Introduction
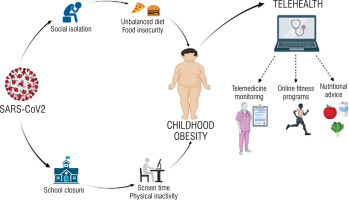
According to the World Health Organisation (WHO), in 2020, 39 million children under the age of 5 years were overweight or obese, and the incidence of obesity among people aged 5–19 years increased from < 1% worldwide in 1975 to 6% in girls and 8% in boys in 2016 [1]. Obesity and overweight may be associated with problems with physical and mental health, and they can affect the quality of life in childhood and increase the likelihood of being overweight and having life-limiting comorbidities in adulthood [2]. Further increases in childhood obesity could translate into serious health and economic challenges and even vulnerability to viral pandemic outbreaks such as COVID-19. Recently, before the outbreak of the pandemic, overweight and obesity levels remained at a constant level in many highly developed countries [3]. However, during the pandemic, a significant increase in obesity was observed in many countries [4, 5]. In an American study in Massachusetts, which assessed the impact of the lockdown on weight status among children in the US, anthropometric measurements of 701 children were analysed before and after the COVID-19 lockdown. During the COVID-19 lockdown, BMI, obesity, and overweight burdens increased, particularly in younger and Spanish-speaking populations. It is interesting that the youngest age group (2–5 years) had the greatest obesity rate increase (26%) compared to other age groups [6]. Behavioural, psychosocial, and environmental changes, which, through a variety of mechanisms, led to widespread rapid weight gain amongst certain populations worldwide. This phenomenon was named ‘covibesity’ [7]. Obesity increases the risk of the development of metabolic syndrome, cardiovascular disease, childhood-onset type 2 diabetes mellitus, and its associated complications [8]. The incidence of type 2 diabetes mellitus (T2DM) in children and adolescents has been growing in recent years [9], which, combined with the increased incidence of obesity in children, is a prognostic phenomenon of particular concern, although the incidence of T2DM is still quite low. As predicted by the SEARCH for Diabetes in Youth study, the number of adolescents with T2DM in 2050 is likely to increase 4-fold compared to the 2010 level [10]. Data on the increase in the incidence of diabetes come mainly from non-European countries (mainly the US). Excessive adipose tissue, deficit in lean mass, insulin resistance, dyslipidaemia, hypertension, high levels of proinflammatory cytokines, and low intake of essential nutrients are factors that compromise the functioning of organs and systems in obese individuals. Obesity was a highly prevalent comorbidity in severe cases of COVID-19 in children and adolescents [11]. Non-obese children were usually asymptomatic and even less susceptible to the infection [12]. The COVID-19 pandemic has affected various aspects of life [13]. Families, including children, had to adapt their daily lives to new circumstances. A recently published literature review by Stavridou et al. [14] showed that the main and basic cause of an increase in obesity rates in children and adolescents was school closure, along with other coronavirus 2019 (COVID-19) restrictions that disrupted the everyday routine of children, adolescents, and even young adults, leading to changes in their eating behaviours and physical activities. A review by Kharel et al. [15], which included 71 studies reporting data from 35 countries, compared how COVID-19 restrictions affected children’s and adolescent’s habits. Most studies reported reduced physical activity, increased screen time, and longer sleep hours among children and adolescents. Interestingly, the experiences of individual countries were slightly different: the decrease in physical activity and the increase in time spent in front of the screen depended on the imposed restrictions: usually, the stricter the restrictions in force in specific countries, the greater the effect. The most important observations are presented below.
