INTRODUCTION
According to the most significant Polish epidemiological survey, Epidemiology of Allergic Diseases in Poland (ECAP), allergic features are declared by up to 40% of the Polish population [1].
The most severe clinical picture of acute systemic hypersensitivity reactions is referred to as anaphylaxis. Potentially life-threatening severe anaphylaxis is characterized by acute respiratory symptoms – bronchoconstriction or laryngeal involvement and/or circulatory disturbances that require prompt medical intervention. It may occur without typical skin lesions [2–4]. The most common causes of anaphylaxis are food allergies (cow’s milk in infants, peanuts in children, and nuts and shellfish in adults), drug reactions, mainly caused by β-lactam antibiotics, non-steroidal anti-inflammatory drugs, and Hymenoptera venoms [5, 6].
The primary management of anaphylaxis is based on removing the potential causative agent and intramuscular administration of epinephrine in the anterolateral thigh. The steps described are essential to limit build-up of symptoms and protect the patient until medical help arrives. It is important to remember that anaphylaxis can occur anywhere but most commonly occurs in non-hospital settings, in outdoors or at home. Therefore, anyone with a history of severe allergic reactions should be provided with an epinephrine injector [3, 4].
According to the World Allergy Organisation (WAO), the incidence of anaphylaxis episodes oscillates between 80 and 210 cases per 1 million people per year, and in the world population, between 0.05% and 2.0% of people will experience an anaphylaxis episode at least once in their lifetime [6]. In the Polish population between 2008 and 2015, the rate of anaphylaxis cases, assessed based on NHF data, oscillated between 5.2 and 8.3 cases per 100,000 inhabitants per year [7]. The above data show the scale of the problem and highlight the role of public awareness and education to ensure the necessary management of anaphylaxis.
One of the groups that should have sufficient knowledge of anaphylaxis and be prepared to deal with this emergency is medical students (MS). In 2021, Leszkowicz et al. showed that knowledge of anaphylaxis among this group at one of Polish medical universities was inadequate [8]. Therefore, the present study aimed to conduct a survey among MS at the Medical University of Warsaw to assess knowledge of anaphylaxis management and whether additional training is required.
AIM
The study aimed to assess MS’ knowledge of anaphylaxis and management principles and how they evaluate their skills in this area.
MATERIAL AND METHODS
The study was based on a diagnostic survey method using a questionnaire of the authors’ own design, with the target group being MS of the Medical University of Warsaw. The online anonymous questionnaire contained 15 questions created based on the latest guidelines for the management of anaphylaxis from the European Academy of Allergy and Clinical Immunology (EAACI) and WAO [3, 4]. It ensured complete anonymity of respondents. It was distributed via social media (Facebook) and posted on MS groups to reach as many MS as possible from each year of study. The questionnaire was available for completion from February to March 2022. The study was approved by the Bioethics Committee of the Military Institute of Medicine (approval number 258/22).
The study group included 253 MS representing all years of study (1–6): 1st year n = 43 (17%), 2nd year n = 39 (15.4%), 3rd year n = 48 (19%), 4th year n = 40 (15.8%), 5th year n = 50 (19.8%) and 6th year n = 33 (13%). The questionnaire contained 15 single- and multiple-choice questions testing whether respondents were allergic or knew the definition of anaphylaxis, symptoms indicative of developing anaphylaxis, and its possible causes. Students were also asked to choose the best description of the actions they should take after noticing symptoms of anaphylaxis, the first-line medication for anaphylaxis, the route and site of its administration, and the dose for children and adults. Respondents also specified whether the dose of the first-line drug could be repeated. Other questions tested whether MS were aware that there are no absolute contraindications to administering the first-line drug in a life-threatening severe anaphylaxis and whether they were aware of what recommendations should be implemented in a patient at risk of developing it in the future. Students determined how they assessed their skills in the basic management of anaphylaxis and whether they thought that knowledge about it should be promoted more widely during university classes/in the community/by general practitioners, or another target group/in other ways.
STATISTICAL ANALYSIS
The data obtained were analysed using Excel and the statistical program Jamovi. Descriptive statistical analysis, Shapiro-Wilk, Leven, Mann-Whitney, Kruskal-Wallis ANOVA, and Dunn’s post-hoc tests were performed, and the rho-Spearman correlation coefficient was calculated. The significance level was taken as α = 0.05 (results p < 0.05 are considered statistically significant).
