INTRODUCTION
Angioedema is a frequently encountered condition in the emergency department (ED). Angioedema typically appears in areas where connective tissue is loose, such as the eyelids, lips, hands, feet, and the genital region. Swellings usually resolve within approximately 72 h [1]. Angioedema can present in three different endotypes based on the underlying pathogenesis: “histamine-mediated angioedema”, “bradykinin-mediated angioedema” and “idiopathic angioedema” [2]. Histamine-mediated angioedema typically occurs with urticaria or as part of an anaphylactic reaction. However, in isolated cases, angioedema may be mediated by either histamine or bradykinin mechanisms [3]. In the USA, there are over one million ED visits annually due to angioedema or allergic reactions. Around 110,000 cases are specifically coded as angioedema (either hereditary or acquired), while the remaining 979,400 cases are coded as allergic reactions [4]. The number of ED visits related to hereditary angioedema (HAE) in the USA ranges between 2280 and 5000 per year, with an estimated rate of 1.87 cases per 100,000 ED visits [5].
HAE is a rare disease with an autosomal dominant inheritance pattern characterized by recurrent angioedema attacks caused by excessive accumulation of bradykinin in the tissues [6]. Angioedema attacks can occur anywhere in the body. Still, the most typical affected areas, in frequency, are the extremities, gastrointestinal tract, oropharynx, face, and genital organs [7]. The most characteristic feature of these attacks is their lack of response to antihistamines, corticosteroids, and adrenaline, which are typically effective in histamine-mediated angioedema. This lack of response can be hazardous during an oropharyngeal attack, leading to asphyxiation and potentially fatal outcomes [6].
HAE affects both genders equally, and its prevalence is estimated at around 1 in 50,000 individuals. The onset of HAE attacks typically occurs after the age of two. By the age of ten, about 50% of patients may have experienced symptoms, and the symptoms tend to increase during puberty [3]. Even in developed countries, the average time to diagnosis from the onset of symptoms exceeds 6 years [8]. In a study conducted in Turkey, the delay in diagnosis was found to be 26 years [9]. Statistically, there should be between 1,534 to 7,669 individuals affected by the condition; however, the number of diseased patients is approximately 550 [10]. This significant delay is attributed to the condition’s rarity and health professionals’ lack of knowledge on this issue [8].
The rarity of HAE and its clinical symptoms resembling other types of angioedema can make diagnosing and managing the disease challenging. Data regarding emergency physicians’ knowledge of HAE is limited.
MATERIAL AND METHODS
STUDY DESIGN AND POPULATION
An electronic questionnaire was created using the Google Forms platform (Google Inc., San Francisco, USA). The survey was distributed through WhatsApp (WhatsApp Inc., Mountain View, CA, USA) and email and targeted emergency physicians in Turkey. The study was conducted between June 2023 and August 2023. The survey consisted of 10 questions developed by the authors and was conducted in Turkish. The English version of the questionnaire is provided in Supplementary. To prevent multiple submissions, the settings in Google Forms allow only one response per individual.
THE QUESTIONNAIRE INCLUDED THE FOLLOWING SECTIONS
Participants were asked to share information on their gender, academic degrees, years of work experience, and type of clinical setup (public hospital, university hospital, private hospital). At the end of this section, we asked the participants, “Have you heard of hereditary angioedema before?”. Participants who answered ‘Yes’ moved on to the second part of the study.
The second part included questions related to various aspects of HAE, such as symptomatology, natural history, diagnostic workup, and triggers of attacks. Single-choice and multiple-choice questions were used. Additionally, a ‘I do not know’ option was provided for each question.
STATISTICAL ANALYSIS
All data were transformed into an electronic Microsoft Excel spreadsheet. Categorical and ordinal variables were presented using frequency distribution, and proportions were compared using the χ2 test. Continuous variables were presented as median with IQR. All analyses were conducted using the SPSS statistical package (ver. 22.0; IBM Corp., Armonk, NY, USA). A p-value < 0.05 was considered statistically significant.
This study was approved by the local ethics committee of Necmettin Erbakan University Medical Faculty Hospital (approval number 2023/4223), and all study participants provided informed consent.
RESULTS
A total of 344 emergency physicians participated in the study. Two physicians who stated they had not heard of HAE were excluded from the study. The median post-graduate employment period was 6 years (IQR, 2–12 years), and 204 (59%) physicians were male. Of the physicians participating in the study, 152 (44.4%) were specialists, 110 (32.2%) were general practitioners, 64 (18.7%) were research assistants, 10 (2.9%) were lecturers, and 6 (1.8%) were associate professors. The distribution by hospital types was as follows: 178 (52%) worked in education and research hospitals, 114 (33.3%) worked in public hospitals, 32 (9.4%) worked in university hospitals, and 18 (5.3%) worked in private hospitals. While 96 (28.1%) had an Allergy and Immunology (A/I) clinic in their institution, 246 (71.9%) did not have any Allergy and Immunology (NA/I) clinic (Table 1).