Physical activity
Thirty-four studies found changes in physical activity among healthy children and adolescents. In 25 of them, a decrease in physical activity was observed (the highest among children from Spain and Brazil). It is worth adding that these were the most affected countries by the COVID-19 pandemic, which translated into a large number of deaths, infections, and severe restrictions. In some countries, physical activity did not change; for example, 8 studies from Italy, China, Australia, and Poland observed no significant change in physical activity levels from before to during the lockdown among children and adolescents [15]. The situation was different in various countries; surprisingly, German children were more physically active during the COVID-19-related restrictions than before the pandemic. The restrictions related to the pandemic in Germany were moderate, which allowed for outdoor physical activity with appropriate social distancing. Moreover, physical activity decreased especially with higher age of children and with lower socioeconomic background. Thus, the COVID-19 pandemic worsened the trend of inactivity, which was alarming even before the pandemic [16]. In one study [17] it was also noted that restrictions related to COVID-19 had a negative impact and lowered the level of physical activity only in previously physically inactive students and in those who were moderately active, while physically active young people increased their level of activity during and after the introduction of restrictions. A Polish multicentre study by Zachurzok et al. [18] showed that daily physical activity was affected by the pandemic leading, to an increase in body mass index (BMI), especially in obese patients with endocrine disorders. Following the first COVID-19 pandemic lockdown, the BMI z-scores of children increased significantly, especially in males. When comparing obese and non-obese subjects, an increase in BMI z-score occurred in both subgroups; however, only in obese children was the increase significant. Similar findings were observed in other countries deeply affected by the COVID-19 pandemic [18]
Exposure to screen
In 31 studies comparing screen time, there was a sharp increase, varying from 55 minutes a day, to almost 3 hours a day in Spain [15]. Singaporean and German children spent 1.54 hours and 1.02 hours more, respectively, on-screen during the pandemic than before the pandemic. Nine out of 10 Italian children also spent more hours in front of the screen. Also, aq Polish study revealed a dramatic increase in children spending more than 5 hours per day using computers and other electronic devices during the pandemic [18].
Sleep duration, bedtime, and wake-up time
Twenty-five studies reported changes in sleep duration among children and adolescents from before to during the pandemic [15]. Twelve studies reported an increase, 2 reported a decrease, and 11 reported no significant change in sleep duration. In Spain, children slept for about 45 minutes longer both during the week and at the weekend. Research from the UK indicated that children during the lockdown slept less than before the pandemic. All of them reported that children and adolescents went to bed later and woke up later during the COVID-19 lockdown than before the lockdown. Sixty-nine per cent of Italian children and adolescents reported having more difficulty in falling asleep during the lockdown. In contrast, Chinese pre-schoolers and teenagers had better quality sleep during the COVID-19 lockdown compared with before the pandemic. Children in Canada and Poland also experienced better quality sleep during the lockdown. According to the study by Zachurzok et al. [18], during the lockdown more children from Southern Poland slept more than 8 hours and slept less than 6 hours than before.
Diet
Consumption of both healthy and unhealthy foods increased during the pandemic [19]. The COVID-19 pandemic exerted a disproportionate burden on low-income children and families, magnifying their vulnerability to both food insecurity and paediatric obesity [20]. In a review by Pietrobelli et al. [21], in addition to the above-mentioned parameters of lifestyle changes, the diet in a group of 41 obese Italian children and adolescents was also analysed. Data were collected at the start of the lockdown and after 3 weeks of mandatory home isolation. It was shown that the amount of vegetables consumed did not change during the restrictions, while the consumption of red meat, potato chips, and sweet drinks increased. In another nationwide survey among over 10,000 participants in China, people aged 15–28 years voluntarily reported their routine lifestyles (e.g. diet, physical activity) in the months before and after the COVID-19 lockdown. Significant changes were observed in the patterns of the variety of food and beverage consumptions during the COVID-19 lockdown. More participants stopped or reduced their intake of fresh fruit (12.4%), fresh vegetables (7.2%), soybean products (11.0%), and dairy products (11.7%) immediately before and after the implementation of the COVID-19 lockdown [22]. Another Polish cross-sectional online survey of adult Poles, conducted during a nationwide quarantine, aimed to assess whether nutritional and consumer habits were affected under these conditions. Over 43.0% and nearly 52% reported eating and snacking more, respectively, and these tendencies were more frequent in overweight and obese individuals [24]. In turn, Zachurzok et al. [18] did not observe differences in the number of meals per day, nor in the number of snacks, sweets, soda, juices, vegetables, fruit, and fast-food meals consumed before and during the lockdown over the whole studied group.
Summing up the disturbing medical data describing the numerous problems that appeared in the paediatric population during the pandemic, it seems that an intervention in the field of physical and nutritional education, promoting a healthy lifestyle among obese children after the COVID-19 pandemic is currently particularly important and necessary, to mitigate its negative effects on unhealthy weight gain in children. It is important to take broadly defined measures to achieve a return to a healthier lifestyle as soon as possible, including the implementation of the updated recommendations of the World Health Organization (WHO) and the American College of Sports Medicine (ACSM), according to which it is advisable that all children and adolescents have an average of 60 minutes of moderate intensity aerobic activity daily exercise. Although lifestyle intervention (diet and exercise) has remarkable effects on weight management, achieving long-term success in weight loss is extremely challenging, and the prevalence of obesity continues to rise worldwide [24].
