INTRODUCTION
Firefighters are commonly exposed to severe stressors and traumatic experiences and are particularly at risk for developing symptoms of occupational burnout [1-3]. A large body of evidence originating from the studies of diverse occupational groups shows that burnout has a number of deleterious health and psychological consequences and may impair productivity and effectiveness at work [4-6]. Little is known, however, about the nature of the connection between burnout and work ability among firefighters and the mental health and psychosocial factors that may act as mediators in this relationship. Clarifying these issues may prove crucial for the planning of interventions aimed at preventing adverse effects of burnout on people who work in this demanding and hazardous profession.
Burnout and work ability
Burnout and work ability represent two important occupational health-related constructs. They both relate to the level of energy at an emploee’s disposal, and the resources that can be used to deal with the workload and that can be invested by a person at a given time [7]. While in the concept of work ability the emphasis is mainly on the physical aspects of work (e.g., job conditions, physical energy, the skills and functional capacities required to meet the workload) [8, 9], in the case of burnout the highly significant role of emotional/affective energy is underlined [4]. However, in both of these phenomena the balance between workload and available job resources is indicated as being beneficial to the worker.
According to the concept developed by the Finnish Institute of Occupational Health (FIOH), the term ‘work ability’ is defined as the balance between the physical, psychomotor and sensory abilities of an employee required to perform work (e.g., health, functional fitness and skills) and the demands posed by work [8, 9]. It is assumed that work ability is the result of an interaction between an employee, the type of task involved and the working environment [10]. More specifically, it is shaped by four groups of factors: health (physical, mental, and social), competences (e.g., knowledge and skills), values (e.g., work motives and attitudes), and the environment (e.g., workplace, type of work, requirements). Work ability is an element of the safety culture of the workplace and is treated as an important factor contributing to safer work which does not threaten the health and life of employees. Numerous studies on antecedents of work ability show that it correlates with higher age, harmful working conditions, and shift work [11, 12], as well as prolonged job demands [13-15] and insufficient job resources [16-19]. For example, a systematic review by van den Berg et al. [15] showed that both high job demands (related to physical and psychological demands) and low job resources (related to low levels of autonomy and poor ergonomic conditions) correlate with low work ability. Airila et al. [17], in turn, showed that resources (related to ‘good’ relations with a supervisor) were predictors of high work ability, measured ten years later, in a group of Finnish firefighters. The mediating variable in this relationship was work engagement. Work engagement is treated as the opposite pole of occupational burnout and defined as a positive, fulfilling, work-related state of mind that is characterized by vigor, dedication and absorption [20]. It is also theoretically a separate construct from work ability [17]; while work engagement refers to the motivational process in which the employee puts all his personal energy into physically, cognitively and emotionally struggling with the challenges of work [20], work ability refers to an employee having the professional competencies and level of health required to perform the job, and occupational virtues that are required for managing the work tasks [21].
Chronically high job demands and a shortage of resources are typical for workers with burnout. Occupational burnout is perceived as a long-term effect of work- related stress caused by excessive job demands, which are not modified by one’s own remedial activity [22]. Initially, burnout was defined as a complex of three symptoms (emotional exhaustion, depersonalization and reduced personal accomplishment) that affect human services professionals [23]. More recent models assume that each profession has specific risk factors which, in the face of insufficient resources, may lead to burnout [24]. In the present study, we adopted a two-dimensional definition of occupational burnout, suggesting that it consists of exhaustion and disengagement from work. The former is a response to intensive physical, affective and cognitive strain. It manifests itself in fatigue, weariness and a decrease in energy. In turn, the latter is expressed by distancing oneself from work and by experiencing negative work-related affect [24].
