INTRODUCTION
Electrodiagnostic (EDX) testing, including nerve conduction studies (NCS) and electromyography (EMG) is the most important diagnostic procedure in diagnosis and follow-up evaluation of the patients with neuromuscular disorders. It should be considered as an extension of clinical neurological examination [1], but not performed instead. The role of EDX is to confirm the initial diagnosis, which was set on the basis of detailed interview and neurological examination by referring physician. EDX is an expensive, difficult and individualized test and as a rater dependent technique requires an experienced electromyographer. Additionally, information about patients medical history, clinical examination and initial diagnosis is invaluable in planning and conducting EDX tests. Thus, the accuracy and diagnostic utility of EDX testing is directly correlated to the appropriate clinical referral diagnosis [2]. Currently, diagnostic procedures, including EDX tests, are overused and misused in the attempt to substitute for the detailed clinical examination [2]. This often leads to the unnecessary diagnostic procedures, which makes the waiting list longer and increases costs for the health funds. Moreover, EDX tests are unpleasant and cause discomfort for the patients.
Like other centers, over time we observed continuous increase in the number of patients referred to our EMG lab [3]. Hence, it is important to analyze if the decision to refer patients to EDX examination is thought-through and examination confirms referral diagnosis.
The aim of this study was to evaluate the type and the concordance of the referral and EMG diagnosis among various referring physicians specialties to our EMG lab from outpatients clinics.
METHODS
This prospective study was carried out in EMG lab located in Institute of Psychiatry and Neurology in Warsaw, Poland. We prospectively collected data about consecutive patients referred to our EMG lab between January 2021 and December 2021 from 14 outpatient medical care facilities. Doctors referring to our EMG lab were mostly neurologists, but also orthopedists, residence doctors, neurosurgeons or internal medicine doctors.
EDX examination was performed using Nicolet EDX Viking (Natus Neurology Inc./Nicolet Biomedical Inc., USA). EMG examination protocol differed according to the referral diagnosis and included sensory and motor nerve conduction (NCS), F wave analysis, electromyography (EMG), repetitive nerve conduction studies (RNS) or single fiber EMG (SFEMG), as appropriate.
The aim of the study was to analyze consistency of the initial diagnosis with EDX test outcome as well as to check whether the specialization of the referring physician had an impact on accuracy of the diagnosis. Finally, we verified if the patients were informed by their doctors about the manner of execution and purpose of EDX tests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by local Ethics Committee.
Statistical analysis
Calculations were carried out using Statistica v.12 (Stat Soft Inc. 2011, Tulsa, OK, USA). Data are presented as number with percentage or mean with standard deviation (SD) or range. Results were analyzed by means of the χ2 test. A p-value < 0.05 was considered statistically significant.
RESULTS
During one year period 454 EDX examinations were performed in 412 patients. There were 26.9% males and 73.1% of females. The age range at the time of the examination was 19-89 years, mean 55.9 ± 14.4 years.
Most patients were referred by neurologists (71.6%), less frequently by orthopedics (16.8%), residence doctors (6.7%), neurosurgeons (3.9%), and least frequently by internal medicine doctors (1%). Mean time between visit to the referring physician and EDX examination was 101.2 ± 57.9 days.
Most of the patients (54.6%) were referred with the diagnosis of carpal tunnel syndrome (CTS), others with diagnosis mononeuropathy or single nerves damage (18.7%), suspicion of polyneuropathy (18.1%), tetany (7.0%), myasthenia gravis (1.3%) or myopathy (0.2%).
Most patients were referred with one diagnosis but some had two clinical diagnoses.
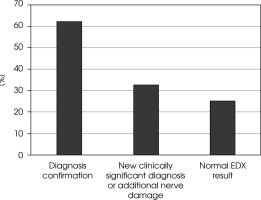
ENG/EMG examination revealed: confirmation of the initial diagnosis in 61.9% of patients, a new clinically significant diagnosis or finding additional, asymptomatic nerve damage in 32.4%, and a normal examination result in 25.1% of patients (Figure I).
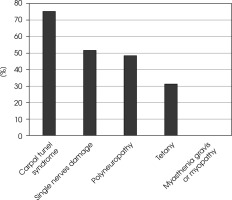
Electrophysiological examination most often confirmed the referral diagnosis in patients with CTS (75.4%), less often when examining single nerves (51.8%), polyneuropathy (48.8%), tetany (31.3%) and the least for myasthenia gravis and myopathy (0%) (Figure II).
The percentage of correct diagnoses was not significantly higher (p > 0.05) in the group of patients referred by neurologists compared to other specialties (CTS 78.1% vs. 76.6%, polyneuropathy or myopathy 49.4% vs. 0%, single nerves damage 46% vs. 56.3%, respectively). Patients with diagnosis of myasthenia gravis were referred only by neurologists and only 2 patients were referred with diagnosis of tetany by other physicians than neurologists with the diagnosis accuracy of 50%. Generally, neurologists more often formed improper clinical diagnosis before EDX examination when compared to other medical specialties (p = 0.048).
Moreover 83.2% of patients referred to EDX test were not informed about the character of the procedure. Patients referred with suspected tetany were most frequently informed about the examination procedure (53.9%), followed by mononeuropathies other than CTS (20.1%), CTS (11.6%) and polyneuropathy (11.3%). Interestingly none of patients referred with myasthenia were informed about procedure.
DISCUSSION
The availability of EDX examinations is increasing and patients are more frequently referred for this examination. However, there is still not enough data on the quality of referrals for these tests. As they are considered to be cost generating and time-consuming, hence decision to refer the patient for this examination should be justified and referral should be carefully planned and formulated.
