PURPOSE
The article presents the fundamental phases of the therapy administered to a 54-year-old patient after a subarachnoid haemorrhage from a ruptured aneurysm of the anterior communicating cerebral artery with an intracerebral haemorrhage, after aneurysm embolisation and left craniotomy, and after an ischemic cerebral stroke. The therapy was based on applied behaviour analysis.
After less than two months of treatment in hospital conditions, the patient was forced to confront a reality unknown to him. Socially and professionally active before, after returning home, the man remained a person with certified severe disability, incapable of independent existence and employment. He showed difficulties with behaviour control and with initiating, planning, and organising his activities. The functional state of his organism was dependent on external control. He required long-term assistance and care as well as intensive therapeutic and medical work in all areas of human existence.
The author of this article is a person who, at that time, was in training to obtain a Polish Behavioural Therapist License (PLTB). She worked with people suffering from developmental disorders on a daily basis and, as a person studying and practicing applied behaviour analysis, she was fully aware of the possibilities of that technique and of the effectiveness of the models of the therapy, based on general rules of learning with regard to changing the behaviour patterns of all living organisms. She undertook to design her own multi-profile rehabilitation programme based on applied behaviour analysis.
As a result, 67 days after the surgery, activities of daily living training, based on applied behaviour analysis, were implemented in the patient’s home environment. Training was conducted 7 days a week, 24 hours a day, by a team composed of a behavioural therapist, a nurse, and the patient’s family. The man, who was in a vegetative state at the beginning of therapy, underwent multi-profile rehabilitation in a natural home situation, based on applied behaviour analysis. The therapy described in this article was administered from 27 November 2020 to 31 December 2021. During that time, behaviour modification was carried out in all areas of the man’s functioning. Desirable sets of behaviour were developed, i.e., cooperation, imitation, communication, self-service skills, order skills, social skills, daily life organisation skills, and spare time organisation skills. Undesirable behaviour patterns were reduced. Simultaneously, the patient was subjected to motor rehabilitation, the outcome of which was an improvement in his motor ability.
Currently, the man is generalising his skills across settings and over time. The assessment concerns the period from 1 January 2022 to 31 December 2022. Thanks to the therapy, the patient did not remain excluded from the socio-cultural sphere. He uses public utility facilities, organises his space as far as possible, and expands his social communication repertoire. Using information technology tools, he fulfils many roles in social and family life.
The process of the patient’s gradual transition from the vegetative state to nearly full-quality functioning in the family and in society is clearly a result of the author’s ABA programme that was implemented. The programme was divided into 4 phases of behavioural therapy, which are described in this article with patient functional assessment provided for each phase.
The main aim of the behavioural therapy was to improve the man’s overall condition, particularly to improve his living skills and to reduce problematic behaviour episodes. The application of effective and efficient behavioural strategies in a stroke patient fully reflects the adjustment of therapeutic techniques to the needs of individual cases regardless of age or disease entity. According to the literature, a person with a brain damage can be subjected to effective therapeutic interventions [1].
The therapy is used in the context of experience with the patient’s problems to which a solution is provided by applied behaviour analysis. The post-stroke patient’s problems are a point of departure for developing a broader project. Work with the patient based on applied behaviour analysis creates psychosocial scaffolding and eliminates functional difficulties. Because the patient remained in a situation of limited health service options, the focus of the therapy on evidence-based teaching made it an integral part of the patient’s success.
While creating the therapy programme and writing this article, the author referred to me her experience and available literature on the subject.
CASE DESCRIPTION
A 54-year-old man, single, living alone, being socially and professionally active. Two days elapsed from the first symptoms of stroke to the moment of hospitalisation, which significantly contributed to the deterioration of his health condition. The patient experienced fainting combined with disorders of consciousness. On admission to hospital, he was conscious and drowsy, with a GCS score of 13. A CT scan of the head revealed a subarachnoid haemorrhage from an ACoA aneurysm and an intracerebral hematoma of the left frontal lobe.
