Introduction
Laparoscopic cholecystectomy for symptomatic gallstones is one of the most common surgical procedures, with the most common indication being the presence of symptomatic gallstones. Although the procedure is considered routine, with clear evidence to demonstrate its feasibility even on a day-case basis, potential complications such as residual choledocholithiasis and mainly bile duct injuries are associated with major morbidity and naturally are of significant concern for both surgeons and patients. Although the concept of “critical view of safety” has revolutionised the principles of “lege artis” cholecystectomy, aiming to avoid bilio-vascular injury at the porta hepatis, there is no global consensus regarding the required extent of dissection of the cystic duct during the procedure, in order to reduce the chance of retained ductal stones post cholecystectomy [1]. Anecdotally, many surgeons would try with the laparoscopic graspers to feel for possible cystic duct stones and gently milk them towards Hartmann’s pouch, prior to application of the cystic duct clips and transection of the gallbladder from the cystic duct stump. Other surgeons, usually with specialist hepatobiliary training, would assess intra-operatively for cystic duct/common bile duct lithiasis using on-table cholangiograms (OTCs) or even laparoscopic ultrasound.
Under this notion and taking into account additionally the great anatomical variability of the extrahepatic biliary tree, it becomes evident that accurate pre-operative planning could play a crucial role in performing a safe cholecystectomy, particularly for the majority of general surgeons who do not have specialist hepatobiliary experience [2, 3]. As a result, the liberal use of pre-operative magnetic resonance cholangiopancreatography (MRCP) is gaining popularity as a roadmap prior to cholecystectomy, aiming to assess primarily for the presence of migrated gallstones within the cystic duct or common bile duct, as well as providing information regarding the anatomical features of the extrahepatic biliary tree on an individualised basis [4–6]. Although the examination is accompanied by an increase in the healthcare-associated costs, the performance of the pre-operative cholangiopancreatography and its correct interpretation enables, particularly, non-hepatobiliary surgeons to tailor the management of cases with increased complexity, such as patients with Mirizzi’s syndrome, or cases with concurrent extrahepatic bile duct lithiasis that would usually require clearance through endoscopic retrograde cholangiopancreatography (ERCP) prior to cholecystectomy [7–9].
As far our unit is concerned, having mainly a colorectal subspecialty interest, we have a low threshold of performing MRCPs for patients with symptomatic gallstones, who present with de-arranged liver function tests, pancreatitis, or evidence of dilatation of the intra/extrahepatic biliary tree in first-line imaging modalities, (transabdominal ultrasound or computed tomography), so as to assess possible bile duct lithiasis. As a result, a high percentage of the patients that are scheduled for cholecystectomy will have undergone a pre-operative MRCP, enabling early identification of anatomical abnormalities of the extrahepatic biliary tree and accurate assessment of concurrent lithiasis of the cystic duct/main bile duct.
Aim
Using this institutional database, we assessed the frequency of anatomical variations of the cystic duct and potential association of those with stone migration within the cystic duct itself, aiming primarily to identify whether it is feasible and necessary to achieve extensive skeletonisation of the cystic duct during routine laparoscopic cholecystectomy, in order to reduce the possibility of residual choledocholithiasis due to retained cystic duct stones.
Material and methods
We performed a retrospective review of the institutional database of all patients who underwent cholecystectomy for symptomatic gallstones, on both an emergency and elective basis, over a 3-year period (01/04/2016 – 31/03/2019). From this pool of patients, we identified those who underwent pre-operative MRCP for any reason, and we assessed the following characteristics: cystic duct length, cystic duct insertion point in relation to the common hepatic duct (lateral, medial, anterior, posterior), the level of insertion of the cystic duct to the common hepatic duct (upper/mid/lower 3rd – measuring the distance between the ampulla of Vater and the confluence of the right and left main hepatic ducts), as well as the frequency of encountered gallstones within the cystic duct. Analysis of the images was performed using our hospital’s electronic software and checked against the findings issued by the reporting Consultant Radiologists. Possible discrepancies were discussed between the principal and senior authors (CS and PJ) and were resolved by mutual agreement. Our study did not require approval from our institutional Ethics Committee due to its retrospective and non-invasive nature.
