Liver abscess is a rare condition with a high mortality rate. The most common pathogens isolated in patients with liver abscesses include Klebsiella pneumoniae, Streptococcus spp., Pseudomonas spp., and Escherichia coli [1]. Its most common causes are biliary tract diseases, such as cholelithiasis, strictures and tumors. The English-language literature distinguishes two types of liver abscesses of bacterial etiology: infectious hepatic cyst (IHC) and pyogenic liver abscess (PLA) [2]. In the available literature in English, 2 cases of liver abscesses caused by Raoultella planticola have been reported: the first one, reported in 2016, was an abscess of the left lobe of the liver in a patient with ketoacidosis secondary to type 2 diabetes mellitus (DM2) [3], while the other one was associated with transarterial chemoembolization (TACE) for hepatocellular carcinoma [4]. Both of those case reports concerned abscesses classified as PLA. IHC caused by R. planticola that we present below has not been reported so far.
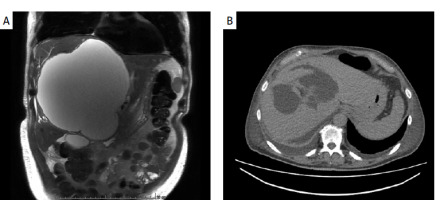
A 68-year-old man with benign prostatic hyperplasia was admitted to the hospital with fever of up to 40°C persisting despite oral antimicrobial therapy. In 2023, the patient had been diagnosed with an extensive liver cyst measuring 13 × 15 × 17.5 cm. The patient had no history of invasive medical procedures. An artist by profession, among other things he made sculptures in clay. On admission to our department, the patient was in good general condition, with no jaundice; the abdomen was soft and nontender. An extensive pathological mass was palpable in his epigastric area. Laboratory tests revealed: alanine transaminase (ALT) 65 U/l, total bilirubin 19.6 µmol/l, γ-glutamyl transferase (GGT) 292 U/l, white blood cells (WBC) 12 G/l, C-reactive protein (CRP) 254 mg/l. Given the suspicion of liver cyst infection, an abdominal magnetic resonance imaging (MRI) scan was obtained, revealing a cyst in the right liver lobe measuring 16 × 18 × 20 cm with a contrast-enhancing capsule – an abscess, with dilatation of intrahepatic bile ducts in both lobes (Figure 1 A). In addition, features of gallbladder adenomyomatosis were observed. After blood cultures were collected, the empirical therapy with piperacillin and tazobactam was administered. On the 5th day of hospitalization, a percutaneous drainage was performed under ultrasound guidance, yielding a total outflow of about 4000 ml of purulent contents, followed by biliary contents in the drain. A pus culture showed growth of R. planticola, resistant to ampicillin. In the following days of hospitalization drainage of a significant amount of biliary contents, at about 1500 ml/day, persisted. On the 11th day of hospitalization, an abdominal computed tomography (CT) scan was obtained, revealing two-banded irregular fluid reservoirs in segments IV, VIII, and V, measuring 9 × 14.5 × 6.5 cm, and a thickened capsule with a small gas bubble, consistent with a residual abscess (Figure 1 B). Laparoscopy with intraoperative ultrasound evaluation was performed: the fluid lesions were drained, and pigtail drains were left in each lesion. Because of persistent drainage of bile, the patient underwent two endoscopic retrograde cholangiopancreatography (ERCP) procedures – because of a leak of bile from the left hepatic duct, a prosthetic device was inserted into it and the common bile duct. The patient was discharged home in good general condition.
Figure 1
A – Abscess of the right lobe of the liver: magnetic resonance imaging before treatment; B – status after abscess drainage, fluid spaces visualized – computed tomography image
Raoultella planticola is a Gram-negative bacillus and a rare human pathogen. For years it was considered an environmental bacterium, harmless to humans. In 1984, the first case of infection was reported [5], and the perception of the pathogenic potential of this bacterium changed. It is now known that R. planticola can cause many different clinical forms of infection, including biliary tract infections [6] and pneumonia [7].
Risk factors of R. planticola infection include, amongst others, extreme age groups, previous history of invasive medical procedures, including endoscopic procedures, immunosuppressed status during cancer treatment, DM2 and consumption of fish and seafood. None of the aforementioned factors were identified in our patient.
The issue that draws our attention when considering the possible causes of this infection is the patient’s constant occupational contact with clay. In a paper published by Ulukent et al., a patient with cholecystitis reported a history of geophagia in childhood [8]. In both cases, close contact with the natural environment was the likely source of bacteria entering the gastrointestinal tract.
Given the biofilm-forming ability of R. planticola, it is possible for this microorganism to persist in the bile ducts even for many years after initial contact with this pathogen [9]. Blihar et al. indicated cholestasis as a factor that facilitates adhesion and colonization of the biliary tract by bacteria of this species [9]. In the case we report here, the pre-existing liver cyst, because of its large size, caused compression of the surrounding tissues with dilatation of the intrahepatic bile ducts and cholestasis.
In considering the possible factors contributing to R. planticola infection, it is noteworthy that the magnetic resonance imaging (MRI) scans revealed the presence of gallbladder adenomyomatosis. In a paper by Doherty et al. describing chronic cholecystitis, the authors state that the existence of this disorder may be related to the development of an infection of this etiology [10]. Nevertheless, the data collected so far do not allow a clear link to be established between the two disease entities.
Infections caused by Raoultella are relatively rare, and clinicians are insufficiently aware of this possibility. R. planticola, because of its phylogenetic similarity to bacteria of the genus Klebsiella, may be misidentified by microbiology laboratories. The frequency of intraabdominal infections with this etiology is likely underestimated.










