Introduction
Upper gastrointestinal bleeding (UGIB) is common in liver cirrhosis patients and accounts for 25% of mortality in this patient population [1]. The total annual hospitalizations due to gastrointestinal bleeding in the United States amounts to 1,000,000, with an estimated 2–10% mortality rate [2, 3]. Out of these admissions, 40% are from upper gastrointestinal bleeding [4]. Non-variceal upper gastrointestinal bleeding (NVUGIB) in cirrhotic patients is common, and studies have shown increased incidence and prevalence of peptic ulcer bleeding in cirrhosis [5]. UGIB in cirrhosis patients harbours greater mortality compared to patients who do not have cirrhosis [6]. UGIB also drives higher health resource utilization, including healthcare costs and length of stay (LOS), in patients with cirrhosis [7].
Aim
Our study aimed to understand the association of NVUGIB in cirrhosis patients and hospital-based outcomes in this subset of patients. Moreover, we also reported the impact of various patient characteristics and comorbidities acting as predictors of mortality.
Material and methods
Study design and database description
This is a retrospective study of adult patients hospitalized due to NVUGIB. The joint releases of the year 2016 through 2018 of the Nationwide Inpatient Sample (NIS) database were utilized. It is designed as a stratified probability sample to be representative of all non-federal acute care hospitals nationwide. A 20% probability sample from all hospitals is then collected. Each hospital discharge is then weighted (weight = total number of discharges from all acute care hospitals in the United States divided by the number of discharges included in the 20% sample), which makes it nationally representative. The dataset for the years 2016 to 2018 consists of more than 7 million discharges each year. This equals to about 35 million yearly discharges nationwide when weighted and is representative of 95% of hospital discharges nationwide.
Study patients
Patients with International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes for NVUGIB were included in the study (Electronic Supplementary Material Table ‘Appendix’). Patients with and without cirrhosis were separated among NVUGIB patients. Patients were excluded if they were younger than 18 years of age. Institutional Review Board approval was sought, but the study was deemed exempt due to the use of de-identified, publicly available data.
Study variables and outcomes
The primary outcome was in-hospital mortality, which was provided within the NIS. The secondary outcomes were as follows: length of stay (LOS), blood transfusion, total hospitalization charges and costs, acute kidney injury (AKI) and dialysis requirement, hypovolaemic shock, vasopressors and intubation requirement, intensive care unit (ICU) admission, and parenteral feeding. Blood transfusion was considered to be completed within 24 h of admission if the time from admission to transfusion was zero or 1 day. The potential confounders that were adjusted for were as follows: age in years, gender, race, admission day as the weekend or weekday, median income in the patient’s zip code as 4 hierarchical categories, patient comorbidities as measured by the Deyo adaptation of the Charlson Comorbidity Index for administrative data, hospital location, hospital region, hospital teaching status as teaching or nonteaching, and hospital bed size [8].
Statistical analysis
Analyses were performed by using STATA, version MP 14.2 (StataCorp, College Station, Texas, United States). We used univariable logistic regression to compute unadjusted odds ratios (ORs). We used 2 distinct approaches to adjust for confounders: propensity score matching and multivariate regression analysis. Propensity scores were employed to match patients with NVUGIB who had cirrhosis with those who did not. A non-parsimonious multivariate logistic regression model was developed to estimate the propensity score. During model building for propensity score, the family specified was binomial and link as logit [9]. The double robust method was used to generate treatment weights, and the inverse probability of treatment weighting was used to match cases with controls using generalized linear models [9]. In the second analysis, multivariable regression models were built by including all confounders that were significantly associated with the outcome on univariable analysis with a cut-off p-value of 0.2 [10]. Variables deemed clinically important to the outcome based on literature review were included in the model irrespective of whether they were significantly associated on univariable analysis. A logistic regression model was used for binary outcomes, and a linear regression model was used for continuous outcomes. Fisher’s exact test for proportions and Student’s t-test for continuous variables was used for other calculations. All p-values were two-sided, with 0.05 as the threshold for statistical significance.