TABLE 1
Demographic characteristics of emergency physicians who responded to the questionnaire
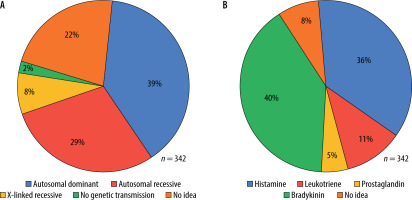
Regarding the inheritance pattern of HAE, 38.6% (n = 132) of the participants said that the disease has an autosomal dominant inheritance pattern, while 22.2% (n = 76) had no idea (Figure 1 A). While 40.4% (n = 138) of the participants correctly answered the question about the pathogenesis of the disease, 52% (n = 178) thought that the condition was due to causes unrelated to the pathogenesis of HAE (Figure 1 B).
FIGURE 1
A – ‘’What is the pattern of inheritance of HAE?’’ percentage of physicians responses. B – ‘’Which of the following is the mediator responsible for the clinical findings of HAE?’’ percentage of physicians responses
When asked about the symptoms seen in HAE, 38 (11.1%) physicians got all the answers correct. Among the incorrect answers, 158 (46.2%) chose ‘itching’, 168 (49.1%) ‘urticaria’, and 42 (12.3%) ‘fever’. The number of correct answers for all the options related to diagnosis and diagnostic workup was 20 (5.8%). Among the incorrect answers, 72 (21.1%) chose ‘complement C3’, 48 (14%) ‘total IgE’, 18 (5.3%) ‘skin prick tests’, and 14 (4.1%) ‘food specific IgE’.
The number of physicians who got all the answers about attack triggers correct was 14 (4.1%). The incorrect answer, ‘contact with allergen’, was chosen by 230 (67.3%) physicians. Twenty-six physicians (7.6%) had no idea. Only 6 (1.8%) physicians knew all the answers for managing acute attacks correctly. Among the incorrect answers, 224 (65.5%) chose ‘systemic corticosteroids’, 206 (60.2%) ‘antihistamines’, 160 (46.8%) ‘adrenaline’, 32 (9.4%) ‘danazol’, and 14 (4.1%) ‘ tranexamic acid’ (Table 2).
TABLE 2
Answers of emergency department physicians on heredi- tary angioedema
The number of physicians who considered HAE in the differential diagnosis and requested a serum C4 level to be measured in patients presenting with abdominal pain symptoms was 14 (4.1%), while this number was 36 (10.5%) in patients presenting with laryngeal edema.
When a patient known to have HAE is presented to the ED with laryngeal edema, the number of physicians who answered ‘C1 esterase inhibitor’ as the first drug treatment was 102 (30%). Among the wrong answers, 180 (52%) chose ‘adrenaline’, 28 (8%) ‘systemic corticosteroids’, and 16 (5%) ‘antihistamine’.
Physicians working in hospitals with allergy clinics were more aware of the HAE diagnosis (10.4% vs. 4.1%, p = 0.024). Physicians in hospitals with allergy clinics were more likely to consider HAE as a diagnosis for abdominal pain and laryngeal edema, and their rate of requesting a serum C4 level to be measured was higher than those who did not have an allergy clinic in their hospital (p = 0.013, p < 0.001, respectively) (Table 3).
TABLE 3
Physicians’ approach to HAE patient management
DISCUSSION
The rarity of HAE, similarity of symptoms with other diseases, and incomplete understanding of its pathophysiology by physicians cause a delay in diagnosis even in developed countries. This study was conducted using an electronic questionnaire to evaluate the level of knowledge of emergency physicians about HAE. The findings revealed a prevalent lack of information, particularly regarding the diagnosis of HAE and the effective management of acute attacks among emergency physicians. Many survey studies on HAE awareness among physicians exist in the literature [8, 11–14]. However, to the best of our knowledge, no specific study was conducted, especially among emergency physicians. This is the first study conducted in this field.
HAE has an autosomal dominant genetic inheritance. Screening first-degree relatives of a diseased patient is an effective method to identify more potential patients. This informed approach allows more people to be diagnosed with HAE with the index case [15]. In this study, 38.6% of the participants knew that HAE was inherited as autosomal dominant. This low rate may lead to low awareness of family screening, which may cause delays in diagnosis [16]. Bradykinin is the main mediator responsible for angioedema in HAE and is a small, vasoactive nonapeptide with a short half-life [17]. In this study, 40% of the emergency physicians identified bradykinin, while 36% identified histamine as the causative mediator. These different opinions among physicians may prevent accurate diagnosis and effective treatment of HAE.
