-SSB, antithyroid antibodies, syphilis serology [fluorescent treponemal antibody]), Schirmer test, prothrombin time, INR, PTT, homocysteine, anticardiolipin, rheumatoid factor, protein C and S were normal. ELISA tests (hepatitis A, HIV, hepatitis B, hepatitis C) were negative. Complete urinalysis was within normal limits. When viral meningitis factors were investigated, none was found. HSV PCR and Brucella tests were negative. The pathergy test for Behçet’s disease was negative. In the electroencephalogram (EEG), a marked slowing of the background rhythm was detected. After the positive anti-NMDA receptor antibody was detected in the paraneoplastic panel studied in the cerebrospinal fluid (CSF), 1000 mg/day methylprednisolone treatment was started and completed in ten days. Levetiracetam 2 x 500 mg was also administered to treat seizures. No pathology was observed in the positron emission tomography taken after no positive findings were found in the thoracoabdominal tomography and scrotal ultrasonography requested for possible malignancy. The patient complained of no seizures during his follow-up examination. He benefited significantly from steroid therapy. In the neurological examination performed on the tenth day of treatment, he was conscious, oriented and cooperative. His speech fluency was, however, impaired and he could speak only falteringly. He showed full muscle strength in all extremities. The patient was discharged on the fifteenth day of hospitalization with 64 mg/day oral methylprednisolone. Prednisolone was discontinued in the second month of the patients examination during the follow-up, carried out outpatient clinic; the results of the neurological examination were normal.
DISCUSSION
Anti-NMDA receptor encephalitis is a type of autoimmune encephalitis caused by the development of IgG type antibodies against NMDA glutamate receptors. It was first identified in 2007 [1, 2]. The majority of patients are young females with ovarian teratoma, which is mostly associated with malignancy. In some studies found in the literature, it has been shown that the production of anti-NMDA receptor antibodies increases during the course of Herpes simplex encephalitis (HSE) and encephalitis occurs clinically. Psychiatric symptoms may occur. Imaging reveals findings only in 33% of cases [1, 2, 5, 6]. Showing hyperintensity in the hippocampus, cerebral-cerebellar cortex, frontobasal and insular areas, and brainstem elements in T2W and FLAIR sequences with mild meningeal enhancement. However, the only MRI finding with prognostic value is cerebellar atrophy which is an indicator of poor prognosis. Patients may show antibodies in the first cerebrospinal fluid study, or antibodies may be positive in recurrent CSF and serum studies [1, 2, 7-9]. EEG changes may be detected but the only EEG pattern specific to the disease is a superimposed fast activity in generalized rhythmic delta activity and which is called “extreme delta brush” [1, 3, 10, 11]. Corticosteroids, intravenous immunoglobulin (IVIG), plasmapheresis, cyclophosphamide and rituximab can be applied in the treatment of the disease. When malignancy is detected, an appropriate treatment for malignancy should be planned. The recovery rate is high when treatment is given, but untreated conditions can be fatal [2, 5, 6, 12].
COMMENT
Autoimmune encephalitis should be considered in patients with suspected autoimmune encephalitis, which takes severe clinical course and fails to respond to treatment adequately; NMDA receptor antibodies and other autoantibody tests should be requested, malignancy screening should be performed and treatment should be started in the early period.






