INTRODUCTION
Obesity has become an epidemic in the world, with rates tripling between 1975 and 2016 [1]. Accordingly, in 1997 the World Health Organization recognized obesity as a pandemic that is a major cause of health problems [2]. The World Health Organization’s 2016 report shows that 1.9 billion people over the age of 18 worldwide are overweight and the more than 650 million are obese; this means that 39% of people over the age of 18 are over-weight and 13% are obese [3]. The Institute of Global Burden of Disease report also shows that the body mass index (BMI) of 25 kg/m2 and above in adults between 1980 and 2013 in men increased from 28.8% to 36.9%, while the increase in women was from 29.8% to 38% [4]. There is also a significant increase in overweight and obesity among children and adolescents in both developed and developing countries [4]. In this regard, the increase in BMI in the form of overweight and obesity is associated with a range of diseases that are threats to health, such as mortality [5-7], cancer [8-11], diabetes [12-14], reduced quality of life [15-17], depression [18, 19], work-related issues [20-22], and other mental health issues [23, 24]. One of the health dimensions that can be affected by over-weight and obesity is sleep disturbances [25].
The International Classification of Sleep Disorders includes a variety of conditions [26]. The most prevalent type of sleep disorder is insomnia, with an estimated 30% of the adult population having trouble starting and continuing sleep, and between 5-10% having insomnia syndrome [27-29]. Another type of sleep disorder is obstructive sleep apnea, with a prevalence of 9% to 38% in the general population and is more prevalent in men [30]. It is estimated that among adults aged 30-69, 936 million worldwide have mild symptoms of obstructive sleep apnea and 425 million have moderate-to-severe obstructive sleep apnea [31]. Other types of sleep disorder can be noted as excessive daytime sleepiness; the overall prevalence of this disorder is reported to be 10.4% in men and 13.6% in women [32]. There are other types of sleep disturbance, such as poor sleep quality, sleep complaints, and so on. Several factors have been reported in connection with sleep disturbances, including aging [30, 33], sex, depressed mood [34], smoking [35], and alcohol use [36].
In addition, sleep disturbances have negative effects on various aspects of health and work such as increasing the risk of sick leave [37], dementia [38], cardiovascular disease [39], back pain [40], physical impairment [41], and mental disoders [42-44].
Studies have examined the risk factors associated with sleep disturbances [45-49]. The relationship between these and BMI and has been investigated in recent studies [30, 49, 50]. Accordingly, systematic review and meta-analysis studies have shown that BMI and weight loss are associated with a range of sleep disturbances, including the dia gnosis and symptoms of insomnia [51], obstructive sleep apnoea [30, 52], and restless legs syndrome [53]. It is clear that overweight and obesity have widespread negative effects on various dimensions of health, and one of these dimensions is sleep. Three systematic reviews and meta-analyses have examined the relationship between BMI and sleep disturbances [30, 51-53]; however, reviewing this group of studies reveals several critical points and necessitates the need for a new systematic review and meta-analysis. First, out of the total number of these studies, only three [49, 51, 53] have meta-analyzed the relationship between BMI and sleep disturbances. Second, each of these three studies addressed only one type of sleep disturbance and did not provide a comprehensive meta-analysis of the association between BMI and sleep disturbances. Third, these studies of the results of research often relied on cross-sectional studies, although cross-sectional studies are not able to determine the causality between BMI and sleep disturbances. Although some studies have examined sex differences in the relationship between BMI and sleep disturbances, this has not been the case for a variety of other causes of sleep disturbances.
Based on what has been stated, this study sought to examine the risk of sleep disturbances in overweight and obesity based on longitudinal studies. This association was also examined separately for overweight and obesity. The third goal was to examine sex differences in the association between BMI and sleep disturbances. Finally, associations between BMI and three types of sleep disorders including insomnia, obstructive sleep apnea, and excessive daytime sleepiness were investigated.
METHODS
Search strategy
In this project, to guide the systematic review and meta-analysis process the steps mentioned in the PRISMA [54] protocol were used. Three sources of scientific information, namely PubMed, Scopus, and Embase, were selected as scientific databases, and based on a complete syntax of keywords listed in Appendix 1 each of these sources of information was fully searched; articles published in English until May 2021 were included. A manual search on references in related articles was also done. In cases where the articles were ambiguous, the authors were contacted via email to provide the required information.