An inverse association between burnout and work ability has been demonstrated in several studies on various professional groups, such as teachers [25], human services professionals [26], nurses [27], flight attendants [28], early childhood educators [7], education employees [29] and medical staff [30]. However, the relationship between burnout and work ability and its possible mediators among firefighters have not been systematically studied to date. A better understanding of the health impairment process and the identification of key factors regulating the development of work ability can help in the design of early intervention programs for the prevention of the negative gain spiral between occupational burnout and low work ability. Any potential vicious circle of this kind could in turn lead to further negative consequences both for humans, organizations and the society in terms of health problems, absenteeism, job turnover, and diminished quality of service [31].
Mediators of the relationship between burnout and work ability
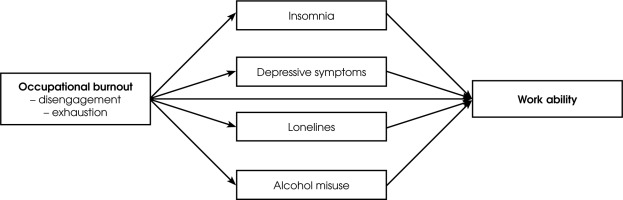
Given the above, in the present study our aim was to shed more light on the mechanisms of the effects of burnout on work ability among firefighters by exploring the roles of four candidate mediating variables: insomnia, depressive symptoms, loneliness and alcohol misuse. The relevant theoretical rationale and empirical research suggest that each of these mental health or psychosocial factors may be negatively affected by burnout [5, 6, 32-37]. On the other hand, all of these factors have been found to predict lower work ability, efficiency or performance [38-45]. This provides a basis for the assumption that insomnia, depressive symptoms, sense of loneliness and alcohol misuse may mediate the effects of burnout dimensions (i.e., exhaustion and disengagement) on the work ability of firefighters.
A hypothesized model is graphically presented in Figure I.
METHODS
Study design and sample
This is a cross-sectional study. The participants were 460 firefighters recruited from various Rescue Units of the State Fire Service in the following provinces of Poland: Kujawsko-Pomorskie, Śląskie, Lubelskie, Wielkopolskie, Podlaskie, Podkarpackie, Zachodniopomorskie, Pomorskie, Warmińsko-Mazurskie, Opolskie, Mazowieckie and Lubuskie. The inclusion criteria were age: 20-55, male subjects, health condition suitable for active service. The exclusion criteria were refusal to give informed consent and termination of professional activity (e.g., retirement pension, disability pension, change of occupation). Data were collected between 20 April 2021 and 28 August 2021.
The background characteristics of the participants are presented in Table 1.
Table 1
Characteristics of the sample of professionally active firefighters (N = 460)
Measures
Burnout
Occupational burnout was assessed with the Oldenburg Burnout Inventory (OLBI) [46, 47]. It consists of 2 subscales – exhaustion (8 items) and disengagement from work (8 items). The responses to each statement are rated on a scale from 1 (strongly agree) to 4 (strongly disagree). After recoding reversed items, higher scores on the two subscales denote more severe symptoms of burnout. In this dataset, Cronbach’s α was found to be 0.835 for the exhaustion subscale and 0.775 for the disengagement subscale.
Work ability
Work ability was measured by means of the Work Ability Index (WAI) [9, 48]. For the purposes of this research, a general indicator of work ability was used, assessed with a single question asking the respondents to mark on a scale ranging from 0 to 10 their current work ability compared with the lifetime best.
Insomnia
The Athens Insomnia Scale (AIS) was used to evaluate the severity of insomnia symptoms. The tool was developed by Soldatos et al. [49] and validated in Polish by Fornal- Pawłowska et al. [50]. This eight-item questionnaire taps into symptoms of insomnia and their effect on daily functioning. An increase in the total score indicates an increase in the intensity of the insomnia. It was demonstrated that the optimal cut-off score for insomnia according to the ICD-10 criteria is 8 [50]. Cronbach’s α for the AIS was 0.846.