Telemedicine in the treatment of obesity
The situation related to the COVID-19 pandemic and the difficulties in accessing traditional healthcare have spread the use of telemedicine services. Telehealth is a service dedicated to patients, in which a healthcare professional uses various digital systems that enable telephone calls, audio-video connections, and monitoring of obtained results by sending results and documentation [25]. The high risk of spreading infection both among staff and patients, limiting the possibility to travel freely and access to traditional medical care, increased the social acceptance of this form of contact with healthcare professionals. In many articles describing the experiences of this new form of therapy, the authors agree that it is necessary to optimize telemedicine in paediatric health care and to establish the standards of such care so that it can be used on a larger scale [26, 27]. In the context of working with an obese patient, the following aspects are important in telemedicine: the whole family can participate in online consultations in real time; digital educational materials can be used during and after the visit; and control teleconsultation allows more frequent and easier contact without exposing patients to costs and wasting time (Fig. 1).
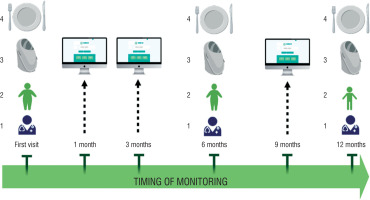
Telehealth, including tele-exercise and tele-nutrition, has been able to address many of the key challenges in delivering health services to obese patients during the epidemic. Promoting increased self-control, nutritional support from a dietitian and psychologist, and sharing training can limit a sedentary lifestyle and be a very effective form of monitoring an obese patient. Many therapeutic teams, somehow forced by the situation, started providing medical advice online during the pandemic, although this method was known earlier [26, 28, 29]. Calcaterra et al. [30] presented an integrated model of caring for obese children by combining telehealth and personal visits. The proposed procedure requires that the first visit of an obese patient should be performed in person and successively after 6 and 12 months of follow-up. The patient’s clinical evaluation, body weight measurements with body composition analysis, and nutritional advice are carried out at personal visits. Televisits are mainly used to assess the progress of treatment, including monitoring body weight, diet, and physical activity – in this protocol, it should take place after 1, 3, and 9 months of observation. In addition, the patient can use the training program provided at any time. It is worth emphasizing that the effectiveness of long-term care for an obese patient depends on the close cooperation of a professional team, which includes a nurse, dietitian, psychologist, and trainer (Fig. 2).
Figure 2
Integrated care model for childhood obesity, combining telehealth and face-to-face visits. Face-to-face visit is proposed at the first evaluation and at 6- and 12-month follow-up; clinical evaluation (1), body weight control (2), body composition evaluation (3), and nutritional counselling (4) are included. At 1-, 3-, and 9-month follow-up. Tele-consultation for monitoring of weight, dietary intake, and physical activity is provided. During follow-up, a supervised exercise training program is remotely delivered 3 times per week in a 30–45-min session [from 30]
On the other hand, O'Hara et al. [26] in their article shared 5 years of experience in using telemedicine in paediatric care at an interdisciplinary paediatric weight management clinic. This schedule is designed to provide the required high intensity and frequency that meets the 2017 US Preventive Services Task Force (USPSTF) recommendation (26 hours of intervention over 12 months). The first visit usually lasts about an hour and is attended by a doctor and a nurse, a dietitian (RD), a psychologist, and a trainer; control visits last an average of 30 minutes. The visits are scheduled quite often: initially 8 appointments a week, then 8 appointments in 2 weeks, up to 6 appointments a month. Both patient families and collaborating paediatricians expressed positive feedback and support for telemedicine, and the services provided via telehealth were of comparable quality to those provided in person. The study assessing the effectiveness of telemedicine [31] confirmed very good results of such treatment. The authors noted the decrease in BMI of obese patients aged 10–17 years who remained in the 1-year Intervention primary care providers (PCPs) and obesity specialists. Using a cross-over protocol, Group 1 had PCP visits + specialist televisits during the first 6 months and PCP visits only during the second 6 months, and Group 2 followed the opposite sequence. Each of the 12 televisits was conducted by a dietitian or psychologist with a patient and parents. The visit program was very intensive: for the first 6 weeks, visits were made weekly. Later, follow-up visits were twice a month. At 3 months, the authors noted a greater decrease in BMI (z-score) for Group 1 (started with PCP visits + specialist televisits) vs. Group 2 (started with PCP visits only) but the decrease in BMI at 6 months and at 12 months did not differ between groups. Patients may have found the program: PCP visits + specialist televisits to be more helpful than visits only with PCP. Most of the patients concluded that they would not have been able to consult obesity specialists if it were not for on-line visits. When asked if in the future they were to choose between a personal visit and a televisit, the majority chose the telemedicine option. Telemedicine can also be used for selective, interventional dietary counselling, because paediatric obesity, and nutrition education for the whole family is the first treatment. In a study by Rhodes et al. [32], parents of overweight and obese children were given a 5-week education in a low-carbohydrate or low-fat diet. Most of the respondents (86%) participated in at least 4 out of 5 planned interviews. Patients had a decrease in dietary fat content, counselling was conducive to changes in healthy eating habits, and parents’ satisfaction with the interviews was assessed as high.