Results
Among the 763 patients who underwent cholecystectomy for symptomatic gallstones in our institution during the study period, a total of 284 (males/females: 81/203) had been evaluated pre-operatively with MRCP (37.2%), and they were included in the final analysis. The average length of the cystic duct was 3.76 cm in our series, with 12 patients having a significantly short cystic duct with less than 1 cm length (4.2%). With respect to the incidental presence of cystic duct stones, these were detected only in 5/284 (1.8%) patients, while common bile duct stones were detected in 38/284 MRCPs (13.4%).
Interestingly, we found that the conventional anatomy of the cystic duct (lateral insertion at the common hepatic duct at the mid-point between the ampulla and the confluence of the right and left hepatic ducts) was present only in 138/284 patients (48.6%). Regardless of the insertion height, lateral insertion was noted in 178/284 patients (62.7%), followed by medial insertion in 39/284 (13.7%), anterior insertion in 28/284 (9.9%), and posterior insertion in 33/284 (11.6%) of the patients, respectively (results summarised in Table I). We identified 1 case where the cystic duct was draining in the proper right hepatic duct and another case where the cystic duct was communicating with an aberrant right hepatic duct. Moreover, in 3 patients we identified complete absence of the cystic duct due to development of Mirizzi’s syndrome. The significant variability of the cystic duct anatomy that was demonstrated through our pre-operative MRCPs can be seen in a representative way in Figures 1–7.
Table I
Summary of the encountered anatomical variations of the cystic duct; notably, the perceived typical anatomy is present in less than 50% of the patients
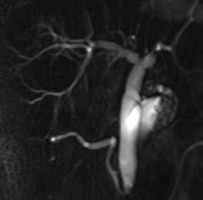
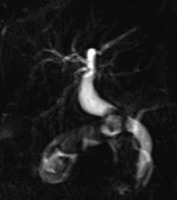
Figure 1
High anterior insertion of the cystic duct, adjacent to the main hepatic duct confluence/ incidental distal common bile duct stone

Figure 3
Drainage of the cystic duct with a segmental right hepatic duct, forming a common channel prior to insertion to the common hepatic duct
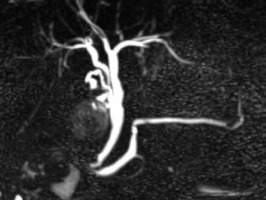
Figure 4
Lateral insertion of the cystic duct, running parallel in anatomical proximity to the common hepatic duct
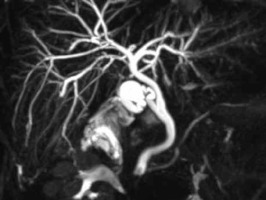
Figure 5
Absence of cystic duct, with development of cholecysto-choledochal fistula (Mirizzi syndrome), with stone migration within the common bile duct
Discussion
Although a very commonly performed surgical procedure performed by the vast majority of general surgeons regardless their subspecialty interest, laparoscopic cholecystectomy can be accompanied by major complications, such as bile duct injuries or recurrent/residual choledocholithiasis. These complications, especially when not recognised early, as well as the associated major morbidity and occasionally mortality risk, usually have significant medicolegal implications for the operating surgeons and their departments. Therefore, the culture of performing a safe cholecystectomy is now well established worldwide, with the popularisation of the concept of “critical view of safety”, having as adjuncts the liberal use of intraoperative cholangiography or bail-out procedures in cases of advanced complexity [10]. The core of this rationale is to ensure non-violation of the key anatomical principles of cholecystectomy, with correct identification of the underlying anatomy. However, most general surgeons do not routinely perform OTC in their practise, and hence one could arguably be not confident and probably not safe to interpret an OTC under the stress of the occasionally aberrant anatomy; a misinterpreted cholangiogram can be as dangerous as a never-performed cholangiogram. Obviously, it must be taken into account that, in addition to the above, the majority of general surgeons have no advanced hepatobiliary training experience, which can prohibit early identification of aberrant ductal anatomy, as well as prompt recognition and definitive treatment of potential ductal injuries or the presence of concurrent choledocholithiasis. As a result, performance of pre-cholecystectomy MRCPs for assessment of choledocholithiasis and clarification of the biliary tree anatomy is gaining popularity, particularly amongst non-hepatobiliary surgeons. The examination enables clear identification of common bile/common hepatic/cystic duct stones, in addition to cross-sectional and three-dimensional reconstruction images of the biliary tree, which are particularly helpful for pre-operative planning in the presence of atypical ductal anatomy.
