INTRODUCTION
An epidemic of cases with unexplained low respiratory infections was detected in Wuhan, China in late 2019. The virus is very contagious and spread quickly globally. On January 30, 2020, the outbreak of the novel coronavirus 2019 (COVID-19) was declared by the World Health Organization (WHO). The outbreak spread to several countries through human-to-human transmission [1], including Iraqi Kurdistan [2].
Healthcare workers (HCWs) are at a high risk of exposure to occupational infection and death because they are on the frontline [3]. In some countries, one in ten HCWs is infected with coronavirus [4]. The HCWs are also more likely to be quarantined during the fight against an outbreak. Quarantine is defined as the separation and restriction of movement of people who have been exposed to an infectious disease. Quarantine aims to decrease the risk of infecting other community members [5], and was considered to be a useful public health measure to prevent the spread of infectious diseases during the severe acute respiratory syndrome (SARS) outbreak in 2003 and the Ebola outbreak in 2014. It is acknowledged to be a primary measure against COVID-19 as well.
Many frontline HCWs are likely to be quarantined during a COVID-19 outbreak, and the quarantine could have adverse psychological effects on them [6]. The HCWs are thus susceptible to the negative mental health effects of the quarantine and may experience high levels of distress and anxiety due to social isolation [7]. Physicians and other clinicians are seriously concerned about their family members’ well-being. The HCWs’ mental health is extremely important during a pandemic because they constitute the central plank of the health system’s response [8]. The quarantine of medical staff could raise all-cause mortality and disease burden [9].
Previous studies have reported that COVID-19 can lead to lowered health-related quality of life (HRQoL) by impairing the physical and psychological well-being of a person [10-12]. Frequent experiences of fear and anxiety owing to viral transmissions in the workplace and the possibility of cross-contamination among family members, as well as sudden increased work pressure, tend to result in mental health burdens. Therefore, the person’s struggle to balance professional and personal life can result in mental health problems like depression and suicidal tendencies [13]. One of these studies included 529 physicians from different regions and specialties. The physicians were asked to report their understanding of quarantine and quarantine behaviors. They were classified as COVID-19-designated group and non-COVID-19 designated group. In addition, the COVID-19 designated centers were subdivided into those who work in low and high-risk areas. The study reported that the most common expressions reported by the physicians were worry (67.5%), isolation (56.9%), and fear (49.7%). The physicians who were aged 60 and older were more likely to feel isolated, and female physicians were more likely to experience fear and worry. The physicians were less likely to experience fear compared to previous exposure to similar traumatic events [14]. The high levels of depression and anxiety among HCWs have been reported in other studies as well [15-17].
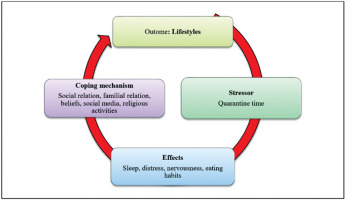
The number of infected and severely ill patients is escalating as well as the number of exposed HCWs who are under self-quarantine, either because they have been infected with COVID-19 or have been in close contact with a confirmed case. We need physically and mentally healthy and well-equipped HCWs to manage COVID-19 cases. There is not sufficient information about the psychological well-being and behavioral lifestyles of HCWs during the COVID-19 pandemic in this region. Therefore, in this paper we examine the impact of a period of quarantine as an external stressor leading to distress and impacting sleep, healthy lifestyle behaviors, and familial relations among healthcare workers during the COVID-19 pandemic.
METHODS
Study design, sampling, and participants
The study was conducted using a descriptive qualitative inquiry. The qualitative approach is appropriate when little is known about the issue being investigated, such as the experiences of frontline HCWs in Iraq [18]. In this study, 12 healthcare workers aged 21-41 (mean: 26; SD: 4 years), who were quarantined for close contact with a COVID-19 confirmed case, were included.