RESULTS
The responses showed that 34.8% (n = 88) of MS are allergic, 59.3% (n = 150) of respondents do not suffer from allergies, and 5.9% (n = 15) are not sure. The majority, 86.6% (n = 219) of respondents, correctly defined the term anaphylaxis as a severe systemic hypersensitivity reaction with a violent onset that is life-threatening. Three-quarters (75.5%; n = 191) of MS correctly marked symptoms that could indicate anaphylactic shock, i.e., shortness of breath, hives, nausea, hoarseness, and decreased blood pressure. As many as 24.5% (n = 62) of MS thought that symptoms such as increased blood pressure, fever, or dry skin and mucous membranes were highly likely to indicate anaphylactic shock. All MS correctly identified the possible causes of anaphylaxis (ingestion of milk, hen’s egg, nuts; taking an antibiotic, painkiller; sting by hymenopterous insects; administration of a contrast agent as part of an imaging study).
The vast majority (90.5%, n = 229) correctly identified which procedure to use in case of symptoms of anaphylaxis. They knew that the triggering agent should be removed, an ambulance should be called, the first-choice drug should be administered, the patient should be placed in a lying/semi-sitting position depending on the condition, and should be monitored. Almost all (97.2%; n = 246) MS were aware that the first-choice drug for anaphylaxis is epinephrine. Ninety-eight percent (n = 248) of respondents knew that epinephrine should be administered intramuscularly, and 95.7% (n = 242) correctly chose the administration site – in the anterolateral thigh.
More variation in responses was observed in the question about the dose of epinephrine in anaphylaxis. More than half (58.1%; n = 147) of respondents answered correctly, indicating the answer “children: 0.01 mg/kg, adults: 0.3–0.5 mg”. A significant proportion of students who correctly indicated the answer were fifth-year students (n = 41). Responses indicating incorrect dosages were marked by as many as 41.9% (n = 106) of respondents. When asked about the possibility of repeating doses of epinephrine in anaphylaxis, 79.4% (n = 201) of the students knew that if symptoms have not resolved, another dose may be given 5–15 min after the first one. Twenty point six percent (n = 52) of students were not aware of this.
Almost all (94.9%, n = 240) knew that there are no absolute contraindications to administering epinephrine in a life-threatening condition in anaphylaxis. A significant proportion (88.14%, n = 223) of MS correctly identified that all 3 of the recommendations listed in the question should be implemented in a patient at risk of anaphylaxis, i.e., referral to an allergy specialist to identify the allergen causing the allergic reaction, supplying the patient with a first-line drug and educating them on the principles of its self-administration, and on potential cofactors, i.e., factors that may promote the development of anaphylaxis.
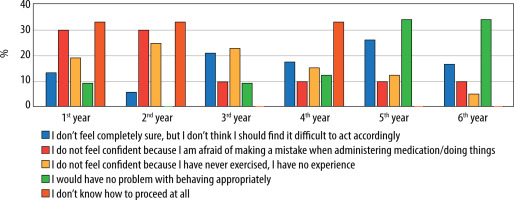
Only 12.6% (n = 32) of MS evaluated their ability to manage anaphylaxis well. These were primarily fifth- (n = 11) and sixth- (n = 11) year students. Forty-one point one percent (n = 104) of all did not feel confident because of a lack of experience and exercise in handling such situations. In this group, the majority were pre-clinical year students: 1st year (n = 20), 2nd year (n = 26), and 3rd year (n = 24). In contrast, 36% (n = 91) of all students felt they need more confidence but should not find it challenging to act appropriately, while 2.4% (n = 6) did not know how to proceed at all (Figure 1).
FIGURE 1
Distribution of medical students’ responses to the question, “How would you rate your skills in the basic management of anaphy- laxis?”
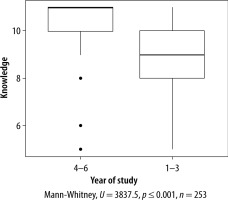
Eighty point two percent (n = 203) of the respondents believed that knowledge about anaphylaxis should be presented to students more widely or practiced in compulsory classes and promoted in the community via mass media. Sixty-six percent (n = 167) of the students thought it would be helpful if knowledge of anaphylaxis was also promoted to patients by their general practitioners. To assess MS’ knowledge of anaphylaxis management, each question testing knowledge was assigned 0 points (pts) if the respondent marked an incorrect answer and 1 point if the answer was correct. Pts were counted for each respondent. In the study group, the mean (M) value of the pts obtained by the students was 9.64 (SD = 1.445, min = 5, max = 11) out of 11 possible pts. Scores oscillated between 5 pts and 11 pts. In order to test whether there were differences in knowledge between students in pre-clinical years 1–3 and clinical years 4–6, the Mann-Whitney test was performed. The results of the test indicated that there was a significant difference in MS’ knowledge of anaphylaxis management depending on the year of study; U = 3837.5, p < 0.001, rrb (rank-biserial correlation coefficient) = –0.52, 95% CI [–0.62; –0.41], n = 253. The scores of students in years 4–6 (M = 10.31, SD = 1.001, Me = 11, IQR = 1) were found to be statistically significantly higher than those of students in pre-clinical years 1–3 (M = 9.01, SD = 1.517, Me = 9, IQR = 2) (p < 0.001) (Figure 2).