Missing data
Hospital variables did not have any missing data (Table I). However, 4 variables pertaining to the patient characteristics had missing data: most of the variables had a very low percentage of missing data (< 0.5%) except for race (2.90%) and median income in the patient’s zip code (1.74%). To test whether missing data could introduce bias, we assumed that data were not missing at random and applied the multivariate imputation by chained equations (i.e. MICE) method estimated from sequential multivariable models with fully conditional specifications [11]. Overall, 10 imputed datasets were constructed using information from all covariates used in the regression models, as well as other covariates in the database without missing information. Results with and without imputation were not meaningfully different. Thus, results without imputation are reported.
Results
Patient characteristics
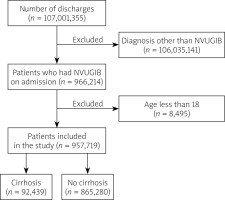
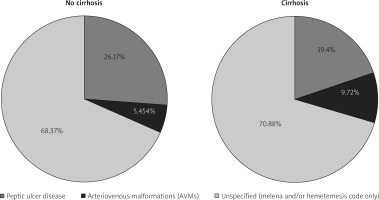
Figure 1 shows the flow diagram for study inclusion. The total number of patients in the studied NIS cohort was 107,001,355, among whom 957,719 (0.89%) had a diagnosis of NVUGIB. Among NVUGIB patients, 92,439 had cirrhosis. Patients with cirrhosis were more likely to be younger, male, and insured by Medicaid or private insurance, less likely to have Medicare, and had small differences in median annual income compared to NVUGIB patients without cirrhosis (Table II). Among NVUGIB patients, cirrhosis was more prevalent in the Hispanic population. Patients with cirrhosis had higher Charlson Comorbidity Index scores. There were numerically small but statistically significant differences in the hospital characteristics between the 2 groups: patients with cirrhosis were more likely to present to a large-sized hospital and less likely to be admitted to small and medium-sized hospitals than patients without cirrhosis. Patients without cirrhosis were more likely to be admitted to nonteaching hospitals in urban areas. The other characteristics were similar between the 2 patient groups or had differences numerically too small to be clinically significant. The proportion of various causes of NVUGIB in both groups is presented in Figure 2.
Table II
Patient and hospital characteristics
Mortality
Overall inpatient mortality from any cause in NVUGIB patients was 2.50%. There were 3.78% deaths for cirrhosis patients and 2.37% for patients without cirrhosis (unadjusted). After adjusting for confounders, cirrhosis patients with NVUGIB had higher odds of inpatient mortality compared to patients without cirrhosis (adjusted odds ratio (aOR): 1.31, 95% confidence interval (CI): 1.18–1.46, p < 0.001) (Table III).
Table III
Primary and secondary outcomes
Independent predictors of mortality
The strength of association of mortality from NVUGIB in cirrhosis patients with multiple variables was tested individually using univariate regression analysis. Multiple patient, hospital, and treatment-level variables were tested. The final model is presented in Figure 3. The variables found to be independent predictors of increased mortality from NVUGIB in cirrhosis were age, admission to medium, large-sized, and teaching hospitals, admission over the weekend, ascites, hepatic encephalopathy, spontaneous bacterial peritonitis, Clostridium difficile infection, malnutrition, heart failure, thrombocytopaenia, hyponatraemia, hepatorenal syndrome, hepatopulmonary syndrome, and cerebrovascular accident. The variable associated with lower odds of mortality from NVUGIB in cirrhosis was female gender. The rest of the variables had no influence on mortality from NVUGIB.
Mortality trend
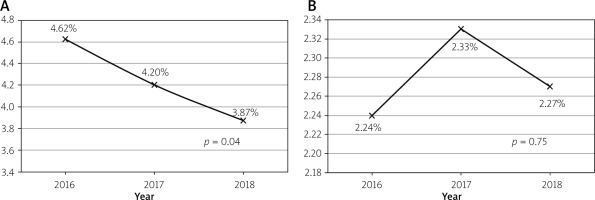
We also examined the mortality across the years in the studied dataset. The mortality from NVUGIB in cirrhosis patients decreased from 4.62% in 2016 to 3.87% in 2018 (p = 0.04) (Figure 4). However, NVUGIB mortality in patients without cirrhosis was unchanged across the years (2.24% in 2016 vs. 2.27% in 2018, p = 0.75).