The HCWs were exposed to a confirmed patient with COVID-19 through an operation. The team was working on a patient with confirmed thyroid cancer. The prevention center of the region called the team that patient’s family members tested positive for COVID-19. Later the patient tested positive for COVID-19. The HCW team was quarantined for 14 days based on the local and national guidelines for the prevention of a COVID-19 outbreak in 2020. The staff was quarantined between the first and fourteenth of June 2020. The participants included 10 females and 2 males, including a surgeon (n = 1), junior resident doctors (n = 2), paramedics (n = 2), nurses (n = 6), and a receptionist (n = 1). All of the participants were Kurdish.
The individual interviewing method was conducted with the participants after quarantine period, between the fifteenth and twentieth of June 2020. We selected the semi-structured interviewing approach with the medical staff to examine the impact of the quarantine on their well-being as well as lifestyles and familial relations (see Figure I). Semi-structured interviews allow us to ask a schedule of prepared as well as to follow up on responses of the participants.
We obtained the written consent form from all participants before conducting the interview. Protection of the confidentiality of participants’ personal information was guaranteed. The second author was one of the surgeons who were quarantined along with the 12 medical staff mentioned. However, the author was not included in the study as a participant to avoid bias. The medical staff was the operation team of the second author but there was no coercion involved in their participation, and none of them refused to participate in this study.
Interviews
The second author contacted the participants for an interview. The author called the HCWs to discuss information and arrange an interview time. All of the individuals who were in quarantine consented to participate in the study after the aim of it was explained to them. The interviews were performed with the participants in a quiet room at Azadi Teaching Hospital. The interviewer was a trained nurse other than those who were quarantined among the studied team. We trained a nurse to interview the participants to avoid bias. The second author trained a nurse on how to conduct an interview with the surgery team. The required information on how to make an interview was given to the nurse. Within sufficient time, the study questions were explained to the nurse to avoid bias. All of the interviews were performed by a trained nurse through face-to-face interviews, which were audio-recorded and then transcribed verbatim. The notes taken at the time of the interview by the interviewer were included in the analysis as well.
The aim of the study was explained to the participants. The following general information was collected: age, gender, specialism (nurse, general physician, and surgeon) and whether the respondent had a chronic disease or pre-existing medical condition. The participants were asked to explain the following questions:
Please explain your experience during the quarantine period.
Did you experience stress during the quarantine? Please give the reasons.
Did your lifestyle change during the quarantine period? What changed?
How did the quarantine period affect your relationship with your family, either positively or negatively?
How did you spend your time during the quarantine?
What did you do to reduce the effects of quarantine? In this question, we asked the participants to explain their coping mechanisms.
The interviewer recorded the responses of the participants on her cell phone. The participants were encouraged to give examples from their quarantine experiences. The interviews were performed during the working time of the HCWs at the hospital, and lasted 30-45 minutes.
Data analysis
We analyzed the data using thematic content analysis and content analysis with a deductive approach using the Graneheim and Lundman method [19]. The first author listened to and translated the interviews from Kurdish into English. The transcripts were sent to the second author to check the contents for any errors. The second author listened to the interviews and checked the translation independently from the first author. The contents confirmed by the second author were sent to the third author to check the text for scientific evaluation and linguistic mistakes. We read and re-read the transcripts and notes to determine the initial categories and parts of the interviews. In this regard, the related texts were shortened and condensed into the mentioned themes made by the researchers as the unit of analysis. We used the condensation concept to summarize the interviews in the determined themes. We obtained the content areas of the study based on the theoretical models of behavior change as suggested by McKenzie and Harris [20]. These models were adopted because the theoretical models of behavior change concentrate mostly on intention and self-efficacy rather than stress or psychological distress. The real life of the medical staff is characterized by external stressors, including the COVID-19 pandemic in 2020 [7, 21]. The segments were coded based on the four determining themes: distress, nervousness, lifestyles, and familial relations. The study adhered to the consolidated criteria for reporting qualitative research (COREQ) in the drafting of the study [22].
Ethical issues
The College of the Nursing/University of Duhok approved the protocol of this study and recorded it as number 9 in May 2020. We obtained a written signed consent form from all participants before the interview. We protected the confidentiality of the personal information of the medical staff.
