Introduction
Paediatric ingestions are common, especially those under 5 years old [1]. Children at this age tend to explore objects by placing them in their mouths.
The extent of the problem is believed to be underestimated, as many ingestions are either not recognised or are managed without seeking medical attention [2, 3].
Accidental foreign body ingestion comprises most such incidents. Foreign bodies in the gastrointestinal tract cause significant morbidity and may even cause death [1]. Coins are the most commonly ingested foreign bodies worldwide. Toys represent a rich source of foreign bodies (toy pieces, disc batteries, and small magnets). Specific cultural/nutritional habits may influence the type of ingested foreign body (pins, fish bones, etc.) [4, 5].
Although most ingested foreign bodies will traverse the gastrointestinal tract uneventfully, some will lodge at natural narrowing points (upper, middle, and lower oesophagus, pylorus, ileocecal valve, and rectosigmoid junction) or at sites of narrowing caused by disease (oesophageal stricture, eosinophilic oesophagitis, inflammatory bowel disease, etc.). Food boluses lodged in a stricture can resemble foreign body ingestion.
Despite the available management guidelines [6] on foreign body ingestion, decisions depend widely on the expertise of the managing physician. Endoscopic management of foreign body ingestion is increasingly popular. Flexible endoscopy enables direct visualisation and handling of the foreign body, and the gastrointestinal tract can be examined for underlying disease or complications of the ingestion [1].
Aim
This study aimed to analyse the clinical presentation, aetiology, and outcome in children presenting with foreign body ingestion, who required endoscopic intervention at our tertiary hospital (King Abdullah University Hospital, Irbid, Jordan).
Material and methods
The files of all children with ingested foreign bodies that required endoscopic retrieval at our hospital over a 3-year period were reviewed retrospectively. Data on age, sex, type of ingested foreign body, presentation, investigations (X-rays and histopathology if done), type of intervention, site of lodging and site of retrieval, and compilations were collected. Statistical analysis was performed using a complementary-descriptive method. Categorical variables were expressed as percentage (%) values.
The research was approved by both the institutional review board at the faculty of Medicine in Jordan University of Science and Technology (32/117/2018) and the University Research Committee.
Results
Of 63 patients identified, 32 (50.8%) were males. Mean patient age was 7.7 ±3.4 years (1 month–17.4 years), and 16 (25.4%) were younger than 5 years old (Table I).
Table I
Patients’ demographics
| Parameter | Value |
|---|---|
| Age | < 5 years – 16 (25.4%) > 5 years – 47 (74.6%) |
| Gender | Male – 32 (50.8%) Female – 31 (49.2%) |
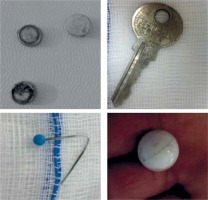
Most patients (74.6%) presented with no symptoms after the family or the child reported the ingestion, followed by drooling and difficulty in swallowing (Table II). Coins were the most common foreign body retrieved (37, 58.7%). (Tables III and IV, Figure 1).
Table II
Presenting complaint
| Complaint | Number (%) |
|---|---|
| Asymptomatic (reported by the family or the child) | 47 (74.6) |
| Accidental finding | 1 (0.48) |
| Choking | 3 (4.8) |
| Drooling/difficulty in swallowing | 9 (14.2) |
| Vomiting | 3 (4.8) |
Table III
Types of foreign bodies ingested
| Type | Number (%) |
|---|---|
| Coins | 37 (58.7) |
| Pin | 3 (4.8) |
| Batteries | 2 (3.2) |
| Fruit seed, food bolus | 8 (12.7) |
| Paper clip, metallic piece, earring | 7 (11.1) |
| Key | 1 (1.6) |
| Marble, plastic ball | 3 (4.8) |
| Plastic tube | 1 (1.6) |
| Magnet | 1 (1.6) |
Table IV
Sites of foreign body on endoscopy
| Site | Number (%) |
|---|---|
| Upper oesophagus | 26 (41.2) |
| Mid oesophagus | 15 (23.8) |
| Lower oesophagus | 4 (6.3) |
| Stomach | 16 (25.4) |
| Not found | 2 (3.2) |
The oesophagus was the most common site of retrieval (45, 71%). A rat tooth forceps was most commonly used to retrieve coins, followed by a net basket. Endoscopy was effective in treating 57 (90.5%) patients, whether through retrieval of the foreign body or by pushing it into the stomach in case of food lodged in the oesophagus. Surgery was needed in 1 (1.6%) patient, a 1-month-old infant with a plastic tube in his stomach. All patients tolerated the procedure well with no complications.