Morbidity
The overall rate of acute kidney injury (AKI) was 19.67% and 20.52% among patients with and without cirrhosis, respectively, and this difference was significant after adjusting for confounders (aOR = 0.81, 95% CI: 0.78–0.85, p < 0.001). Similarly, kidney failure requiring dialysis was significantly different between the 2 subgroups (aOR = 0.58, 95% CI: 0.44–0.77, p < 0.001). Hypovolaemic shock did not differ among the 2 groups (aOR = 1.01, 95% CI: 0.91–1.11, p = 0.90).
Treatment setting and length of stay
The overall mean LOS was 4.23 days for patients hospitalized with cirrhosis, 4.49 days for patients with, and 4.21 days for patients without cirrhosis. After adjusting for confounders, patients with cirrhosis had a significantly lower comparative mean LOS by 0.44 days (mean adjusted difference in LOS: 0.44, p < 0.001). 5.58% of cirrhosis patients required ICU stay compared with 2.78% in non-cirrhosis patients (aOR = 1.29, 95% CI: 1.18–1.40, p < 0.001). Similarly, cirrhosis patients had higher odds of requiring intubation (aOR = 1.42, p < 0.001), but the requirement of vasopressor support was not significantly different (aOR = 0.94, p = 0.60).
Resource utilization
Markers of resource utilization used were as follows: total hospitalization costs, total hospitalization charges, blood transfusion, and parenteral nutrition. Evaluation of the mean total hospitalization charges showed that they were $44,193 (95% CI: $43,632–$44,754) for the overall study population, $51,637 (95% CI: $50,338–$52,936) for cirrhosis patients, and $43,398 (95% CI: $42,854–$43,942) for patients without cirrhosis (unadjusted numbers). After adjusting for the confounders, total hospitalization charges were significantly lower for cirrhosis patients by $3384 with a p-value of < 0.001. Upon evaluating the charge per day, we found it to be $12,909 for cirrhosis patients and $11,430 for patients without cirrhosis (p < 0.001). Similarly, when we examined total hospitalization costs, it was found that the overall study population, cirrhosis patients, and non-cirrhosis patients had mean total hospitalization costs of $10,667 (95% CI: $10,578–$10,756), $12,295 (95% CI: $12,064–$12,526), and $10,493 (95% CI: $10,405–$10,582), respectively. Cirrhosis patients had significantly lower comparative adjusted mean total hospitalization costs by $822.71 (p < 0.001). Upon evaluating the cost per day, we found it to be $3114 for cirrhosis patients and $2810 for patients without cirrhosis (p < 0.001). The requirement of blood transfusion (overall and within the first 24 h) was similar in both groups (aOR = 1.02, 95% CI: 0.98–1.05, p = 0.37 and aOR = 1.04, 95% CI: 0.99–1.08, p = 0.06 respectively). The urgency in time for first blood transfusion represented by mean time in days to first blood transfusion was similar in both groups (0.55 vs. 0.55, p = 0.83). Cirrhotic patients had lower odds for the need for parenteral nutrition (aOR = 0.47, 95% CI: 0.37–0.60, p < 0.001) (Table III).