Patients with HAE typically present with attacks of non-pruritic, non-marking edema involving the skin (extremities), genitourinary tract, abdomen, face, or oropharynx. More than half of patients have at least one laryngeal attack [18]. In this study, only 38 (11.1%) participating physicians identified all symptoms correctly. Physicians were more aware of edema-related facial, tongue, extremities, and larynx symptoms. Interestingly, a significant portion of the participants selected “pruritus” and “urticaria”, which are, in fact, symptoms of histamine-mediated angioedema. Regarding HAE triggers, 230 (67.3%) of the physicians gave the wrong answer and chose ‘contact with the allergen’. This high rate indicates that physicians could not differentiate between histaminergic and bradykinin-induced angioedema in a case presenting with angioedema. The number of physicians who knew all triggers correctly was 14 (4.1%).
To diagnose HAE, a complement C4 level, C1-INH antigenic level, and C1-INH functional level should be measured. In HAE, the C4 level decreases by almost 100% during angioedema attacks, while at least 95% show a decrease even between attacks [7, 19]. In the current study, the number of participants who marked the correct answers about the diagnostic HAE was as follows: 144 (42.1%) for ‘serum C4 levels’, 252 (73.7%) for ‘C1 esterase inhibitor’, and 132 (38.6%) for ‘C1 esterase function’. Only 20 (5.8%) physicians knew all the correct answers. When asked whether they had previously considered HAE in a patient presenting with episodes of abdominal pain and laryngeal edema and ordered a serum C4 test, only 4% and 11% of physicians answered “yes”, respectively. These low rates suggest that many physicians do not know the serum C4 level, which is widely available in many health centers and plays an essential role in diagnosing the disease.
Unlike histamine-mediated angioedema, bradykinin-mediated angioedema attacks in HAE do not respond to adrenaline, antihistamines, or corticosteroids. First-line attack treatment consists of C1-INH replacement therapy and therapies that suppress the production or function of bradykinin [3, 20]. Fresh frozen plasma (FFP) may be a second-line treatment option in attacks if none of the first-line therapies are available [20]. In our study, a list of agents that can be used in the treatment of angioedema was presented to emergency physicians. Physicians were asked to indicate which agents were preferred in treating HAE attacks. 68.4% of physicians selected C1 esterase inhibitor, 11.7% icatibant, and 40.4% FFP. The number of physicians who answered all of them correctly was only 6 (1.8%). More than half of our study’s physicians chose the wrong treatment option and ticked systemic corticosteroids, antihistamines, and adrenaline. In line with these data, it was revealed that physicians did not have sufficient knowledge on treating HAE attacks.
Huang et al. [21] reported that approximately 25% of patients with HAE were treated in the ED with a diagnosis of anaphylaxis. Laryngeal edema is the most feared involvement in HAE, which can be fatal. In a series of 221 patients, laryngeal edema was found in less than 1% of all attacks recorded [18]. Mortality due to laryngeal edema is more than 30% in undiagnosed patients, while this rate is around 1% in diagnosed patients [22]. To the question, “When a patient known to have HAE comes to the ED with acute laryngeal edema, what is the first treatment administered?” 52% of the physicians answered adrenaline. Only 30% of physicians chose C1 esterase inhibitor. A United Kingdom ED study showed that most drugs used to treat bradykinin-mediated angioedema are available in hospitals with allergy clinics. Still, these drugs were not easily accessible in ED. Furthermore, only half of the hospitals analyzed had guidelines for using these medicines [23]. Lack of protocols and access to medicines can lead to treatment errors and poor outcomes in patients presenting with HAE. Beyond the availability of C1 esterase inhibitors in the hospital, emergency physicians’ knowledge of managing an HAE attack and appropriate use of C1-INH is critical to prevent morbidity and mortality.
To evaluate the effect of hospitals with allergy clinics on HAE awareness, we asked physicians about the presence of allergy clinics in the institution where they worked. Our study found that physicians working in institutions with allergy clinics were more aware than those working in institutions without, especially in diagnosing HAE. This difference may be attributed to allergists offering inter-clinical training and having greater access to diagnostic parameters.
This study had several limitations. One of the limitations of our study is that we did not use a standardized and validated questionnaire because no such questionnaire was available at the time. However, a questionnaire with similar questions used in HAE awareness studies was used, and a working group with experience in HAE prepared this questionnaire. Another limitation was the relatively low response rate from the invited physicians, with only a small proportion (11.4%) providing responses.
CONCLUSIONS
This study shows that emergency physicians recognize HAE but do not fully differentiate it from histaminergic angioedema. Early diagnosis and effective treatment are critical to improving quality of life and preventing potentially fatal attacks. Although HAE is a rare disease, most emergency physicians will likely encounter HAE attacks at some point in their careers. Therefore, it is necessary to increase awareness among emergency physicians to intervene rapidly and correctly in HAE attacks.