FIGURE 2
Differences between groups for the variable ‘Knowledge’ – distribution by the variable ‘Year of study’
It also examined whether students’ responses to the question about assessing their basic skills in anaphylaxis management correlated with their scores in the knowledge test (variable ‘knowledge’). The results of the rho-Spearman correlation analysis, which was performed, indicated a significant relationship between these variables, rho = 0.46, 95% CI [0.36, 0.56], p < 0.001, n = 253. The strength of the correlation was found to be very high and the direction of the correlation was positive. Students who rated their skills in AS management better scored higher on the knowledge test (Table 1).
TABLE 1
Results of rho-Spearman correlation analysis
| Variable 1 | Variable 2 | N | rho | 95% CI | P-value | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| How would you rate your ability to perform basic management of anaphylaxis | Knowledge | 253 | 0.46 | *** | 0.36 | 0.56 | < 0.001 |
The respondents’ answers to the question checking if they were allergic were compared with the number of pts they obtained in the knowledge test (variable ‘knowledge’). For this purpose, the Kruskal-Wallis ANOVA test was used. The results of the test indicated that there were significant differences in the students’ knowledge, considering the categorization of having or not having allergies, χ2 (2) = 8.89*, p = 0.012, ω2 rank = 0.04, 95% CI [0.00; 0.09], n = 253, but the strength of the observed effect was found to be small (Figure 3).
FIGURE 3
Differences between groups for the variable ‘Knowledge’ – distribution by the variable ‘Are you allergic’
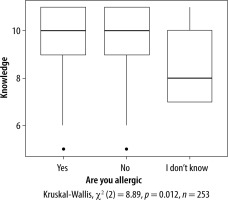
Dunn’s post-hoc test, with the Benjamini-Hochberg correction for multiple comparisons, was used to determine the significance of differences between pairs of groups, as mentioned earlier. The results of the test for the variable measuring students’ level of knowledge indicated that there were significant differences for the following pairs of categories: non-allergic students scored higher on the knowledge test than those who were unsure about their allergies (Z = –2.91, p = 0.004), and allergic respondents also scored higher than students who were unsure whether they were allergic (Z = 2.87, p = 0.004). However, allergic and non-allergic respondents had no statistically significant differences in knowledge (p = 0.932).
DISCUSSION
Almost 35% of MS surveyed claim to suffer from allergies. This result is in line with the results of the ECAP study, which showed that almost 40% of respondents declared experiencing allergic reactions [1].
Many MS appear to have a good basic knowledge on anaphylaxis, although there are areas where knowledge gaps exist. However, after tallying up the scores assigned to the individual survey questions, the average score for MS was high (9.64 out of 11 pts), the lowest score was 5 (less than 50%), and the highest was 11 (100%). Similar surveys conducted on MS indicate their less than perfect knowledge of anaphylaxis, which improved after the exercises implemented in the study [8, 9]. Analogous observations about the state of knowledge on anaphylaxis have been made by researchers assessing MS and those already in the medical profession [10–14].
The majority of respondents knew the correct definition of anaphylaxis, but 1 in 4 surveyed students was wrong about the indicative symptoms. In a study conducted in 2020 at the Medical University of Warsaw, Lange et al. found that 72% of surveyed nursing students and 28% of emergency medicine students knew the definition of anaphylaxis [15]. In a study conducted at the Medical University of Gdansk, Leszkowicz et al. found that 77.8% of MS knew what anaphylactic shock was, and 73.4% correctly identified its symptoms [8]. Wijekoon et al. surveyed MS at three universities in Sri Lanka, presenting clinical cases for resolution [10]. Out of 385 participants, only 7.3% made accurate diagnoses in all clinical cases, and 34.5% of the students correctly diagnosed all (7) cases of anaphylaxis. A study by Wang et al. tested the knowledge of Medscape users (including physicians, medical professionals, MS, and others) by giving four clinical cases for diagnosis [12]. Of all 7822 respondents, more than 80% correctly diagnosed a case with pronounced respiratory and skin changes as anaphylaxis, but only 55% knew that anaphylaxis could occur despite having no skin symptoms. Of the doctors surveyed, almost 50% correctly diagnosed anaphylaxis in the four presented cases. In contrast, in a Spanish study by Olabarri et al., more than 90% of 425 paediatric emergency care providers correctly diagnosed anaphylaxis [13]. However, more than two-thirds got it wrong in a patient with decreased blood pressure after ingestion of an unknown allergen, and almost 66% incorrectly diagnosed anaphylaxis in a patient with progressive urticaria and significant angioedema.
