A 63-year-old woman was initially referred for nephrectomy with a presumed diagnosis of advanced renal cell carcinoma (RCC) of the left kidney. The patient presented with flank pain, fatigue, and unintentional weight loss over several months. Her medical history included hypertension, a smoking habit (20 pack-years) and a significant family history of cancer (two sisters, one with uterine and one with lung cancer).
Computed tomography (CT) of the abdomen revealed a large mass originating from the upper pole of the left kidney, measuring 8.0 × 7.2 × 7.6 cm. The mass appeared as a solid, malignant tumor extending into the spleen and causing infarction, while infiltrating the pancreatic tail and the left adrenal gland. No significant enlargement of the left renal vein or inferior vena cava was observed. These findings were consistent with RCC infiltrating neighboring organs (Figure 1).
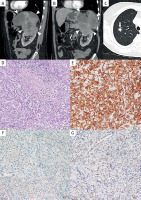
Figure 1
Computed tomography (CT) of the abdomen in the arterial phase, shown in soft tissue window in multiplanar reconstructions (A, B), and of the chest in the lung window in the axial plane (C). In the sagittal (A) and paracoronal planes (B), a large mass (arrowheads) is visible, infiltrating the upper pole of the left kidney, the pancreatic tail, the spleen, and the left adrenal region. In the right lung (C), a nodule (arrow) with spiculated margins is observed. Pancreatic undifferentiated carcinoma with osteoclast-like giant cells (hematoxylin & eosin staining, magnification 200×) (D). Positive CK7 staining in cancer cells (magnification 200×) (E). Negative SMAD4 staining in cancer cells (magnification 200×) (F). Negative PAX8 staining in cancer cells (magnification 200×) (G)
Chest CT staging revealed a solitary 10-mm pulmonary nodule in the right upper lobe, suspicious for metastasis. Additional smaller nodules with ground-glass opacity were noted in the upper lobes bilaterally, likely inflammatory in origin. Based on imaging and clinical presentation, the patient underwent radical nephrectomy with splenectomy and partial pancreatectomy.
Histopathological examination revealed an undifferentiated carcinoma with osteoclast-like giant cells originating from the pancreas, with invasion of the kidney, spleen, and adrenal gland. Immunohistochemistry confirmed pancreatic origin, showing positive staining for CK7 and CKAE1/AE3, and negative staining for PAX8, CD10, and SMAD4, ruling out renal primary tumor. The final pathological staging was pT3N1M1, with metastatic involvement in one of two peripancreatic lymph nodes and one renal vessel lymph node. Next generation sequencing revealed mutations in KRAS G12V and TP53, further supporting the pancreatic origin of the cancer. KRAS codon 12 mutations, found in 90–95% of pancreatic ductal adenocarcinomas (PDAC), include the G12V variant in approximately 30% of cases [1].
Post-surgical biopsy of the largest pulmonary nodule revealed adenocarcinoma of lung origin, unrelated to the primary pancreatic tumor. Given this dual diagnosis of pancreatic carcinoma and lung adenocarcinoma, the patient was initiated on palliative chemotherapy with cisplatin and gemcitabine. At the time of reporting, the patient had completed two cycles of chemotherapy with stable symptoms.
This case involved a rare form of pancreatic undifferentiated carcinoma with osteoclast-like giant cells, representing just 0.4% of pancreatic cancers [2], and mimicking renal cell carcinoma both clinically and radiologically. While initial imaging suggested aggressive RCC with direct invasion into adjacent organs, the final diagnosis revealed a rare subtype of pancreatic cancer – undifferentiated carcinoma with osteoclast-like giant cells – with kidney infiltration, a presentation not previously reported in the literature. In contrast, when these two organs are involved, RCC typically metastasizes to the pancreas, mimicking primary pancreatic cancer [3]. This case emphasizes the importance of histopathological evaluation when imaging suggests an unusual pattern of invasion.
The patient’s management was complicated by the discovery of a synchronous pulmonary adenocarcinoma. Despite the aggressive nature of the pancreatic carcinoma, the patient’s clinical condition remains stable. Ongoing treatment will be adjusted based on therapeutic response and symptomatology.