Treatment modalities
Upper endoscopy
For patients with total NVUGIB in cirrhosis, an in-hospital upper endoscopy without therapy (diagnostic endoscopy) was performed during 57.86% of admissions, and endoscopic therapy was administered during 14.85% of admissions (Table IV). An in-hospital diagnostic endoscopy was performed in 58.54% of admission in cirrhosis patients compared to 57.79% in patients without cirrhosis (unadjusted numbers). In comparison, endoscopic therapy was administered more in cirrhosis patients (17.20% vs. 14.60% of admissions). After adjusting for confounders, the cirrhosis group had significantly higher odds of receiving endoscopic therapy than non-cirrhosis patients with NVUGIB (aOR = 1.08, 95% CI: 1.03–1.13, p < 0.001). However, diagnostic endoscopy was performed 10% more often in non-cirrhosis admissions (aOR = 0.90, 95% CI: 0.87–0.93, p < 0.001). Early (within 24 h) upper endoscopy (whether diagnostic or with therapy) was performed more often in cirrhosis patients (49.04% vs. 42.46%, p < 0.001).
Table IV
Procedure performed
Radiology-guided embolization of a bleeding vessel
For patients with NVUGIB in cirrhosis, radiography-guided embolization was required for 0.54% of admissions. It was required for 0.42% of admissions in cirrhosis patients compared to 0.56% in non-cirrhosis patients; after adjusting for confounders, the cirrhosis group was 53% less likely to have undergone it than non-cirrhosis (aOR = 0.47, 95% CI: 0.36–0.61, p = 0.03).
Discussion
The overall mortality rate in NVUGIB varies from 5% to 12% in different parts of the world [12]. Data from our study of 957,719 patients from the United States demonstrated overall mortality for NVUGIB to be 2.50%. The mortality of NVUGIB among patients with and without cirrhosis was 3.78% and 2.37%, respectively, which was lower than previously reported in the literature. Owing to the large sample size, the likelihood of beta error is low in our study, thus being a better representative of the inpatient population with NVUGIB. We utilized NIS data from 2016 to 2018, and recent advances in endoscopic treatments of NVUGIB have led to a decrease in mortality. We also demonstrated decreasing mortality trends from NVUGIB in cirrhosis patients compared to patients without cirrhosis.
Historically reported in the literature, predictors of mortality for NVUGIB include advanced age, coexistent diabetes or malignancy, haematological conditions, alcohol use, hypoalbuminaemia, haemodynamic instability, haematemesis upon admission, in-hospital bleeding, re-bleeding, need for surgery, and admissions over weekends [13–15]. Our study also confirmed age, weekend effect, and comorbidities as independent mortality risk predictors as well as insurance status, admission to medium or large-sized hospital, and presentation to an urban teaching hospital as additional risk factors. Other independent mortality predictors identified included the presence of ascites, hepatic encephalopathy, spontaneous bacterial peritonitis, clostridium difficile infection, malnutrition, heart failure, thrombocytopaenia, hyponatraemia, hepatorenal syndrome, and cerebrovascular accident. Ascites, albumin, and hepatic encephalopathy are prognostic components of Child Turcotte Pugh Classification, whereas serum sodium and creatinine levels are used to compute the MELD Sodium Score, a validated scoring system for mortality in chronic liver disease [16, 17].
Compared to a well-reported higher incidence of AKI in NVUGIB in cirrhosis, our study demonstrated less AKI in cirrhotic patients compared to patients without cirrhosis [18]. We relied on ICD-10-CM diagnosis codes to extract patients from the database, and there exist distinguished codes for AKI and hepatorenal syndrome. The diagnosis of AKI and hepatorenal syndrome overlap, and cirrhosis patients with creatinine disturbances on presentation are initially coded as AKI but later reclassified to hepatorenal syndrome if that is truly the aetiology of kidney dysfunction. Thus, even though our results are reflective of clinical practice in the United States, caution should be taken while interpreting AKI findings in the study because low baseline creatinine in cirrhosis patients can lead to misdiagnosis of AKI.
