INTRODUCTION
Value stream mapping (VSM) aims to identify unnecessary activities that can be minimized or eliminated without negatively affecting the overall treatment process. The core principles for implementing more efficient healthcare services include placing the patient at the center of service coordination, identifying value from the patient’s perspective, and eliminating activities that fail to provide value – essentially targeting areas of waste that prolong treatment time.
The lean management concept according to J.P. Womack and D.T. Jones [1] is based on the following principles:
defining the value of a product or service from the customer’s perspective;
identifying the activities necessary to develop a new product, from the concept stage to market launch;
eliminating waste, i.e., all activities that do not add value to the product or service;
operating on the assumption that the activities that cannot be properly measured, cannot be properly managed; similarly, tasks required to create, order, and produce a product that cannot be precisely identified, analysed, and integrated cannot be improved or perfected [2].
The project anticipates that medical entities in Poland will be encouraged to establish an internal system for monitoring the quality and safety of the healthcare services they provide. As part of the internal quality monitoring system, the authorities in charge of hospitals will implement solutions for identifying and managing risk. These solutions will require hospitals to analyze root causes, which is essential for detailed analyses of adverse events.
The analysis aims to provide an understanding of the circumstances and behind adverse events. By modifying procedures, the system will help prevent similar incidents in the future.
The first step in lean thinking is working on a precise definition of value. Delivering the wrong product or service in the right way is, in this model, referred to as muda [2]. Flow is enhanced when the focus is on the product and its needs, rather than on the organization or devices. This approach ensures that all activities needed for designing, ordering, and delivering the product occur in one continuous stream [2].
In 2017, approximately 6.2 million people worldwide died from stroke (including 2.7 million from ischemic stroke), and 130 million life-years were lost (DALY) due to premature death or health impairment caused by stroke (including 55 million of those attributable to ischemic stroke). These data are sourced from the Institute of Health Metrics and Evaluation, an organization which has been closely cooperating with World Health Organization since 2018 on collecting and improving global health data. Stroke is the second leading cause of death, following heart diseases. In 2013, stroke caused nearly 12% of all deaths globally [3], and in 2017, the percentage rose to 13%. In 2013, both the DALY and mortality rates from stroke in developing countries were statistically significantly higher than in developed countries. While the mortality rate from stroke in developed nations nearly halved between 1990-2013, it only decreased by approximately 15% in developing countries [4].
The disability rate among stroke survivors is equally concerning. In highly developed countries, about 50% of stroke remain disabled, while in Poland, the rate is 70%. Within five years of the first stroke, one in five patients will experience another stroke or a heart attack. In Poland, there has been no noticeable decline in stroke- related mortality and disability, making stroke prevention particularly urgent and critical.
As experience shows [5], the prognosis for ischemic brain stroke can be significantly improved with timely diagnostic, therapeutic, and treatment procedures. Time is one of the most crucial factors in this process. Promptly transporting the patient to the hospital and conducting essential diagnostic tests enables the initiation of appropriate therapies, significantly reducing the risk of early complications.
The purpose of this article is to assess the potential and usefulness of applying VSM to the process of treating stroke patients in the Polish healthcare system, as exemplified by the Institute of Psychiatry and Neurology (IPiN).
The standard process for treating patients at risk of stroke consists of four stages. It begins at the place of the primary healthcare level by identifying risk factors, followed by preventive measures for at-risk patients. In the event of stroke symptoms, the next stage involves the period until the patient is admitted to the hospital. The third stage begins upon admission to the neurological stroke unit, where hospital treatment typically lasts 7-9 days. After this stage, i.e., upon discharge from the hospital, the final stage of treatment, rehabilitation, follows, depending on the patient’s specific needs.
METHODS
This study was conducted as part of the Lean Management in Healthcare project, whose main goal was to develop National VSM Standards and pilot the implementation of tools for measuring the value stream in the patient treatment process.