Selection criteria
A set of inclusion and exclusion criteria were used for this study. Studies were included in the project if they met the following requirements: 1) overweight and obesity were considered as exposure variables; 2) sleep disturbances such as insomnia, restless legs syndrome, obstructive sleep apnea, snoring, sleep complaints, poor sleep quality, and excessive daytime sleepiness were the outcome variables; 3) study design was longitudinal studies, and cross-sectional, retrospective, time series, clinical trial studies, and case studies – review studies were excluded. Studies were excluded from the project with one of the following conditions: 1) studies in which the study subjects were children; 2) studies that did not provide the necessary information for the odds ratio and making this calculation was not possible; 3) studies on women during pregnancy or following childbirth; 4) studies that were from the same database and in this case only one article with the highest quality was selected.
Data extraction
A framework for the information extraction process was created. Accordingly, types of information were extracted for each of the eligible studies and these included information sets including the authors of each study and year of publication, population, country, length of time until fellow-up, demographic indicators of the study population such as age and sex, BMI, sleep disturbance and its measurement, and finally the result of each study.
Qualitative measure
In the qualitative evaluation section, as an essential component of a systematic review, the EPHPP tool [55, 56] was used. In the present study, according to the nature of this research, five adjusted dimensions of this tool were used to assess the quality of each of the studies selected.
Meta-analysis
This research involved a systematic review as well as a statistical analysis in the form of meta-analysis; the steps taken to complete the meta-analysis are described below. The odds ratio and confidence interval were extracted for each study. In cases where the risk ratio was reported, this ratio was converted into the odds ratio [57]. In cases where the hazard ratio was reported, this ratio was pooled separately. In some studies, there were dependent outcomes that used existing procedures [58] to combine them, and in independent outcomes, a fixed-effects method was used to combine them. Therefore, this information was extracted from each study and then the pooled odds ratio was calculated on the basis of the random- effects method. The analyzes were conducted at several levels. The first analysis was the association between BMI ≥ 25 and sleep disturbances, and then this odd ratio was calculated based on overweight and obesity, sex, and sleep disturbances categories. The degree of heterogeneity in the meta-analysis was studied based on two tests and their results were reported; the first test is I2, and the results of this test were reported for all analyzes, and the second was χ2 test [59, 60]. Publication bias was investigated using tests (Egger [61], the trim-and-fill [62]), as well as graphical representations (Funnel plot). The results were analyzed with Stata-14 (Stata Corp. College Station, TX).
RESULTS
Selected studies
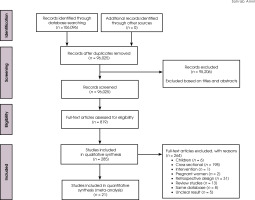
After searching the sources, 17,582, 27,315, and 61,199 articles were obtained from each of the information platforms PubMed, Scopus, and Embase respectively. After screening the studies based on Figure I and removing the duplicate studies and the unqualified studies based on the titles and abstracts, 819 articles were downloaded and collected in full text. After reading all these full texts, 534 articles were excluded. Out of the remaining 285 articles, 264 were removed on the basis of the reasons mentioned in Figure I, and finally 21 longitudinal studies [63-83] remained for this project.
Quality of selected studies
Table 1 describes the qualitative status of studies in five dimensions: selection bias, confounder’s bias, performance bias, data collection bias, and withdrawals/dropouts and missing data bias. For selection bias, the results showed that a total of 14 studies had a low bias, while 3 articles were moderate in bias and the rest displayed high bias. When it came to confounder’s bias, the frequency of high bias studies was higher. In terms of performance bias, all of the studies had a low and moderate bias. In the data collection method, six studies showed that the bias was low, and the rest showed moderate and high bias. In the component related to the withdrawals/ dropouts and missing data, thirteen studies had a low bias, and the rest of the articles showed moderate and high bias.