RESULTS
In this study we included 12 HCWs, both males (n = 2, 16%) and females (n = 10, 83%) aged 21-41 years old (mean: 26; SD: 4 years) – see Table 1 for the general information of participants. The analysis of the data resulted in the following four themes: stress, feeling depressed, familial relations of medical staff, and lifestyle changes of medical staff during the quarantine period.
Table 1
General characteristics of participants
Stress during the quarantine period
Most participants experienced stress when they were being tested for COVID-19 on the first and last day of the quarantine. The stress of the participants was mostly due testing positive. They were afraid that they may have infected their family members. One participant remarked:
“I was so stressed to be tested positive for COVID-19. I had very high stress on the testing day. I was waiting for an unknown outcome. If I tested positive for the disease, maybe I lose my job at the private hospital. There are many unemployed nurses ready to work in this region.” (Participant 2)
Other participants reported similar experiences on the first and last day of the quarantine period. Most remarked that it would be a negative point for them to be tested positive for COVID-19. When we asked for further clarification on why being tested positive for COVID-19 would be a negative point for them, they reported that COVID-19 was at the early stage in this region and that it was a stigmatized disease locally.
Some participants felt stress due to fears for the well-being and life of their family members. They reported that they had old parents who might not be strong to fight the infection.
“I am so afraid that I have infected my mother and father. I work as a receptionist at public and private hospitals. I have contact with many patients who visited and were admitted to the hospitals. I went home and came back to the hospital. I felt guilty because I was afraid I may have infected my mother and father with the corona [COVID-19 disease].” (Participant 4)
Some surgeons suggested that they would be away from their private job for a long time if they were infected by COVID-19, and that this would impact the workload of their colleagues.
Feeling nervousness during the quarantine period
Most participants experienced nervousness at the beginning of the quarantine.
“I had no good impression at the beginning of the quarantine. I was so nervous because I was far from my family. It was my first time staying at a place for fourteen days. Also, the last day was so stressful for me, because we needed to take the test for COVID-19. I was so afraid to be tested positive.” (Participant 2)
Similar experiences were reported by participants 3-12.
Others remarked that they would be admitted to the hospital for three weeks if they had a positive test. In that case, they would be away from their family and job.
“I will be admitted to the hospital for three weeks to receive treatment if I test positive for COVID-19. This has made so bad an impression on me. I had these kinds of impressions throughout the quarantine time. It was the first time that I have been distant from my family. I have good impressions when I talk to my family and friends.” (Participant 7)
Similar experiences were reported by participant 8.
Only the first participant who was quarantined gave a favorable response. This was because she had a chance to have proper rest. She told us:
“I was so happy during the quarantine. I had so busy a time working at the hospital. But here I was so free and did not have to deal with the patients. I worked at the public hospital in the morning and the private hospital in the evening. I did not have sufficient time to sleep before quarantine time. During the quarantine, I could sleep and call my family members. I had no time to answer the contacts of my family members before this time.”
Coping mechanisms
Family relationships
The participants adopted several coping mechanisms (positive experiences) to maintain their healthy lifestyles. Maintaining familial relationships was the most common strategy. All of the participants had more positive relationships with their family members during this period. They spent more time talking to their families and their relationships became stronger. Most of them had not had adequate time to be with their family before the quarantine period. For example, participant number 4 stated:
“I found that I was so far from my family. Because I worked every day at public and private hospitals in the morning and evening, respectively. I finished my job at 10 pm every day. When I came back home, the members of my family were sleeping, and when I left for the hospital they were still asleep.”
Another participant told us that:
“I called my family members to spend the quarantine time [as a way of passing time during the quarantine]. The quarantine time was difficult and so long. I had too much time to call my family members and friends. Before the quarantine time I was always working at the hospital. I worked in a public hospital in the morning and a private hospital in the evening. Therefore, I had not sufficient time to spend with my family members and friends.” (Participant 1)
Although the participants did not have good experiences of the quarantine, their contact with their families was a strong feature in the reduction of their bad feelings and stress, particularly when they knew that their family members were safe.