Depressive symptoms
The Center for Epidemiologic Studies Depression Scale-Revised (CESD-R) [51], adapted to Polish by Świtaj et al. [52], contains 20 items referring to the various symptoms of depression. Respondents are asked to indicate how often they ‘have felt this way in the past week or so’. Response options range from 0 (not at all or less than 1 day) to 4 (nearly every day for 2 weeks). The higher the total score, the more severe the depressive symptoms (Cronbach’s α = 0.936). A score equal to or above 16 indicates persons at risk for clinical depression.
Loneliness
The De Jong Gierveld Loneliness Scale (DJGLS) [53, 54] consists of 11 items, to which interviewees are asked to respond by using a five-point scale ranging from 1 (yes!) to 5 (no!). It can be used to assess both the overall level of loneliness and the two of its dimensions: emotional (6 items) and social (5 items). After recoding the items that refer to the emotional aspects of loneliness, a higher total score signifies a more intense global sense of loneliness. The scale had a very high internal consistency (Cronbach’s α = 0.911).
Alcohol misuse
The CAGE questionnaire [55, 56] was utilized to determine the severity of alcohol misuse. It is a simple and easy-to-use self-report instrument composed of 4 questions, with the scores of 0 for ‘no’ and 1 for ‘yes’. Thus, the total score ranges from 0 to 4, with higher ratings indicating greater alcohol problems. A score of at least 2 suggests alcohol abuse. In the present study, Cronbach’s α for the CAGE was 0.722.
Procedures
The ethical approval for the study was granted by the Bioethical Committee at the Institute of Psychiatry and Neurology in Warsaw. All participants provided their written informed consent. The measures were administered by psychologists of the Psychological Assistance System in the State Fire Service; however, respondents could also fill in the questionnaires personally if they wished to do so. The participants answered a set of questions regarding their background socio-demographic and occupational characteristics (where necessary, the information was supplemented or verified by psychologists).
Statistical analyses
Data analyses were conducted in JASP 0.14.1 (University of Amsterdam, Netherlands). Each binominal variable was presented as prevalence in the sample – in both an absolute (number of observations, n) and relative way (percentage, %). Each continuous variable was characterized as mean (M) with standard deviation (SD). For continuous variables, the distribution was assessed with the Shapiro- Wilk W test and the analysis of the Q-Q plots of the residuals. Cronbach’s α coefficients were calculated to evaluate the internal consistency reliability of the measures used in the study. Bivariate associations between the scores on the instruments administered to respondents were initially checked with Pearson product-moment correlations. After initial assessment of the correlation coefficients, a mediation model was created, with burnout dimensions, i.e. the OLBI subscales scores, considered as predictors, work ability (the WAI score) as an outcome, and the following variables considered as mediators: insomnia (the AIS score), depressive symptoms (the CESD-R score), loneliness (the DJGLS score) and alcohol misuse (the CAGE score). All paths in the model were adjusted for: marital status, place of residence, education level, length of service, number of firefighting actions per month, number of working hours per week, worktime system, qualifications, functions, workplace, and financial situation. Bootstrapping, with sampling set at N = 1000, was performed to empower the results and account for possible non-parametric distribution. The confidence intervals (CI) were computed using the bias-corrected percentile method as suggested by Biesanz et al. [57]. Statistical significance was defined as p < 0.05 or CI not encompassing 0.
RESULTS
Taking into account the cut-off scores adopted for the AIS, the CESD-R and the CAGE, 22% (n = 99) of our sample could be classified as having insomnia, 15% (n = 71) as being at risk for clinical depression and 12% (n = 57) as having alcohol problems. Table 2 presents descriptive statistics and intercorrelations for the instruments utilized in the study.
Table 2
Means, standard deviations, and intercorrelations (Pearson's r) for the instruments used in the study (N = 460)
OLBI-E – Exhaustion subscale of the Oldenburg Burnout Inventory, OLBI-D – Disengagement subscale of the Oldenburg Burnout Inventory, WAI – Work Ability Index, AIS – Athens Insomnia Scale, CESD-R – Center for Epidemiologic Studies Depression Scale-Revised, DJGLS – De Jong Gierveld Loneliness Scale, CAGE – a four-item screening tool for alcohol misuse. For all instruments, higher scores indicate higher levels of the measured constructs.