In our institution, which has a mainly colorectal subspecialty interest, under this rationale, we have adopted a low-threshold MRCP policy for patients with symptomatic gallstones, who present with abnormal liver function tests, gallstone-related pancreatitis, or dilatation of the intra/extrahepatic biliary tree in transabdominal ultrasound or computed tomography. Because we do not perform routine OTCs of bile duct explorations in our unit, given our main colorectal subspecialty orientation, our main surgical concern during performance of standard laparoscopic cholecystectomies would be the clear identification of the cystic duct and cystic artery, in line with the “critical view of safety”, without further routine dissection towards the main bile duct. As a result, anatomical variations of the cystic duct and information regarding the presence of concurrent cystic duct stones are of particular interest, because this is the main biliary structure that we would expect to encounter during our dissection. Therefore, we aimed to use the relevant pre-operative cholangiography data from our institutional database to assess the frequency of the anatomical variants of the cystic duct and possibly to correlate it with the presence of ductal lithiasis.
In accordance with similar results from previously published studies, our data demonstrated that the conventional cystic duct anatomy (right lateral insertion at the mid-point between the confluence of the right/left hepatic ducts and the ampulla of Vater) was present only in fewer than 50% of our patients. Interestingly, fewer than 2% of our patients had incidental cystic duct stones [11–15]. These findings signify clearly that an attempt to extensively skeletonise the cystic duct during routine laparoscopic cholecystectomy is an unnecessary step and even potentially hazardous for the patient, particularly when the operation is not performed by surgeons with hepatobiliary expertise. In addition, in our series we identified 17 cases (6% of the study group) with red-flag radiological features regarding a high-risk of bile duct injury due to gross deviation from the standard expected anatomy (12 patients with cystic duct < 1 cm, 3 patients with absent cystic duct – Mirizzi’s syndrome, and 2 patients with communication of the cystic duct with aberrant or non-aberrant right hepatic duct). On these occasions, the availability of the pre-operative MRCP enabled the operating surgeons to proceed with upfront subtotal cholecystectomy in 9 patients, to avoid a possible bile duct injury; conversion from laparoscopic to open surgery was required in 4 cases, to allow completion of the procedure in a safer manner.
To the best of our knowledge, there is no established consensus regarding the required extent of dissection of the cystic duct prior to its division during routine laparoscopic cholecystectomy, to theoretically reduce the risk of residual choledocholithiasis. Under this notion, we believe that our study sheds light on an important step of this very common surgical procedure, but this can have dreadful complications upon misinterpretation of the biliary anatomy. Because we applied no exclusion criteria for our analysis, we believe that our study has a pragmatic substance, reflecting the everyday clinical practise. However, being retrospective in nature, it bears an associated selection bias. Also, because we did not come across some of the rarer anatomical biliary tree abnormalities, such as duct duplication or choledochal cysts, we hypothesize that our results could have been even more robust with a larger study population. However, we deemed the high percentage of non-typical cystic duct anatomy and extremely low percentage of incidental cystic duct stones as sufficient for us as a group of authors to draw conclusions in terms of our future operative strategy.
Conclusions
Due to significant anatomical variations and low likelihood of incidental cystic duct stones, extensive dissection of the cystic duct to reduce the risk of retained ductal stones is not advocated. Appropriate use of preoperative MRCP purely for purposes of cholangiography, as in patients with recurrent severe cholecystitis, can be useful in surgical planning in order to reduce the risks of inadvertent bile duct injuries, particularly in the absence of advanced hepatobiliary surgical experience.