Despite limited evidence of outcome benefit, prophylactic endotracheal intubation is commonly performed prior to endoscopy in upper GI bleed for airway protection [19]. Although studies are lacking comparing instances of intubation in the setting of NVUGIB between cirrhosis and non-cirrhosis, we demonstrated increased occurrence in cirrhotic patients (4.52% vs. 2.01%). We illustrated that the therapeutic endoscopy was carried out more in cirrhotic patients than diagnostic endoscopy alone. That could be explained by greater severity of gastroduodenal ulcers and the presence of high-risk bleeding stigmata in cirrhosis patients. As demonstrated by Garg et al., early endoscopy can lead to shorter LOS [20]. Early (within 24 h) upper endoscopy was carried out more in cirrhosis patients for NVUGIB in our study (49.04% vs. 42.46%, p < 0.001). Recent advances in endoscopic therapies to control bleeding and performance of earlier endoscopy result in lower overall resource utilization due to decreased LOS, as demonstrated in our study.
There are various limitations to our study. First, the exposure is not entirely randomized, owing to the retrospective design of our study. We relied on multivariate regression models and propensity matching to account for confounders. The results obtained from both methods were comparable, which diminishes the likelihood of confounding, although residual confounding can still occur. Additionally, we controlled for the diverse patient and hospital-level characteristics, which lessens the chance even further. Second, an administrative database was evaluated to obtain the data. The use of ICD-10 codes in place of clinical parameters can lead to misclassification of the diagnosis. ICD-10-CM codes were used to derive the data, which are more specific than ICD-9-CM and have shown high sensitivity and specificity to investigate gastrointestinal diseases [21]. Third, data on medical treatments is not captured in the NIS; therefore, the use of medication making patients vulnerable to UGIB, including antiplatelet therapy and anticoagulants, could not be controlled for in the analyses. Similarly, due to inaccessible data on the laboratory values in the database, MELD or Child-Pugh scores could not be used; instead, we applied the Charlson Comorbidity Index to control for comorbidity burden, a generalized validated prognostic scale, as was employed in previous studies. Finally, we reported the overall inpatient mortality of patients who were hospitalized with a principal diagnosis of NVUGIB, because the cause of death could not be determined from the database. We believe further randomized trials are imperative to overcome the limitations experienced in this study.
Regardless of these shortcomings, our study has several strengths. We described the rate of NVUGIB in cirrhosis as 3.78% in the hospitalized population across the United States, which is more than the overall rate of NVUGIB (2.50%). We used NIS, which includes data on patients at diverse hospital-level characteristics from more than 45 states as outlined in the methods section. This results in superior external validity and generalizability; hence, we believe that the results obtained should reflect the patient population admitted to the hospitals across the United States. We also found out that hepatorenal syndrome, cerebrovascular disease burden, and clostridium difficile infection serve as predictors of mortality from NVUGIB in cirrhosis patients. Moreover, NIS eliminates the frequently experienced limitation of single-centre studies by allowing the use of a large sample size because it is the largest publicly available, all-payer database comprising the inpatient population. Propensity matching is a powerful tool while analysing administrative databases, and it helps control confounding by indication [22]. It uses a wide range of empirically derived covariates that constitute surrogates for unmeasured confounding variables while matching cases with controls [23, 24]. Utilizing nationally representative data, our study eradicates biases connected with practice patterns in single- or multi-centre studies. Likewise, the distinguished variables in the database awarded the opportunity to consider elements such as household income estimates, hospitalization cost, and hospital factors, which are not generally achievable in single-centre studies.
Conclusions
Cirrhosis acts as a significant predictor of mortality in NVUGIB. We also showed that admission to larger bed-size hospitals, hepatorenal syndrome, cerebrovascular disease burden, heart failure, and clostridium difficile infection serve as independent predictors of mortality from NVUGIB in cirrhosis patients and should alarm the physicians of poorer prognosis. Identification of these should lead to proper placement of the patient in a hospital unit with the appropriate level of care to provide effective and high-value care for the patient that potentially helps reduce mortality. NVUGIB in patients without cirrhosis was found to have a higher resource utilization as indicated by hospital LOS, and adjusted total hospitalization charges and costs, but the rates of upper endoscopy therapy involving both acuity and complexity of intervention during the procedure were greater in the cirrhosis subgroup. Further research is warranted to test interventions to reduce the morbidity and mortality gap between these 2 subgroups.