Summarizing, telemedicine today offers many opportunities for good chronic cooperation with an obese patient. It is a valuable addition to traditional visits, and it increases the attractiveness of meetings. This modern approach to treatment is well accepted by young people, and thanks to easy access to group therapy with the participation of the entire therapeutic team or a few patients who motivate each other, it allows a more lasting effect to be achieved. However, it should be emphasized that telemedicine cannot completely replace personal contact between the patient and the doctor and other team members. A well-confirmed method is to combine on-line visits and traditional ones in a planned schedule, which of course should be individually matched to the patient’s needs.
Pharmacotherapy in obesity in children
The preferred therapeutic strategy for treating obesity begins with a non-pharmacological approach, which relies on the adoption of interventions aimed at changing lifestyle, including diet modification, increased physical activity, and behavioural changes. Drugs intended for the treatment of obesity in children are rarely used due to their misconception as drugs with limited efficacy, safety concerns, and reluctance by patients and doctors. Pharmacotherapy should be an addition to behavioural methods, but it is worth using it if the effects of the methods used thus far are unsatisfactory [33]. In Poland, an additional limitation is often the cost of such therapy, because drugs registered for the treatment of obesity and modern drugs used in type 2 diabetes are not reimbursed.
Different types of anti-obesity drugs, which have distinct mechanisms of action, are available; currently, anti-obesity drugs that have been approved for the paediatric population by the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) are of limited number compared to those approved for adults. The following drugs were approved by the FDA for the treatment of obesity for adults: orlistat, phentermine, phentermine hydrochloride/topiramate extended release, bupropion/naltrexone, liraglutide, and semaglutide. As of 2022, only 2 drugs are approved by the FDA for the treatment of obesity in children: orlistat and liraglutide [34]. In the case of semaglutide, clinical trials in the paediatric group are currently underway. It is likely that some of the medications currently used only in obese adults will also be available in older children. Importantly, registration tests are underway for the next 2 unimolecular, long-acting incretin hormones glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) have been reported: NN9709 (formerly MAR709 and RG7697) – phase II study of DT2 [35] and tirzepatide (formerly LY3298176) [36]. GIPR/GLP1R co-agonists are acylated peptides engineered to activate the GIP and GLP-1 receptors, key mediators of insulin secretion that are also expressed in regions of the brain that regulate food intake. In May 2022, the FDA approved tirzepatide (Mounjaro – formerly LY3298176) for the treatment of type 2 diabetes in adults [37].
Orlistat (tetrahydrolipstatin) is a potent, slowly reversible inhibitor of pancreatic and gastric lipases, which are required for the hydrolysis of dietary fat in the gastrointestinal tract. It acts in the lumen of the stomach and small intestine after binding to the active serine site of gastric and pancreatic lipase; the inactivated enzyme does not hydrolyse the fat ingested in the diet in the form of triglycerides to the absorbed free fatty acids and monoglycerides. Its inhibition of fat digestion reduces micelle formation and, consequently, the absorption of long-chain fatty acids, cholesterol, and certain fat-soluble vitamins [38]. Orlistat is approved by the FDA for the treatment of obesity in adolescents (age ≥ 12 years), but it is not approved for children in Poland. In the largest RCT of orlistat, in combination with diet, exercise, and behavioural modification, it significantly improved weight management in obese adolescents compared with placebo. The use of orlistat for one year in this adolescent population did not raise major safety issues, but gastrointestinal adverse events were more common in the orlistat group [39]. In the largest paediatric trial, children were randomized to either orlistat 120 mg or placebo 3 times daily for 52 weeks. At the end of the trial, the BMI had decreased by 0.55 kg/m2 with orlistat and increased by 0.31 kg/m2 with placebo. Furthermore, 26.5% of children in the orlistat group had a 5% or greater decrease in BMI compared with 15.7% of those in the placebo group [40].