Social media
Some participants spent their time watching movies and TV programs to kill time during the quarantine. This was a way for them to deal with the isolation, loneliness and anxiety during this period.
“I did not know how I should spend my time. Fourteen days was so long a time for me to spend at the hotel. So, I spent my time watching movies and TV. I did not watch TV or movies before the quarantine.” (Participant 1)
Similar experiences were reported by participants 6-9 and 12.
Religious activities
Some participants performed their religious observances to relieve the stress of the quarantine. The participants, as we have seen, had a high level of stress about test results – the consequences of positive one result were very stressful for them. Therefore, they used many coping mechanisms, and religious activities helped them to cope. For example, participant 3 reported that:
“I felt that I was becoming so depressed during the quarantine, and having to stay in a room for fourteen days. I started to perform my religious activities and I felt better.”
Reading books (other than religious books) was another coping strategy used by participants (Participant 3).
Lifestyle changes of HCWs
The lifestyles of the participants changed during the quarantine; with sleep being the first aspect to change. Most would sleep a lot during this time. Participant number 12 reported that:
“I worked as a nurse in a public hospital in the morning and in a private hospital in the evening. When I went back home at night, I was so tired I fell asleep directly. Now, I do not work in the morning and evening. I talk to my family at night. Sometimes, I do some activities on social media. But I do not have anything to do in the day and I sleep throughout it. I do not know how I can change my sleeping behaviors when I go to the hospital.”
Regarding their eating habits, the participants reported that their food choices did not change. Their families cooked food for them and brought it to the hotel, since they were not happy with the food there. However, their eating habits changed because they slept throughout the day. One of the participants mentioned:
“I did not eat breakfast at the hotel, because I was sleeping in the day. I was so sensitive to the food at the hotel. My family brought food for me. But my eating habits have changed since the quarantine time. I ate lunch later in the day Also, I ate dinner late at night. I felt that I was becoming obese here.” (Participant 6)
Another participant reported a similar problem during his stay at the hotel.
“I was at the hotel for fourteen days. I had no opportunity to do physical activity. I was becoming obese because I had lunch at late in the day and dinner too late at night.” (Participant 1)
Only two participants reported that their lifestyles and habits did not change.
DISCUSSION
This study showed that the participants faced distress due to difficult experiences during the quarantine period. The first and last days were stressful for them because they were afraid of being tested positive for COVID-19, and consequently having potentially infected their family members. The HCWs attempted to maintain healthy lifestyles, including getting sufficient sleep, reducing distress levels, and maintaining positive relationships with their families. The effects of the COVID-19 pandemic were alleviated by some coping strategies, including familial and social support.
A small number of previous studies have reported that HCWs experienced long-lasting depressive, posttraumatic stress, and alcohol dependency and abuse symptoms. They have a fear of infection and are concerned about their families and children [23]. Chen, Wang [24] documented the general health status of HCWs who cared for patients with SARS. They measure the general health status at the beginning of the study, four weeks later, after two weeks of self-quarantine, and after two weeks of off-duty shifts. The hospital administrators and employees with no history of quarantine or contact with SARS patients were considered a control group. It was reported that the HCWs have significantly and negatively changed physical role functioning, emotional role functioning, and social role functioning. Bai, Lin [25] reported quarantine as the factor most related to acute stress disorder in HCWs during the SARS pandemic. The quarantined HCWs were more likely to report exhaustion, anxiety, detachment, insomnia, irritability, poor concentration, fear of infecting family members, and deteriorated work performance. Prospective cross-sectional studies have shown that quarantined HCWs account for 60.0% of the persons with severely depressed symptoms [17, 26, 27] and are significantly more likely to have post-traumatic stress symptomatology [27]. Close to 10% of HCWs who worked during the SARS outbreak experienced high levels of posttraumatic stress symptoms in 2003. The quarantined HCWs who worked in SARS wards or had friends/relatives infected by SARS were two or three times more likely to report insomnia [28]. The possible difference between the findings reported in this study and the literature may be related to the shorter quarantine period of our study, which may not have been long enough for the HCWs to develop serious psychological problems. However, there was a stigma toward the infection by COVID-19 in this region at the early stage. Therefore, it might be that the HCWs were stressed on the first and last days of the quarantine time due to the presence of stigma towards the COVID-19 disease in our region.