The possible causes of anaphylaxis and the basic regimen of actions to be performed when detected were known to the vast majority of MS in our study. Almost all the students surveyed knew that the first-choice drug in anaphylaxis is epinephrine (97.2%) and that it should be administered intramuscularly (98%) into the anterolateral thigh (95.7%). However, 4% of MS would administer the drug into the patient’s arm and 1.6% by the intravenous route. Similar results have been obtained by other researchers investigating the knowledge of students [10, 15, 16] as well as healthcare providers [12, 13]. However, in the study by Wijekoon et al., 9.9% of pre-interns in Sri Lanka would have administered epinephrine intravenously if they had been able to do so, which is significantly higher than in our survey [10]. Of the 1013 healthcare providers surveyed by González-Díaz et al., 75.2% correctly identified epinephrine as the first-choice drug, but only 56% knew that the preferred route of administration was intramuscular [11]. Similarly, an unsatisfactory result (66.9%) regarding the route of administration was obtained in a study conducted by Grossman et al. among 620 emergency physicians in the US [14]. In the Polish study by Leszkowicz et al., 67.9% of MS indicated epinephrine as their first-choice drug before training; this number increased to 95.7% after training [8]. The correct route of administration was chosen by 62.4% of Polish MS at baseline and as many as 96.5% after training.
Medical students’ knowledge of epinephrine doses for children and adults needs to be improved, with only 58.1% knowing the correct doses. A similar result was obtained by Wijekoon et al. [10], but other studies indicated that MS and doctors were more knowledgeable [13, 15, 17, 18]. In a Spanish study by Olabarri et al., one in 10 paediatric emergency care providers surveyed did not know the correct dose, site, and route of epinephrine administration, which is a significantly higher result [13]. Seventy-three point three percent of physicians surveyed in Singapore by Ibrahim et al. knew the correct dose of the first-choice drug; however, among nurses, the correct answer was given by 50% [18]. Worse results for questions about epinephrine dosage in anaphylaxis were obtained by González-Díaz et al.; 45.5% of 1013 study participants answered correctly [11]. Indian health providers had even worse knowledge in the Drupad et al. study, according to which 26.4% knew the epinephrine dose [19]. Also, in the study by Leszkowicz et al., 26.4% of MS knew the specific doses, although after participating in the training, as many as 86.7% answered correctly [8]. A poor result was obtained by Ozdemir et al., as only 19% of MS at one of the Turkish universities knew the maximum dose of epinephrine for children and adults [16]. However, their knowledge improved considerably after the training, rising to as much as 96%.
According to our survey, as many as 1 in 5 MS does not know that if anaphylaxis symptoms do not subside, epinephrine can be administered again 5–15 min after the first administration, and most of them believe that the drug can be administered only once. This knowledge was also tested by González-Díaz et al.; in their study, only 62.1% of healthcare providers surveyed knew that the interval between subsequent epinephrine doses was 5–10 min [11].
The majority of MS surveyed (94.9%) were aware that there are no absolute contraindications to the administration of epinephrine in the life-threatening condition of anaphylaxis. These results are consistent with the findings of Wijekoon et al., as, among the MS surveyed, 2–8% identified ischaemic heart disease, pregnancy, tachycardia, and hypertension as contraindications for epinephrine [10]. In our study, 3.6% of MS identified ischaemic heart disease as an absolute contraindication to the drug in anaphylaxis. However, in a study by Ozdemir et al., only 26% of MS had no gaps in knowledge of absolute contraindications to epinephrine use in anaphylactic shock [16].
Almost 90% of respondents knew that a patient at risk of anaphylaxis should be referred to an allergist for diagnosis, supplied with epinephrine for self-administration, and educated. Lange et al. made similar observations; 97% of nursing and 94% of emergency medicine students would recommend an autoinjector with epinephrine to a patient after an anaphylaxis episode [15]. Almost all emergency medicine physicians participating in the Grossman et al. survey in the US declared prescribing epinephrine autoinjectors to patients on discharge. However, only a proportion of them, 75% of those surveyed, gave the patient instructions for its use [14]. The same percentage of doctors referred these patients to an allergologist. Wijekoon et al. had different observations; only 50% of MS in the study declared arranging follow-up on discharge, and 27% of respondents wanted to prevent affected patients from having any contact with any trigger identified as an allergen [10].