Discussion
Foreign body ingestion represents a relatively common problem in young children. While younger children tend to explore reachable objects by mouth, older ones tend to accidentally ingest such nonedible objects while playing. Historically, rigid scopes were used to retrieve objects lodged in the oesophagus. With widespread availability and experience with fibre-optic scopes, endoscopic management of foreign body ingestion has gained popularity [1, 6]. This study described the experience of our centre in the endoscopic management of foreign body ingestion.
In our study, 63 patients with foreign body ingestion required endoscopic intervention. The literature reports that children below the age of 5 years are most affected by ingestion [7–9]. In our cohort, affected children were older. This might reflect referral bias rather than a different epidemiology.
Foreign body ingestion has no sex predilection. Previous reports showed an equal distribution between males and females. In our study, almost equal numbers of males and females required endoscopic intervention for foreign body ingestion, consistent with the literature [10–13].
Common objects ingested by children are coins, batteries, toys, magnets, food pieces, and jewellery. Coins represented the most common foreign body lodged in the oesophagus. In our cohort, 37 (58.7%) of the ingested foreign bodies were coins. This is consistent with the literature [9–12, 14]. Interestingly, pins were retrieved from 3 patients. In two, the pins were held in the mouth to fix a headscarf and were suddenly swallowed. Disc batteries represent a growing concern [6]. Our numbers are lower than other reports [9, 15]; this might reflect the underuse of electronic devices with button batteries by Jordanian children rather than high awareness of the ingestion risk. The recommendations of the NASPGHAN were challenged recently at the Digestive Disease Week (DDW) [16] as the damage to the stomach lining might occur early and without symptoms. Despite compliance with the NASPGHAN recommendations dealing with batteries, still we found a small ulcer in the stomach at the site of the lodged battery. The timing of endoscopy was determined according to the NASPGHAN recommendations; 30 (47.6%) were done on an emergency basis (symptomatic oesophageal foreign bodies, sharp objects, batteries and one magnet). One more indication was extreme family anxiety in 3 patients.
Most children had a normal gastrointestinal tract. However, abnormal anatomy such as a stricture might lead to a foreign body lodging in the oesophagus. In our cohort, 7 children showed endoscopic features of eosinophilic oesophagitis, and 3 were confirmed with histopathological features. Two presented more than once. Taking biopsies may be wise, especially if endoscopic findings suggest the need or because of repeated presentation [17]. On the other hand, 2 patients had the foreign bodies at the site of oesophageal strictures; one after corrosive ingestion, the second at the anastomosis site of oesophageal atresia operation.
It is well known that most children with foreign body ingestion present with nonspecific symptoms, and nearly 50% are asymptomatic [18]. Most of our patients were asymptomatic and were brought to hospital directly either after witnessing the ingestion or it having been reported by the child.
In our study, most of the ingested objects lodged in the oesophagus, with 50% in the upper oesophagus. This is consistent with previous reports in which the cervical oesophagus was the most common site of foreign body lodgement secondary to the natural narrowing [8, 19–22].
Although endoscopic removal of a foreign body is ideally performed under general anaesthesia with endotracheal intubation, only 3 patients in our cohort underwent endoscopy under these conditions. Endoscopy was performed in our gastrointestinal unit. Most patients required local lidocaine and midazolam with or without ketamine. All children in our cohort tolerated the procedure well with no complications. However, this study does not recommend endoscopic retrieval of foreign bodies under sedation. The authors encourage complying with the NASPGHAN recommendation [6] to do such procedures under general anaesthesia, while the patient is intubated to protect the airway.
Foreign bodies were either removed with appropriate endoscopic tools (forceps, basket, etc.) or pushed into the stomach (in case of a lodged food bolus). Endoscopic management was successful in 57 (90.5%) cases. In the remaining cases, either the foreign body had already passed the duodenum at the time of endoscopy, or it was not feasible to remove, as in the case of a premature neonate with a plastic tube in the stomach. This unfortunate baby had respiratory distress in our NICU, for which he had a unit-customised nasopharyngeal airway using small nasogastric tubes. One of the tube limbs slipped into the stomach. This ended up being removed through open gastrostomy.
Conclusions
Endoscopic intervention is safe and effective in retrieving foreign bodies lodged in the upper gastrointestinal tract. Early intervention might prevent complications and alleviate parental anxiety. Because coins are the most commonly ingested foreign body, addressing this issue by raising awareness will certainly reduce the magnitude of the problem.