(CT scan: A saccular aneurysm 8.5 x 5.2 mm in the region of the AcomA/RACA-seg. I/II, with the base facing upwards and forwards. A suspected aneurysm < 2 mm near the branching-off of the AcomP left of the ICA. A suspected aneurysm approx. 2 mm to the right, between RMCA I and II. L frontal lobe hematoma penetrating into R frontal lobe and the ventricular system – 7 cm in size, midline shift 6 mm to the R. Ruptured aneurysm in the region of the RACA/AcomA).
As a matter of urgency, under general anaesthesia, AcoA aneurysm embolisation was performed using 6 spirals. Decreased RA2 inflow was observed during the procedure. Frontal craniotomy with intracerebral hematoma removal was performed subsequently. A GCS score 11-12 after the procedure, with no motor deficits, with a Babinski reflex on the left and nuchal rigidity. On the third day after surgery, the patient’s condition deteriorated. There were disorders of consciousness and tetraparesis. The patient’s general condition was unstable and poor. According to information received from the doctor, the patient was pronounced brain dead on the Glasgow Coma Scale. Another CT scan revealed that during the surgery, the patient had one more ischemic cerebral stroke.
(CT scan of the head: Hypodense areas, most probably ischemic, in the vascularisation regions of anterior cerebral arteries with hematomas of different sizes within these areas; larger hematomas in the left frontal region – the largest one 50 x 38 mm in size, partly coating the region of the embolised aneurysm. Low blood levels in the posterior horns of the lateral ventricles and in ventricle III. A small amount of blood in the cerebral sulci of the frontoparietal region and in the anterior part of the interhemispheric fissure; small hematomas in the region of the lateral fissure on the left side. Cerebral sulci in the frontal regions are invisible. Frontal horns of the lateral ventricles with signs of modelling. Central brain structures convex to the right by approx. 4 mm. Subdural air at the craniotomy level).
After the surgery, the man was hospitalised in the neurosurgical department for 35 days. The patient remained conscious but sluggish. Contact with him was difficult. His condition qualified him for palliative or hospice care. Although he was in a good general condition, he was nevertheless transported to the neurological ward for further treatment. In the neurological ward, he received pharmacological treatment (Nootropil, Clexane, Betaloc ZOK, Biseptol, Tritace, Amlopin, Ketonal, Ketrel, Lorafen, and Haloperidol). The patient did not cooperate with the staff. He did not carry out instructions, such as, “move your finger”, “open your mouth”, or, “close your eyes,” or carried them out with delay. Rehabilitation was not conducted due to difficult contact with the patient, urinary tract infection, and patient isolation. Further treatment in hospital was no longer possible, and neither was the transfer to the rehabilitation ward. The man was therefore discharged, having been hospitalised for a total of 58 days in the neurosurgical and neurological wards.
(CT scan of the head: condition after a left frontal craniotomy and AcoA aneurysm embolisation – numerous artefacts. Extensive heterogeneous hypodense areas in the frontal lobes and in the deep structures on the left side – liquifying ischemic and haemorrhagic lesions with the formation of malacic areas. Vasogenic hypodense centres in both hemispheres. Accentuation of subdural fluid spaces).
In accordance with the decision of his family, the man was transported home. He stayed with his family, who decided to provide him with comprehensive assistance, care, and decent living conditions. The family members’ idea of decent living conditions was not limited to home care and nursing. They were looking for new solutions. The author’s multi-profile rehabilitation programme was implemented; it was based on applied behaviour analysis and divided into 4 phases. In the described programme phases, we dealt with the same person at different stages of functioning. The phases of the programme were administered on the basis of the patient functional assessment, performed using direct, indirect, and experimental methods [2].
Phase I. The patient functional assessment, behavioural therapy objectives, and intervention strategies
The aims of the individual behavioural therapeutic/rehabilitation programme stemmed from the functional state of the organism. The assumptions of work with the patient were specified, i.e., cooperation, imitation, and undesirable behaviour reduction. The primary aim for the patient’s family was to make him admissible to the rehabilitation ward in hospital conditions.