All the appointed mediators correlated significantly at the level of p < 0.001 with both predictor and outcome measures. Thus, the mediation model was constructed as planned. The results of the mediation analysis are summarized in Table 3.
Table 3
Summary of the assessment of total, direct and indirect effects of burnout on work ability in the sample of firefighters (N = 460)
OLBI-E – Exhaustion subscale of the Oldenburg Burnout Inventory, OLBI-D – Disengagement subscale of the Oldenburg Burnout Inventory, WAI – Work Ability Index, AIS – Athens Insomnia Scale, CESD-R – Center for Epidemiologic Studies Depression Scale-Revised, DJGLS – De Jong Gierveld Loneliness Scale, CAGE – a four-item screening tool for alcohol misuse.
Standardized estimates are presented (from linear regression models), with 95% confidence intervals (CI), derived from bootstrapping with N = 1000 sampling. The model was adjusted for marital status, place of residence, education level, length of service, number of firefighting actions per month, number of working hours per week, worktime system, qualifications, functions, workplace, and financial situation.
The coefficient of determination (R2) for the whole model was 0.444. This may be interpreted as 44% of variance in the WAI score being explained by the proposed mediation model. A rise in the OLBI Exhaustion and Disengagement scores predicted a fall in the WAI score. These effects remained statistically significant when controlled for the mediators. Both the CESD-R and the DJGLS scores turned out to be partial mediators of the association between the OLBI Exhaustion subscale and the WAI, and between the OLBI Disengagement subscale and the WAI. The mediating effects of the CAGE score and the AIS score were statistically non-significant. The observed effects were independent of marital status, place of residence, education level, length of service, number of firefighting actions per month, number of working hours per week, worktime system, qualifications, functions, workplace, and financial situation.
DISCUSSION
In this paper, the nature of the relationship between occupational burnout and work ability was analyzed on a relatively large sample of firefighters. As expected, a strong negative direct effect of the two burnout dimensions (i.e., exhaustion and disengagement) was found on work ability. The direct link between burnout and work ability can be well explained in the light of Conservation of Resources (COR) theory [58, 59]. COR theory posits that the overriding goal of human activity is the acquisition, preservation and protection of valuable objects, i.e., resources [58]. Thanks to them, it is possible for the individual to survive, as well as to obtain other desired ‘goods’. Resources therefore play a key role in assessing and interpreting life events as stressful (or not) and regulating ways of dealing with them. COR theory also assumes that people must constantly invest their resources in order to acquire new ones or to compensate for the loss of some resources [60]. This assumption has several important practical implications. First, people who have a ‘rich’ pool of resources are not only more likely to make a profit in the future but are also less likely to lose them. Secondly, those who have resources feel more secure and therefore invest them more offensively, thus increasing their pool of resources, while those who do not have them tend to be defensive and try to protect what they already have [60]. Third, initial success in acquiring resources may lead to further successes (the so-called positive gain spiral), while the initial loss of resources is often associated with subsequent losses (negative loss spiral).
In the context of work, job resources are factors that facilitate employees’ professional development, help achieve work goals and reduce their physiological and psychological costs related to workload [61]. They also play a key role in the development of both job burnout and work ability [62]. According to the COR theory, employees with few job resources will be more likely to experience a loss spiral, while those with a high level of job resources will have greater opportunities to expand their pool. Loss spirals, as explained by Hobfoll [59], occur when resources are exhausted and are therefore not available to deal with future risks of loss, potentially leading to further losses. A characteristic feature of burnout is the progressive process of depletion of motivational and energy resources, which cannot be replenished [61]. Inability to rebuild one’s own resources, along with constant attempts to meet high job demands, may lead to impaired occupational functioning and a deterioration of the physical (e.g., endocrine disorders caused by the autonomic nervous system) [63] and mental (e.g., affective disorders) [62] health of workers, thus reducing their ability to work [61].