A typical project for organizational and structural improvements in lean management within hospitals consists of five stages:
establishing a lean team, selecting the process for VSM, and gathering data;
developing the current state VSM map;
developing the future state VSM map, along with suggestions for improvements;
creating a “pathway to implementation”, which is a schedule of tasks leading to the implementation of improvements and achieving the desired state;
estimating the potential effects of implementation and installing a system for measuring and monitoring task execution for continuous process improvement (Kaizen).
Recording patient handling time within the service delivery points (SDPs) and resource utilization time enables the calculations of the added value stream. The resource cost calculations were based on data from the following areas:
Below is the description of the facility where the research was conducted using the process mapping tool.
RESULTS
The IPiN is a scientific institute dedicated to developing innovative methods for treating and rehabilitating neurological and psychiatric disorders. It operates two neurological clinics with a total of 80 beds, treating approximately 3,500 patients annually, of which about 900 are stroke patients.
The treatment process for stroke patients begins with their admission to the reception area, where, vital parameters are secured and basic laboratory and neuroimaging diagnostic tests are performed. The patient is then transferred to the intensive care neurological unit, where thrombolytic treatment and/or mechanical thrombectomy are administered to those who meet the qualifying criteria, along with diagnostic procedures to determine the cause of the stroke. Rehabilitation is carried out concurrently.
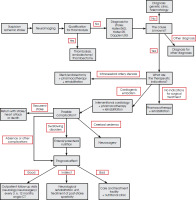
The chart outlining the treatment process for stroke patients is presented in Figure I.
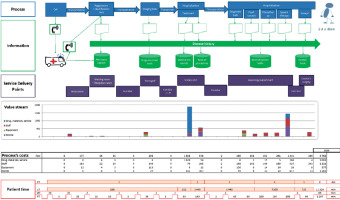
Information flow and value stream
The information flow begins with the patient’s call to emergency services, followed by a phone call from the ambulance informing the hospital about the transport of a stroke patient. The reception collects basic information about the patient, including the most crucial information on the time elapsed since the onset of stroke symptoms. Once the patient is admitted to the hospital, their medical history becomes the primary tool for collecting and recording information in their medical records. Within the hospital, information exchange is facilitated through an integrated computer system, where all medical events are logged, and notifications are sent to the appropriate medical staff.
The established added value stream for the future state VSM of stroke treatment at IPiN amounts to PLN 5,762 per patient. For the 1,200 stroke patients planned in the 2017 budget, the total cost of resources used in the value stream was PLN 6,914,598. This reflects only the direct costs of the utilized resources. To calculate the total cost of stroke treatment, the following cost categories should be added to the direct costs:
readiness costs (preparedness patient arrival);
departmental costs (allocated shared areas and auxiliary staff);
general hospital and management costs;
weighted average cost of capital.
For auxiliary, maintenance, administrative, and management processes in hospitals, it is necessary to map and calculate value streams using methods suitable for these types of processes. While the same analytical tools are used, these maps differ significantly from VSM for patient treatment processes.
Value stream map – future state
In this section, we will focus on the third stage: the development of the future state map, as part of the analysis of the hospital treatment process for stroke patients, conducted according to the assumptions of the Lean OZ project [6].
A classic VSM in healthcare consists of diagrams representing three streams of flow: patients, resources, and information [7]. Among these “patient flow” is crucial for value increment. The value stream map (Figure II) presents a graphic visualization of the future state of the stroke patient treatment process at IPiN, highlighting key indicators and parameters critical for managing this process. Given the reference nature of the two stroke units at IPiN, it is important to note that the diagnostic and treatment pathway for a stroke patients aligns with the guidelines of the Polish Neurological Society, the expertise of the treatment teams and the significant involvement of IPiN staff in the development of Polish stroke guidelines [5].