Liraglutide is an acylated glucagon-like peptide-1 analogue (GLP-1), which controls appetite and food consumption, strengthens the most important signals of satiety, and reduces the most important signals of hunger, leading to a reduction in body weight and fat tissue. It prevents the development and reduces inflammation of the atherosclerotic plaque, has a beneficial effect on the level of plasma lipids, and improves glycaemic control in patients with type 2 diabetes by reducing fasting and postprandial blood glucose [41].
Liraglutide is an anti-obesity medication that is approved by most regulatory agencies (including the United States Food and Drug Administration and the European Medicines Agency) for chronic obesity [42]. In the largest RCT of liraglutide 3 mg among adolescents (12 to < 18 years old) with obesity, in which all participants also received lifestyle therapy, the mean placebo-subtracted BMI reduction was approximately 5% with one year of treatment. After 56 weeks, a reduction in BMI of at least 5% was observed in 43.3% of participants in the liraglutide group vs. 18.7% in the placebo group, and a reduction in BMI of at least 10% was observed in 26.1% and 8.1%, respectively [43]. Importantly, no new safety signals were observed in the adolescent trial in relation to previous adult trials.
It is well known that the consequence of chronic obesity may be type 2 diabetes mellitus. Although cases of T2DM in the paediatric population, especially in Europe, are still not very common, it should be expected that in the context of the rapid increase of obesity after the COVID-19 pandemic, there may be more and more children with T2DM. Standard T2DM treatment includes lifestyle changes (dietary modifications and increased activity) and pharmacotherapy [44]. Current pharmacologic treatment options for youth-onset T2DM are limited to 3 approved drugs: insulin, metformin, and liraglutide [45]. Due to its good tolerability and high efficacy, metformin is currently the first-line drug in the treatment of T2DM, and due to its safety and the lowest number of side effects, it is the most commonly used drug in children. It is approved for the treatment of T2DM in patients over 10 years of age [46]. It affects glycaemia by reducing hepatic glucose production, increasing intestinal glucose utilization, and improving insulin-mediated glucose utilization in peripheral tissues. Metformin can be taken with meals or in a sustained release dose, usually 500–2000 mg/day, and may cause slight weight loss (up to 4 kg) [47]. Moreover, metformin can be used as adjunctive therapy for patients at high risk of metabolic complications, fatty liver, obesity, and, above all, insulin resistance. A randomized clinical trial in youths aged 10–17 years with T2DM demonstrated the addition of subcutaneous liraglutide (up to 1.8 mg daily) to metformin (with or without basal insulin) as safe and effective to decrease A1C (estimated decrease of 1.06 percentage points at 26 weeks and 1.30 at 52 weeks), although it did increase the frequency of gastrointestinal side effects [45]. It is worth emphasizing that metformin has been used for many years for managing paediatric patients without diabetes who are overweight or obese, especially with a confirmed insulin-resistant state. Although its use for weight management is off-label, metformin is typically prescribed in youths for an on-label concurrent conditions [48, 49]. It seems that the consumption of weight-loss drugs in children has increased during the last years and during the COVID-19 pandemic in parallel to an increase in the number of obese patients, especially new widely available drugs like liraglutide; however, there are currently not enough reliable data on this matter.
Conclusions
Due to the scale of the problem of overweight and obesity, much attention is currently being paid to the search for effective forms of therapy. There is no universal or effective method of treatment of obesity. Healthy lifestyle recommendations are sometimes insufficient and do not work. Pharmacotherapy is still used relatively rarely, but it is a great opportunity for patients in whom an intensive dietary approach did not bring the expected results. Research is still needed to personalize childhood and adolescent obesity treatments and translate them into clinical practice. It is definitely worth using different modern methods of treatment, among others telehealth and telemedicine, which are not only positively assessed by the medical staff, parents, and patients, but also have a documented positive impact on the achieved clinical results. The use of such methods should no longer be seen as a luxury but more as a potential to be used as a promising tool to more conveniently and effectively reach areas requiring clinical care for childhood obesity, implemented long-term and holistically by the entire medical team.

 ENGLISH
ENGLISH