Due to the significant impact of reinforcements in working with adults with acquired brain damage [3], the programme began with the identification of reinforcers. The patient’s menu included various kinds of reinforcements. The most effective reinforcements in his profile were biological ones, i.e., candies, chocolate, and cookies. There were also reinforcements associated with activities, such as watching TV, material reinforcements, and social reinforcements, including systematic attention and approval [4]. Attention and signals or approval were provided at the moment of the man’s desirable behaviour in every situation of daily life.
Accompanying reinforcers should be related to the patient’s programming and programme goals [5]; therefore, further reinforcements were conditioned, especially those related to activities. With time, the full bag of consumption-related reinforcements was supplemented with interactions/cooperation with household members and the physiotherapist.
Biological reinforcements were provided for the patient’s every correct reaction, even the smallest one, to instructions, such as, “look at...”, or, “raise your hand”, when changing his body position from his back to his side, when changing the disposable diaper, getting dressed, putting away a cup of water, and maintaining eye contact with the therapist.
Numerous behavioural contracts were made with the patient [6] – not only for simple activities but also for ones that required greater effort and time from the non-ambulatory patient, for example: doing exercises with the physiotherapist for an hour, DRO [6], lying peacefully for 30 minutes, or helping with nursing activities, such as the patient is holding a diaper – “give it to me”. The patient usually worked for biological reinforcements. Behavioural contracts were initially visualised; then, they were written by the therapist, and finally they were written down by the patient. DRO procedures were effective for children with varying degrees of intellectual disability. DRO has been shown to be successful both with and without rules laid out for the individual [7].
Numerous proactive strategies were used. Because of the left hemispatial neglect syndrome, the patient’s bed was arranged in such a way that all activities and interactions took place to the left to ensure the greatest possible activation of the patient’s left side. Work with a calendar was applied to achieve better orientation in time and space. Intensive activities of daily living training were implemented in the patient’s bed based on behaviour chains, e.g., arranging the blanket, putting away the cup, using the phone, using the TV remote, and washing face. Improving the cognitive abilities of stroke patients by enhancing functional training is important to ensure effective early rehabilitation training. Early training may not only improve cognitive dysfunction in stroke patients but also aid in returning to daily activities [8].
Systematic desensitisation was applied [2] regarding the acceptance of the catheter. As a result of being exposed to the catheter stimulus, fear in the patient considerably reduced. According to the literature on the subject, systematic desensitisation is effective in the treatment of phobias and some other anxiety disorders [9].
The man exhibited difficult behaviour patterns, such as tearing out the catheter. He also exhibited ideas of going to the bathroom or to work which was set in the reality of 15 years before, when the patient was a physically healthy person. During such moments, he was highly excited and active in his bed. Despite tetraparesis, he sometimes fell off the bed (which he thought about as, “going to the bathroom”). Two faces of the post-stroke patient manifested themselves: (1) without planning, excessively inhibited in everyday activities; and (2) living in his space from 15 years before, excited, exhibiting difficult behaviour episodes. After a difficult behaviour, the patient lapsed into unawareness about the occurrence of difficult behaviour episodes. These kinds of behaviour lasted from a few to 50 minutes.
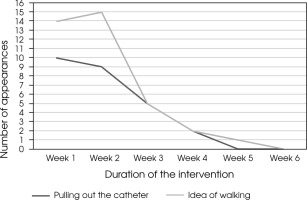
In the behavioural programme, due to the behaviour threatening to the patient’s health and life by damaging his bladder, the therapist used mechanical immobilisation procedures [2], in accordance with Section X c of the Code of Ethics of the Polish Behavioural Therapist License. For medical reasons, such as delicate skin, the patient’s arms were protected with a blanket (made of delicate fabric so as not to injure the skin). The number of difficult behaviour episodes occurring in the patient is presented in Figure I.