In our study patients were most frequently referred with clinical diagnosis of CTS (54.6%) which is consistent with some other authors who reported CTS diagnosis in Mondelli et al. [4] study (54%). Other authors reported that most common referral diagnosis was polyneuropathy or radiculopathy [3, 5]. Those discrepancies may result from the scope of the dominating specialty of the referring physicians.
The result of the ENG/EMG examination in our cohort was confirmation of the diagnosis in ~62% and a new clinically significant diagnosis in 32.4%. Reports of Perry et al. [6] stay in concordance with our findings. Authors analyzed the EMG findings of 98 inpatients. The study confirmed the clinical diagnosis in 53.3% of the patients, provided a new diagnosis in 12.6% and was inconclusive in 16.8% and normal in only 3.0%. However, in this study only neurologists referred for EDX tests. Authors explained those findings by the fact that neurologists are more familiar with neurologic symptoms and signs, hence their clinical diagnosis is more likely to be correct. Additionally, inpatients, especially in neurology departments of university, usually suffer from unusual and difficult neurological diseases and disorders with neuromuscular system involvement. However, this was not confirmed by our study as diagnosis confirmation was less frequent in patients referred by neurologists. On the other hand neurologists referred much more frequently to our center than other specialties. Hence, decision about referring and referral diagnosis could have been more thought-through when patients were referred by other specialties than neurologists.
We did not find significant differences in correct initial diagnosis formed by referring physician and its confirmation by EDX between neurologists and other medical specialties. Other authors suggest that those are neurologists who more frequently refer for EDX with abnormal EDX result (58.9%) when compared to orthopedics (47.3%) [5].
In our cohort ~25% of patients had normal EDX examination results, which is concordant with large study presenting results from seven European EMG laboratories in which the percentage ranged from 16% to 33% [7]. However, some other studies reported normal or inconcensive EDX tests in up to 55% of patients [2, 5, 8]. The high proportion of normal EDX tests in those studies denotes the need for more careful examination and accurate clinical diagnosis in order to reduce the time spent and resources. We should also consider reducing patient discomfort related to EDX study. Moreover, physicians, especially those at the state social insurances, have not enough time for the detailed history taking and clinical examination due to the large number of patients they examine in a very limited time. Besides, many physicians are not familiar with EDX tests and their limitations. On the other hand, it is possible that in the countries where accessibility to EDX tests is better, physicians tend to refer their patients to EMG lab even if the damage of peripheral nerves or muscles is less probable. This may also be the case with the referrals of our patients. On the other hand normal EDX result may also be clinically beneficial as it may exclude peripheral nerves damage and direct diagnostics to other possible causes of symptoms.
It is worth noting, that the sensitivity of EDX tests is not 100%. This is the case for mononeuropathies, polyneuropathies (especially in very old patients where the normal limits are not well defined) and even for myasthenia gravis tests. There are a number of factors that should be considered when interpreting the EDX test results, such as age [9], skin temperature [10, 11], skin thickness [12], height [13] or even gender [14, 15]. However, in our laboratory we make every effort to ensure the highest quality of EDX tests and always care about fighting possible pitfalls of EDX tests such as low temperature of the limbs.
In our study, diagnosis of CTS was slightly more frequently confirmed when patients were referred by neurologists compared to other medical specialties but less frequently when patients were referred with suspected single nerves damage. This inconsistency may be explained by the fact that neurologists referring patients to our center are not neuromuscular neurologists. Other studies suggests that EDX examination confirms referral diagnosis more often when patients are referred by neuromuscular neurologists than other neurologists [3]. However, neurologists tend to formulate clinical diagnosis more often when compared to other specialties. In the study of Nardin et al. [16] the electrophysiological diagnosis was unsuspected in 28% of the cases when the referring physician was a neurologist and in 42% for non-neurologists.
According to our study vast majority of the patients (~82%) were not informed about the EDX procedure beforehand by their physician. This led to unnecessary additional stress for patients, who found false information about EDX tests from not professionals, before they were referred to our EMG laboratory. From an ethical point of view this is unfair [17]. The reason may be incomplete or lack of knowledge about EDX tests, but also lack of time of referring physicians and limited access to the doctors during the COVID-19 pandemic (some consultations were remote in the form of teleconsultations with no possibility of examining the patient). Some authors reported that 52.1% of patients received either no information about EDX test or the information they received was very poor and incorrect [4]. Other authors reported that even 92% of patients did not receive information about the test and also 92% of patients were not instructed about any precautions to be taken by referring physicians [18]. Importantly, those studies were carried out before the covid-19 pandemic.
Finally, in our cohort there was a significant predominance of women (72%). This is consistent with some reports (58.8-61.5%) [4, 5]. A possible explanation is that men are more reluctant to go to the doctor and would rather do household chores. On the other hand other authors from Pakistan examined men more often (65.4%) [18].
LIMITATIONS OF THE STUDY
Our study has some limitations. Firstly, it was a single center, which may limit generalizability of our results for the whole country. Secondly, we analyzed examinations provided in the era of COVID-19 infection, which may also differs from the standard access to doctors and additional examinations as well as proper information about the purpose and the manner of execution of EDX tests.
CONCLUSIONS
Our study showed inconsistency of the EDX results with the clinical diagnosis formulated by the referring physician in a large number of patients. In addition, a significant percentage of correct EDX test results is noteworthy. The decision on the scope of the examination and clinical suspicion in patients referred for ENG/EMG examination should be preceded by a detailed and careful interview and physical examination. This would save patients suffering, costs in the health system and time for doctors performing EDX tests.