Quarantine has been shown to be associated with stress, depression, unhealthy diet, and decreased physical activity [29]. The stresses of quarantine and social isolation have negative psychological effects on individuals, including increased stress and anxiety [16]. In addition, individuals have concerns for themselves and their loved ones, and the disruption of daily life and routine during stressful events. These stressful events could result in functional impairment and post-traumatic stress outcomes [30].
The factors that have been shown to contribute to psychological distress in HCWs who care for patients in isolation are risk perception, the outbreak’s impact on life, depressive effect, working in a high-risk unit, and caring for multiple patients [31]. Quarantines or lockdowns are implemented to prevent the spread of COVID-19 but they may cause different physical, psychological, social, and economic consequences. The people who faced social distancing, isolation, and lockdown suffer from very serious psychological problems such as anxiety, stress, fear, fear-induced over-reactive behavior, frustration, guilt, anger, boredom, sadness, worry, depression, helplessness, loneliness, insomnia, and depression [32].
The HCWs who were quarantined due to close contact with a confirmed case of COVID-19 were receiving their food from their families in this study. Therefore, we do not think that their eating behaviors have been negatively changed. However, we do not have clear information about their healthy and unhealthy food behaviors. Also, apart from the shortness of the quarantine period, the social relationships of the HCWs with their families and relatives and social media were a reason for their not having serious psychological problems.
The studies conducted in other regions of the world have reported worse situations, compared to this study. For example, research conducted among Italian doctors during the lockdown reported alarming psychological conditions, particularly among those who worked in the most affected regions. The prevalence of psychological distress and poor well-being was 93.8% and 58.9%, respectively. These prevalence rates were even higher among female hospital workers with low job seniority, and doctors who were caring for COVID-19 patients [33]. A similar study conducted in this region reported that the mean score for stress was raised significantly with and increased duration of dealing with suspected/confirmed cases of COVID-19 [7].
We need physically and mentally healthy and well-equipped HCWs to manage the COVID-19 outbreak. Therefore, a mental health initiative needs to be included in COVID-19 emergency plans [34]. The HCWs may show signs of psychological distress during a COVID-19 outbreak [35] and be reluctant to partake in psychological interventions [8].
The main concern and stress of the participants in this study was the fear of being positive for COVID-19. In addition, they were extremely anxious about possibly having infected their family members. The HCWs may be exposed to stigmatization and a loss of trust in our community [28]. The medical staff had a high degree of concern about being positive for COVID-19 on the first and last days of the quarantine. Some of the HCWs in our study had not previously faced being far from their family members. They could have had to spend more time away from their families. In addition, it seems that there is a stigma of infection by COVID-19 among medical staff in this region, and a positive result could have a further effect on their working status in the private sector.
We need to enhance the safety of HCWs and trust in the system to curtail the potential risk of nosocomial infection, as they may have a fear and anxiety about infection in the health system. It is necessary to mention that physical separation from or infrequent communication with families could result in family distress. The second author of this study, as the team leader, supported the staff psychologically during the quarantine because the people in isolation were significantly susceptible to neuropsychiatric complications due to limited space for physical movement [36].
The participants in this study were not found to be positive for COVID-19 two days after quarantine ended. However, quarantined persons are more likely to report distress owing to fear and risk of infection [37]. It is possible that the medical staff were unable to sleep during the night due to fear of being positive for COVID-19 and the stress of quarantine. Therefore, it is evident that they report changes in their lifestyles, such as sleeping and eating habits. It seems that health fears, social isolation, and job stress are the main factors that account for the quarantine’s impact [38]. A study from Singapore during the SARS pandemic showed that the following factors decrease posttraumatic stress: a) establishing clear communication of directives and precautionary measures; b) giving feedback to and obtaining support from management; c) support from supervisors and colleagues; d) support from the family; e) talking to someone about their experiences, and f) performing religious observances [39].