Phase I of the therapy lasted 6 weeks. The condition for the patient’s hospitalisation in the rehabilitation ward was his cooperation with the medical staff. The patient was admitted to the rehabilitation ward. He fully generalised the skills acquired through intensive training at home in hospital conditions. The patient achieved an improvement in trunk stabilisation. His stay in the rehabilitation ward lasted 20 days. Next, he spent 8 days in the observation and isolation ward due to COVID-19 infection.
Phase II. The patient functional assessment, programme modification, and intervention strategies
The objectives of the individual therapeutic/rehabilitation programme were modified based on the progress in the patient’s functioning. The assumptions of work with the patient were specified; they included key skills, i.e., cooperation, imitation, self-service skills, and undesirable behaviour reduction.
Phase II of behavioural therapy was a period of work with a non-ambulatory patient. The man was able to verticalise his trunk in a wheelchair. The proactive behavioural strategies from Phase I were continued. To enable the man to do tasks and activities without direct clues or hints, the therapist used a daily schedule [10]. Implemented plans have been shown to be effective in increasing the independent behaviour of people with disabilities [11].
Initially, the patient’s schedule included a few activities, such as drinking water on his own at time intervals, taking medication after meals, and organising his spare time. Then the tasks in the schedule were expanded based on the patient’s established skills. Due to the patient’s deficits stemming from brain damage and due to his motor disability, the daily schedule was introduced on a smartphone. Clues were provided using a smartwatch worn on the wrist, where sound and vibration redirected the patient to the schedule without hints from third parties.
Systematic desensitisation was applied regarding the acceptance of the daily urine collection bag. As a result of being exposed to the urine collection bag stimulus, fear in the patient considerably reduced.
Difficult behaviour patterns were noted, such as spilling urine from the daily urine collection bag on himself and the surrounding objects. The number of difficult behaviour patterns occurring is presented in Figure II.
Episodes of tearing out the catheter and strong excitement did not occur. In the behavioural programme, in accordance with Section X c of the Code of Ethics of the Polish Behavioural Therapist License, time-out without exclusion was applied. Time-out was associated with an armband. The armband around the patient’s arm meant that he had access to reinforcements; no armband meant that the access was suspended.
Phase II lasted 20 days. The patient was admitted for hospitalisation in the rehabilitation ward, where he stayed for 85 days. The patient fully generalised the skills previously acquired through the multi-profile training.
Phase III. The patient functional assessment, programme modification, and intervention strategies
The objectives and programme of the individual therapeutic process were modified based on the progress achieved in motor rehabilitation and in the generalisation of the skills acquired during the previous phases of treatment across different situations and settings. Assumptions concerning autonomous and independent functioning were added, including self-service skills and order skills. Cleanliness training was added. The assumptions of work with the patient were specified. They included cleanliness training, economic skills, and the development of self-service skills.
Phase III of behavioural therapy was a period of work with the 55-year-old patient diagnosed with epilepsy with generalised tonic-clonic seizures as a result of a stroke. He needed help with getting up and transferring to the wheelchair. The rehabilitative treatment led to improvement regarding the range of active movements and muscle strength of the lower limbs. The patient was able to cover several distances with support. He walked slowly, in small steps. Sphincter control disturbances. Diapered and non-catheterised due to numerous urinary tract infections. Disordered communication repertoire of mands. Cognitive function deficits, with a predominance of attention and executive function deficits. Difficulties with initiating, planning, and organising activities. Disturbed social skills. Disturbed temperature regulation. The man exhibited no difficult behaviour patterns.
As regards behavioural strategies, proactive strategies used in the earlier phases of the programme were continued. The daily schedule was maintained, and activities organising spare time were added, such as listening to audiobooks, reading books or activities associated with self-service, and order skills.