In this context it needs to be mentioned, though, that the direction of the cause-effect relationship between burnout and work ability is not entirely clear. Some longitudinal studies suggest that burnout is the cause of low work ability [25, 26, 64]. For example, in an eight-year cohort study among forest industry workers, Ahola et al. [64] reported that exhaustion and cynicism measured at the baseline predicted work ability measured at the follow-up. There are also empirical data showing the direction of this link to move in the opposite way [7, 65]. However, it can be assumed that the relationship between burnout and work ability might be bidirectional rather than unidirectional, and that there is a specific negative gain spiral between the two phenomena. This is evidenced by the results of research on the association between work ability and work engagement (as a phenomenon complementary to burnout), which found that work engagement measured at Time 2 mediated the relationship between work ability measured at Time 1 and work ability measured at Time 2, ten years later [17].
Our hypotheses regarding the mediating roles of insomnia, depressive symptoms, feelings of loneliness and alcohol misuse in the relationship between burnout and work ability were partly supported by the data. In the light of Hobfoll’s COR theory [58, 59], all four mediating factors considered can be conceived as different forms or manifestations of loss of resources, which may result from burnout and contribute to poor work ability. However, we found that only depressive symptoms and loneliness were partial mediators in the associations between both exhaustion and disengagement with work ability. The mediating effects of insomnia and alcohol misuse were not confirmed.
The character of the relationship between burnout and depression and their discriminant validity have been the focus of extensive research and vivid theoretical debate [4, 6, 66-68]. Nonetheless, the prevailing view is that the two are related but distinct constructs [67, 68]. Furthermore, although the relationships between them are obviously complex, depression is regarded as a likely consequence of burnout [4, 6]. This was confirmed in a systematic review of physical, psychological and occupational consequences of burnout performed by Salvagioni et al. [5], which revealed that burnout significantly predicted depressive symptoms or antidepressant treatment in the majority of the prospective studies included that investigated the psychological consequences. In turn, depressive symptoms (including low energy, fatigue, lack of interest and motivation, and cognitive impairment) have been demonstrated to negatively affect work efficiency and ability [41, 69]. Against this background, our findings provide empirical evidence for and support the notion that the intensification of depressive symptoms is one of the routes through which burnout exerts its harmful effects on the work ability of firefighters.
With respect to employees’ loneliness, i.e., subjectively perceived social isolation, it has been argued that it may not necessarily result from objective social isolation, but rather may be due to exhaustion related to occupational burnout [34, 36]. In line with this assertion, a study by Shapiro et al. [70] revealed that in a sample of internal medicine residents, burnout was associated with loneliness in a dose-response fashion. Previous research also showed that loneliness may predict a variety of negative occupational outcomes, such as work disability, unemployment, absence from work or work inefficiency [41, 42, 71]. The present study contributes to this area of research by showing that loneliness may partly explain a disadvantageous impact of exhaustion and disengagement on work ability among firefighters.
As far as insomnia is concerned, it is a relatively common condition that may vary in its severity. It is both a risk factor for and one of the symptoms of depression [72]. In this study, it can be seen that insomnia symptoms correlated with both burnout and work ability, but the association did not hold in a multifactorial mediation model. It should be noted that the AIS score was correlated with depressive symptoms even more strongly (r = 0.615, p < 0.001) than with burnout and work ability. Thus, there is a possibility that the detrimental effect of insomnia on work ability may be limited to those cases in which an individual suffers concurrently with other depressive symptoms. Additionally, it is worth mentioning that the AIS was designed to screen for insomnia according to the ICD-10 criteria and may not be optimal for the measurement of the severity of insomnia symptoms. It is much less sensitive than, e.g., the Insomnia Severity Index (ISI) [73] for subthreshold insomnia. Hence it would be desirable to replicate the findings using other measures of insomnia severity.