The participants reported that they tried to call their families and friends, engage in social media activities, watch TV, and play video games; a small number looked to their religion. In addition, the medical team created a social media group within which to spend their free time. All these activities may have been effective in reducing the level of stress they experienced. The participants used social media as an avoidance strategy to reduce their distress. Social media use has been determined as a primary means for people facing health issues. In this regard, persons under stress use social media as a means of relaxation and recovery [40]. However, we assume that a strong relationship with family members and friends was a key factor in alleviating their levels of stress. A study from Singapore found that doctors have a lower score for posttraumatic stress compared to nurses. The study reported that doctors were more likely to use humor as a coping strategy, whereas nurses used religion and spirituality as their coping mechanisms [41]. Communication is considered to be a way of fostering relations between frontline providers and their supervisors by heightening the sense of appreciation and support. Moreover, open communication means that the supervisors demonstrate concern for the staff ’s well-being [36]. In this study, the team leader was quarantined along with other staff due to contact with a suspected and later confirmed case of COVID-19 during a thyroid cancer operation. Therefore, the team leader continuously supported the team members psychologically. He also had continuous contact with them through the social media group. A qualitative study showed that external stress is moderated by some coping strategies, such as beliefs, habits, and social support, in general practitioners. In addition, the process of changing or maintaining healthy behavior could cause distress in some circumstances [20].
It is crucial to mention that socio-cultural factors affect stress perception [7, 42]. The effects of the COVID-19 pandemic on the mental health of HCWs can be different based on the country and its resources, the care activity carried out, and the time of evaluation [43, 44]. The people in this region have an acceptable level of social relations. To prove this point, the participants reported that their family members cooked food for them and brought it to the hotel. In addition, their friends and family members called them continuously. The social relations of the participants with their family members and friends could have had an important role in alleviating the stress faced by the team [21]. Similar findings have been reported among HCWs in Spain, where higher levels of distress were found in the geographic areas with the highest incidence of COVID-19 (> 245.5 cases per 100 000 people) [45].
However, it is noteworthy that most of the participants in this study were single females. In addition, the public had negative attitudes towards people diagnosed with COVID-19 at the early stages of the outbreak in this region. Therefore, being anxious of the participants during quarantine may associate with both their socio-cultural of our society and the stigma towards the COVID-19 disease. There was some kind of stigma evident around COVID-19 at the early stage of the outbreak in Iraqi Kurd-istan. Therefore, the first and fourteenth days of the quarantine were highly stressful for the participants. If they were positive on the first or fourteenth day they would be admitted to the COVID-19 hospital until being tested negative. Therefore, the HCWs were thinking about their duties at the hospital, university, and private clinics. They could lose some of their patients in the case of a long absence from a private clinic.
It is worth mentioning that these changes were not permanent among the HCWs. They were able return to their normal situation after the quarantine. But distress and nervousness are considered health issues among individuals under quarantine. Therefore, we need to manage these health issues through suitable strategies.
LIMITATIONS OF THE STUDY
We did not compare the findings of this study with a control group because later the situation escalated and the region went into a complete lockdown. In addition, the findings reported in this study may not be generalized to other clinical departments since medical teams have considerable differences. Also, no standardized tests measuring anxiety levels, intensity of stress or coping style, or symptoms of depression were used in this study. The quarantine period lasted only two weeks; this length of time may not have been sufficient to change the habits of respondents. We did not report the previous habits, well-being, and pathological symptoms of respondents in this study. The results of this study were very limited and subjective. Future research may profit from a more diversified and larger sample size.
CONCLUSIONS
Implications for Behavioral Health Quarantine periods during outbreaks of infectious disease can drive psychological distress in healthcare workers owing to social distance and separation from family members. We hypothesize that drawing on familial support could be used as a coping mechanism for moderating psychological distress. This study showed that HCWs experience psychological stress during their quarantine. The sleep status of the HCWs was affected adversely along with negative effects on their lifestyles. However, the HCWs used social and familial relations as coping mechanisms (positive experiences) to relieve the effects of the quarantined period.