Self-service skills regarding the patient’s hygiene activities were transferred from the bed to the bathroom. The skills acquired were generalised across settings. Further skills were implemented, such as putting clothing on upper trunk. Order skills included putting things back in their place, using small household appliances, preparing meals, and cleaning up after meals. The patient was taught through total-task chaining [6].
The ability to use the toilet on one’s own is one of the most important skills acquired in life. As a result of incontinence-related underwear staining, more time, energy, and financial resources have to be devoted to one person’s basic needs. Behaviour showing incapability of using the toilet can also pose a threat to the person’s health [12]. The 55-year-old patient remained dependent in matters of independent toilet use, including sphincter control.
Based on the patient’s needs regarding independent functioning in this area, cleanliness training was introduced. At first, the control of physiological functions was based on training the body and activating a sequence of actions rather than on developing conscious physical sensations that signal the need to defecate. The habits training makes it possible to provide an acceptable way of retaining dignity and improve personal hygiene; it leads to the development of a routine of regular defecation [12]. Behavioural toilet training combined with feedback to enable error-free learning is more effective than trial-and-error learning for a stroke patient [13].
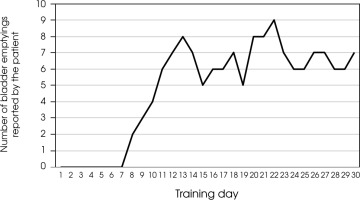
Two-day observation of the man was conducted. A record was kept to document drinking and eating times, bladder emptying times, and stool control. The man received 2 cups of water to drink, and the therapist kept a record of times when the patient emptied his bladder. Urination started 2 hours after drinking. Based on the results, the patient’s individual profile was created. A schedule of regular toilet visits was made. Habits training was introduced, covering the day between 5:00-6:00 and 22:00-23:00, depending on the patient’s diurnal and nocturnal activity. The patient exhibited sleep disorders. Training was based on the principle of 2 cups of liquid and a toilet visit 2 hours later. He remained there for an average of 5-10 minutes. A record was kept of whether the patient managed to urinate. Incidents of enuresis or faecal staining outside the designated hours were ignored as much as possible. Biological reinforcement was provided in training. After a toilet visit, the patient drank another 2 cups of water – this pattern appeared every day, including liquid dishes, which the patient received every day. Establishing and maintaining routine, with a complete sequence of actions performed each time, became a guarantee of the man’s success.
The 8th day of training brought the first spontaneous messages on toilet use involving bladder emptying. Toilet use additionally performed a mandic function at that time as the patient required physical support when getting up and transferring to a wheelchair. On the 12th day of training, 24-hour patient communication was observed concerning the need to empty the bladder. Subsequent days brought further skills regarding bladder control and signalling the need to use the toilet; the man experienced an increased sense of full bladder and calmly covered the route to the toilet. The patient was in cleanliness training for 30 days. He used the toilet when he needed to. He begun to differentiate between the urge to defecate and the urge to empty his bladder. After training, he was fully independent regarding toilet use. Episodes of nocturnal enuresis did not occur. The man underwent motor rehabilitation at home. Data regarding cleanliness training are presented in Figure III.
Phase IV. Generalisation of skills, programme modification, and intervention strategies
The objectives and programme of the individual therapeutic process were modified based on the progress in motor rehabilitation and the generalisation of the skills acquired during the previous phases of treatment across situations and settings. Social skills training was added. The assumptions of work with the patient were specified, i.e., social skills training, economic skills, and the development of self-service skills.
Phase IV of behavioural therapy was a time of work with the 55-year-old patient who showed an improvement in the overall condition. The abilities acquired during the activities of daily living training in the previous phases of the programme were maintained. The ongoing rehabilitation improved the range of movements in hip and knee joints. The patient walked with elbow crutches. He continued to show disturbed social interactions and disturbed functional communication involving mands and waiting.