Finally, regarding alcohol misuse, the data from the literature provide rather limited and not entirely consistent evidence for its relationship with burnout [6]. In our study, correlations of burnout dimensions with alcohol misuse turned out to be much smaller than the correlations of burnout with other potential mediators. The same refers to the correlation of work ability with alcohol misuse. Thus, it comes as no surprise that the contribution of depression and loneliness to the investigated mediated effect proved to be much stronger than that of alcohol misuse. However, the results obtained may have been affected by the fact that alcohol misuse was assessed with the CAGE, which is merely a screening tool [55]. It is possible that the utilization of a questionnaire which would allow for the stratified assessment of the severity of alcohol problems, e.g., the Alcohol Use Disorders Identification Test (AUDIT), is required to verify the relationship between burnout, alcohol misuse and work ability [74].
Our current findings may have relevant practical implications and point to a combination of depressive symptoms and loneliness as potential targets of interventions aiming to alleviate the deleterious impact of occupational burnout on the work ability of firefighters. Therapeutic programs devised in this way should be verified in clinical trials, similarly to interventions found to be effective in reducing loneliness [75] or depression [76] among workers who are at high risk of burnout. In addition to alleviating the negative effects of burnout, such therapeutic programs should also include preventive elements. In this context, it is about enriching both the work environment and the employees (firefighters) with resources that facilitate coping with high job demands (e.g., support from coworkers, leadership and self-efficacy). Rich job-related and personal resources enable both professional development, by achieving professional goals, and – by reducing the job strain – minimize the risk of burnout. Before implementing such preventive programs, it is also worth taking a closer look at the causes of loneliness in firefighters. Do they have an individual basis and result from the employee’s personality tendencies (e.g., strong neuroticism), or are they mostly related to external factors, such as, e.g., excessive workload or being excluded by colleagues at work? Recognition of the sources of loneliness has remarkable consequences for the type of interventions undertaken. Since feelings of loneliness are important in the context of work ability, it is worth identifying people prone to perceived social isolation early on, in the recruitment phase, in order to provide them with special support from other members of the organization. However, if the sense of loneliness is related to problems of adapting to the group or social exclusion, perhaps such a preventive program should be extended to entire teams of firefighters. The issue of the sources of loneliness in the workplace should also become the subject of detailed research in the future. As the results of this study indicate, it has significant consequences for the functioning of employees.
The study has limitations that need to be acknowledged. Most importantly, a cross-sectional design precludes drawing definite conclusions regarding the direction of the relationships observed. It should also be remembered that the research sample included men only. This is due to the fact that the firefighter profession is typically male; however, it is likely that conducting studies among women (or in traditionally female professions) would yield different results. Hence, any attempt to generalize the results for the entire population should be made with great caution. Next, we only used self-report instruments to assess the constructs of interest. Furthermore, the mediation model that was tested did not address possibly complex interrelationships between the candidate mediators. Additionally, no moderation effects were controlled for in the study, both with respect to job characteristics and to personality variables. It seems that rich job resources (such as leadership, social support, or job control), as well as personality traits (such as hardiness or self-efficacy) may help counter the development of the two components of burnout and buffer their harmful effects on mental health. In future research, it is worth investigating alternative, serial mediation models assuming a causal chain linking of the selected mediating variables as well as testing moderation effects. Finally, it cannot be ruled out that other variables, which were not taken into consideration in the present study, may also act as mediators in the association between burnout and work ability.
CONCLUSIONS
Despite the reservations listed above, we believe that our analyses are a novel contribution to the understanding of the role of burnout in the firefighting profession. In summary, we demonstrated that burnout may undermine the work ability of firefighters. Its harmful effects are both direct and indirect, partly mediated by depressive symptoms and loneliness. These are, however, modifiable factors that need to be addressed in comprehensive anti-burnout interventions. Such interventions should be routinely offered to this professional group in order to prevent the loss of work ability and impairment of job performance.