Statistical analysis of stroke patients’ hospital stay
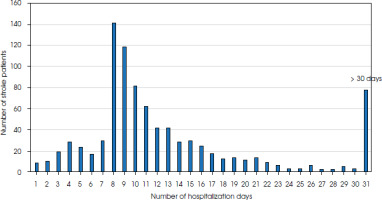
The statistical analysis of hospital stays for stroke patients reveals the highest demand for 8-day hospitalizations, with over 140 patients annually. This is partly enforced by the structure of diagnosis-related groups (DRGs), which financially discourage shorter stays. From the 9th day of hospitalization onwards, the number of patients gradually decreases, with only 3-4 patients annually staying 30-day. In total, 78 patients were hospitalized for more than 30 days, with the average length of stay for these patients being 54 days. The longest stay recorded was 178 days. Additionally, 140 patients had relatively short stays (1-7 days) within the analyzed 12-month period. The median length of stay for stroke patients is 16 days, and the arithmetic mean is 15 days (Figure III).
DISCUSSION
The analysis conducted suggests a potential division of stroke patients into two groups based on the length of their hospital stays:
714 patients with a stay from 1 to 16 days (fast-track hospitalization);
197 patients with a stay longer than 16 days (slow-track hospitalization).
The division into two distinct value streams is feasible due to the operation of two independent neurological clinics at IPiN:
Importantly, the division can be achieved primarily by shifting “standard patients” to Department 1 and moving “non-standard patients” to Department 2. This shift is expected to lower the existing VSM indicators in Department 2, moving them significantly below the average. This change will be the department’s new specialization in treating more complex cases.
Furthermore, Department 2 will undergo modifications to accommodate these new responsibilities. As the number of patients treated annually decreases, the staff in Department 2 will have more time to focus on diagnosing of patients with complications and coexisting conditions, as well as implementing specialized, non-standard treatment methods.
In the next stages of improvements, an optimization strategy is proposed, involving temporary personnel exchanges between Department 1 and Department 2. These exchanges which help staff gain additional experience, enhance their qualifications and ensure the duplication of key skills across the departments. This approach aims to increase the flexibility of the neurological departments, a key feature of mature organizations managed by value stream principles [6].
A concerning phenomenon is the prolonged hospitalization of many patients (over 30%) – beyond 8 days, which is considered optimal by the payer (National Health Fund – NFZ). Addressing this issue is critical for improving hospital efficiency and aligning with payment guidelines.
The primary sources of information to create the value stream map were gemba walk observations, where the patient’s treatment path is followed, and interviews with the medical and administrative staff involved in the patient care and service provision. Supplementary information came from financial and accounting data, including generic costs at specific service delivery points, a registry of fixed assets and equipment, personnel and payroll records, and medical statistics (including data on patient numbers, procedures, and diagnoses).
CONCLUSIONS
The VSM for the future state of the stroke patient treatment process at IPiN illustrates the treatment flow, incorporating the improvement opportunities identified during the analytical work. A key issue highlighted is the excessive patient transport times, which are caused by the distance between the most critical service delivery points, i.e., the reception area, imaging diagnostics, and the stroke unit and their location at different floors of the hospital building.
A proposed solution is to divide stroke patients into two streams:
standard patients (fast track, without complications);
non-standard patients (slow track, with complications).
Separation of standard patients and implementing a fast therapeutic track offers several benefits, including adherence to and completion of planned procedures within the expected waiting time, predictable information flow, monitoring of appropriate indicators, stabilizing costs at a predictable level. Ideally, it should take place at the level of the Emergency Department/Admission Room and can be applied in any hospital with a neurological/stroke department.
Meanwhile, the segregation of non-standard patients and transferring them to the slow therapeutic track will enable the completion of all planned and unplanned procedures. However, a bottleneck in the treatment process of stroke patients exists due to the limited number of beds in the neurological department, which requires attention for optimizing patient flow.
The presented value stream mapping process can serve as groundwork for developing standardized guidelines for managing stroke patients in hospitals.