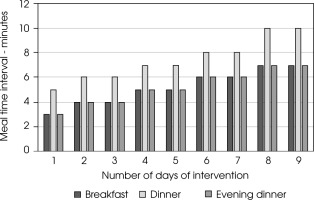
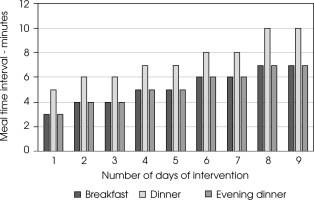
For compulsive eating, a behavioural contract on eating meals calmly was made for a specified time interval. The patient ate meals at a fast pace: breakfast – 3 minutes, lunch – 5 minutes, and dinner – 3 minutes. The man usually didn’t bite his meals. The patient had to eat a meal no earlier than a specified criterion – the interval of eating each meal was increased by 1 minute. The patient always chose reinforcements as part of the concluded contract. After the specified time, the contract was settled. Most often, these were biological reinforcements, such as sweet snacks. As the days passed, the time interval for eating meals became longer. The contracts were written by the patient. Figure IV shows the scope of behavioural changes during the intervention.
Table 1
Phase I of the therapy
Table 2
Phase II of the therapy
Table 3
Phase III of the therapy
Table 4
Phase IV of the therapy
The skills acquired were generalised to settings such as restaurant or cinema. Further skills were introduced, such as receiving guests or functioning independently (e.g., for 8 hours) at home.
Order skills were expanded, such as vacuuming or using a dishwasher. The patient was taught through total- task chaining.
Based on modelling [2], the patient was taught the social skills of waiting and building longer utterances. Methods based on stimulus control were used; the therapist applied additional clues aimed at stimulus control, such as the, “wait”, card. The patient takes part in family celebrations and uses various public utility facilities, such as a restaurant or a church.
COMMENT
The article presents an example therapy based on applied behaviour analysis administered to a patient after a subarachnoid haemorrhage from a ruptured aneurysm of the anterior communicating artery with an intracerebral haemorrhage, after aneurysm embolisation and left craniotomy, and after an ischemic cerebral stroke. The author has described a model of therapeutic procedures using a wide array of techniques proposed by applied behaviour analysis. The therapy was administered in accordance with the principles of applied behaviour analysis, with the programme adjusted to the functional state of the body, the needs of the patient and his family, and community factors. The community factors included the possibilities of providing health care and the sources of financing available to the patient and his family as regards the application of new technologies in working with the man. The therapeutic programme was adjusted to the patient’s individual needs. Teaching took place on a multi-profile basis. The man’s progress in the acquisition of skills was the basis for the modifications introduced in the programme of therapeutic work and in the family’s increasing demands regarding health care services.
The focus of the patient’s therapy on evidence-based teaching changes the approach to the patient as a socially excluded person. The behavioural therapy is focused on teaching new skills and reducing undesirable behaviours, which ultimately improves the functioning of the person after stroke and their family.
It creates a kind of relief buffer for the patient’s family members, who are obliged to provide palliative care 24 hours a day, which involves financial and, above all, emotional losses. The patient himself is not a person doomed to life in bed without the fulfilment of his needs. A patient dependent on external control, isolated from social roles, and experiencing radical sensory, perceptual, and cognitive weakening becomes a person who can be restored to the full joy of life and to the functional use of life thanks to applied behaviour analysis.
Data collected from the patient’s family indicate that the patient’s condition dramatically improved his self- efficacy. According to the patient, the implemented behavioural interventions contributed to his independent functioning in society, restored optimal physical fitness, and, above all, restored the meaning of life and hope for a better tomorrow.
The presented phases of therapy fully reflect the effective modification of behaviour patterns in a person after a subarachnoid haemorrhage from a ruptured aneurysm in the anterior communicating artery with an intracerebral haemorrhage, after aneurysm embolisation and left craniotomy, and after an ischemic cerebral stroke.
The outcome of the applied behaviour approach seems to be significant enough to encourage the further development of the therapy for stroke patients regardless of the type of neurological disorders, functional difficulties, and age.