One of the most critical questions asked respondents to rate their basic skills in anaphylaxis management. Unfortunately, only about 10% of MS declare to be fully ready to undertake the relevant actions, and a sizable proportion of respondents (77.1%) feel they need more confidence in the procedure because they have never practiced it and lack experience. This is why paying attention to developing MS’ skills in management of anaphylaxis and other emergencies during their studies is so important. In the study by Ozdemir et al., only 14% of pre-interns declared that they could diagnose and treat anaphylaxis. However, after the exercise conducted by the researchers, the participants’ confidence increased up to 83% [16]. It was thus similar to the original observations of Wijekoon et al., who found that almost 80% of MS were self-confident in diagnosing anaphylaxis. However, self-confidence in managing AS was declared by fewer (62.1%) [10]. The researchers found a positive correlation between knowledge, perception scores, and self-confidence. The same relationship was found in our study. MS who were more confident in their ability to manage anaphylaxis scored higher in the knowledge test (questionnaire). Nevertheless, a sizable proportion of students expressed the need to receive knowledge about anaphylaxis more extensively during their studies, including, in particular, practical exercises in the management of this condition. Such needs among nursing students were observed by researchers Noh and Lee in their study [20]. They found that the educational needs of the nursing students oscillated around four themes: the need to educate about anaphylaxis, implement this using different teaching methods, practice the knowledge gained, and repeat the exercises to consolidate the knowledge. Also, in a study by Lange et al., 80% of nursing students and 69% of paramedic students felt that the university does not spend enough time teaching about life-threatening conditions, including anaphylaxis [15].
The relevance of the exercises conducted for MS was demonstrated in the work of the researchers, who tested the knowledge of MS, conducted a training session, and then tested the participants’ knowledge again. In this way, in Leszkowicz et al. study students’ knowledge improved by an average of 28.6%, significantly increasing their confidence in their own skills in managing anaphylactic shock [8]. Almost all (99.4%) respondents declared after the training that they could use an epinephrine autoinjector in an emergency. Mawhirt et al. also noted a significant improvement in knowledge after the simulation exercise conducted for MS, and all participants agreed that the simulation was good for their education [9]. Therefore, the authors encourage institutions involved in training medical personnel to incorporate clinical simulations to make learning how to manage allergy-related life-threatening conditions much more effective.
As we suspected, after tallying up the scores for the answers to the questions and comparing the results of MS in the pre-clinical and clinical years, it turned out that the knowledge of the students in clinical years 4–6 was greater than that of the students in the pre-clinical years. Arguably, this is due to their more significant experience and ability to acquire more general medical knowledge throughout their years of study. Wijekoon et al. observed statistically significant differences in the mean scores of the anaphylaxis management knowledge test conducted among pre-interns from Sri Lanka [10]. Differences were based on the final MBBS results category (the higher MBBS results, the higher scores), the university, and the presence of a personal history of allergy (higher in students with a history of allergy). Statistical analysis of our questionnaire also indicates differences in the scores of allergic and non-allergic students. However, only those indicating higher knowledge of non-allergic and allergic students compared to students unsure whether they have allergies were statistically significant. Leszkowicz et al., on the other hand, found no statistically significant differences between the scores of allergic and non-allergic students [8]. However, they observed that higher test scores were associated with seeing anaphylactic shock before, which aligns with previously mentioned works.
LIMITATIONS AND STRENGTHS
The survey has some limitations. It was not validated. This was an online survey to test students’ knowledge, so it is possible that students did not answer only according to their knowledge but were assisted by information from available sources, which could have affected the results. However, even if such practices occurred, the survey still fulfilled its purpose: educating students. The survey group came from the Medical University of Warsaw. At the same time, the results could have been different if the survey had been carried out at another university as how classes are conducted may differ. Nevertheless, the questionnaire is an essential source of information about MS’ knowledge of anaphylaxis management, and its results and the need for more knowledge and practical exercises expressed by students draw attention to the need to refine the curriculum in terms of the aspects mentioned.
CONCLUSIONS
It is reassuring that most MS are aware of what anaphylaxis is and the basic management guidelines. However, many feel they need more confidence in their abilities in this area, which indicates a lack of sufficient practice. Students express the need to develop skills in coping with crises, such as anaphylaxis, as part of their mandatory coursework during their studies and to disseminate this knowledge widely in the community.







