PURPOSE
Collet-Sicard syndrome (CSS) was first described in 1915 by French otolaryngologist Fréderic Justin Collet, who referred to it as “glossolaryngoscapulopharyngeal hemiplegia” [1]. In 1917, French radiologist and neurologist Jean-Athanase Sicard independently delineated a neurological disorder with a similar clinical presentation [2]. CSS is a rare neurological syndrome characterized by ipsilateral palsy of the cranial nerves (CN) IX, X, XI, and XII, without involvement of the sympathetic trunk. The syndrome presents with a distinctive constellation of symptoms, including dysphagia, absence of the gag reflex, impaired taste and sensation in the posterior third of the tongue, dysphonia, tongue deviation, palatal paralysis, hemianesthesia of the larynx, pharynx and soft palate, as well as weakness of the quadriceps and sternocleidomastoid muscles [3, 4].
This condition is most prevalent among men. The most common clinical manifestations include dyspha gia, dysphonia, tongue deviation, palate paralysis, and trapezius muscle weakness, and the most frequently identified etiology is neoplastic. Other potential causes of CSS include vascular, traumatic, congenital, and systemic conditions. Current evidence indicates that the lesions commonly affect the jugular foramen and the parapharyngeal retrostyloid space – the former is most often associated with neoplastic lesions and the latter with vascular pathology. Furthermore, the prevertebral anatomic space is most often affected by traumatic injury. Treatment depends on etiology and includes conservative management, surgery, radiotherapy or radiochemotherapy, and endovascular treatment [3-5].
The purpose of presenting this clinical case is to raise clinical awareness of CSS thereby reducing diagnostic delays and facilitating earlier initiation of treatment to improve patient outcomes.
CASE PRESENTATION
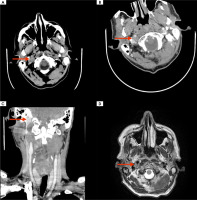
A 58-year-old male presented to the Emergency Department with approximately four-month history of progressive dysphagia and speech disturbances. The patient demonstrated unintentional weight loss of approximately 8 kg over this period. He had been previously assessed at the neurology, gastroenterology, and pulmonology outpatient clinics due to these symptoms. The patient’s medical history included a previous treatment for C4-C5 spondylodiscitis, approximately two years prior, a history of cardiac arrhythmias and gastroesophageal reflux. Among abnormalities observed during the neurological examination were dysphonia, diminished reflexes on the right side of the pharynx and the palate, deviation of the uvula to the left side, atrophy of the right half of the tongue with associated tremor, and deviation of the tongue to the right side. Furthermore, residual right upper limb weakness and head drooping were observed following treatment for spondylodiscitis. According to the patient, these symptoms have worsened over the past few months. The results of the laboratory tests were within the normal range. The patient was admitted to the Neurology Department for further evaluation. An extensive differential diagnosis was conducted, during which vascular etiology and amyotrophic lateral sclerosis were both ruled out. The laryngological examination revealed symptoms of damage to the right vocal fold. A computed tomography (CT) and magnetic resonance imaging (MRI) of the brain and neck revealed the presence of an extensive focal lesion in the region of the right jugular foramen, located between the internal carotid artery and the jugular vein, measuring 16 × 15 × 25 mm, and exhibiting heterogeneous enhancement following the administration of contrast agent (Figure I). Additionally, bilateral presence of multiple reactive cervical lymph nodes was observed. The possibility of lymphoma was raised during the hematological consultation, regardless of normal blood count and white blood cell smear results. Obtaining a sample of the lesion for histopathological and immunohistochemical examination was recommended. Neurosurgical evaluation was without sequelae. To collect the material, the patient was transferred to the Otorhinolaryngology Department. The pathomorphological findings were consistent with a diffuse large B-cell lymphoma (DLBCL). The patient was sub sequently referred for further hematological treatment.
Figure I
A) Computed tomography (CT) scan of the brain (without contrast enhancement) showing a focal lesion in the area of the right jugular foramen between the internal carotid artery and the jugular vein (red arrow). B, C) CT scans of the neck (with contrast enhancement) showing a focal lesion with heterogeneous contrast enhancement (red arrow). D) T2-weighted sequence magnetic resonance scan showing a focal lesion in the area of the right jugular foramen between the internal carotid artery and the jugular vein (red arrow)
COMMENT
The clinical presentation and the results of additional tests led to the diagnosis of CSS. The patient had evidence of damage to the lower CN IX, X, XI, and XII, with symptoms consistent with this rare syndrome. A carefully examined patient’s history, including details about his constitutional symptoms suggestive of malignancy, guided the diagnosis. Histopathological examinations substantiated the neoplastic etiology of the lesion and led to the diagnosis of DLBCL. The analysis of the available literature indicates that this is the first documented case of CSS resulting from DLBCL.
The most prevalent cause of CSS is a tumor, most often in the form of metastases to the skull base, and paragangliomas [5]. In the diagnosis of lower CN palsy, it is also prudent to consider other potential etiologies that may manifest as CSS. These include, but are not limited to, the internal carotid artery dissection [6-8], aneurysm [9, 10] or pseudoaneurysm [11, 12], internal jugular vein thrombosis [13], Jefferson fracture [14-16], condyle fracture [17], congenital bone conflicts [18, 19], and infectious diseases [20, 21]. CSS can be effectively identified during routine clinical examinations. The pre sence of CN IX palsy can be determined by requesting the patient to swallow saliva, while CN X palsy can be diagnosed through the observation of dysphonia, dysphagia or vocal cord paralysis. CN XI palsy can be identified by examining for sternocleidomastoid and/or trapezius muscle dysfunction, whereas CN XII palsy can be diagnosed by noting the presence of ipsilateral tongue wasting [4, 5].
CONCLUSIONS
A constellation of symptoms such as dysphagia, hoarseness or dysphonia, and tongue weakness should guide clinicians to the possibility of CSS. Given the most common neoplastic etiology of CSS, an accurate recognition of the characteristic symptoms, combined with a thorough neurological examination and accurate interpretation of the patient’s history, is essential for prompt diagnosis and initiation of appropriate treatment.