Table 1
Studies included in the meta-analysis
Body mass index and risk of sleep disturbances
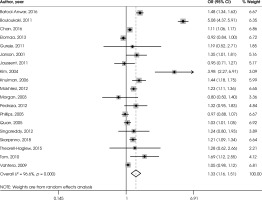
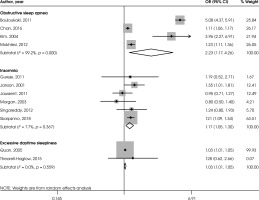
Figure II shows the association between BMI ≥ 25 and sleep disturbances. The odds ratio in this regard was 1.33 and the confidence interval was between 1.16-1.51 (n = 19; p < 0.001; I2 = 96.6%). For 2 studies that reported hazard ratio (HR), pooled HR was 2.10 and the confidence interval was between 0.40-11.01 (n = 2; p = 0.379; I2 = 97.4%).
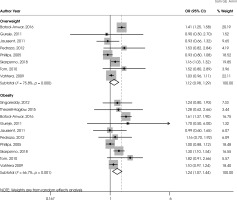
Figure III shows the association between overweight and obesity and sleep disturbances. The odds ratio was 1.12 and the confidence interval was between 0.98-1.29 (n = 8; p = 0.100; I2 = 75.8%) in overweight. The odds ratio was 1.24 and the confidence interval was between 1.07-1.44 (n = 10; p = 0.005; I2 = 66.7%) in obesity.
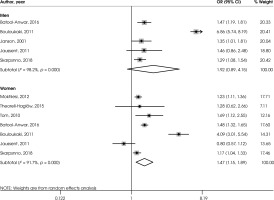
Figure IV shows the association between BMI ≥ 25 with sleep disturbances in men and women. The odds ratio was 1.92 and the confidence interval was between 0.89-4.15 (n = 5; p = 0.095; I2 = 98.2%) in men. The odds ratio was 1.47 and the confidence interval was between 1.15-1.89 (n = 7; p = 0.002; I2 = 91.7%) in women.
Figure V shows the association between BMI ≥ 25 and different types of sleep disturbance. The odds ratio was 2.23 and the confidence interval was between 1.17-4.26 (n = 4; p = 0.015; I2 = 99.2%) in obstructive sleep apnea. The odds ratio was 1.17 and the confidence interval was between 1.05-1.30 (n = 6; p = 0.004; I2 = 7.7%) in insomnia. The odds ratio was 1.03 and the confidence interval was between 1.01-1.05 (n = 2; p = 0.003; I2 = 0%) in excessive daytime sleepiness.
Heterogeneity and publication bias
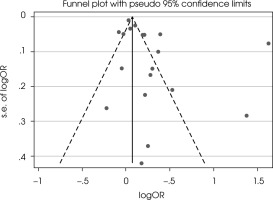
The results of the heterogeneity test showed that this index is at a high level [59] and equal to I2 = 96.6%, and the c2 test showed this result 537.23 (df = 18; p < 0.001) [31]. The funnel test in Figure VI showed that there was publication bias. The Egger (p = 0.071) test was also significant, indicating a publication bias [61]. The trim-and-fill [62] method imputed 6 missing studies, and the odds ratio increased to 1.59 and CI = 1.29-1.96 (Figure VI).
DISCUSSION
This study aimed to evaluate the risk of an individual experiencing sleep disturbances based on overweight and obesity, which was performed using systematic review and a meta-analysis of longitudinal meta-analyses. The first result of this meta-analysis was that a BMI above 25 increases the risk of sleep disturbances by up to 33%. This finding indicates the significant role that high BMI plays in the long term in increasing the risk of sleep disturbances. Also, discerning the relationship between overweight and obesity with the risk of sleep disturbances showed that with increasing BMI, the risk of sleep disturbances increases, so that obesity doubles the risk of sleep disturbances compared to overweigh. There seems to be a direct linear relationship between BMI and sleep disturbances; as the BMI increases, so does the risk of sleep disturbances. This finding is consistent with previous studies that have shown that increasing BMI increases the risk of sleep disturbances [49, 53]. In the relationship between overweight and obesity and sleep disturbances, we need to pay attention to other mechanisms. One mechanism is the effect of overweight and obesity on the increased risk of diabetes [84, 85]; diabetes, in turn, is recognized as a risk factor for sleep disorders [86, 87].
Another finding of the study showed that the risk of sleep disturbances in men with overweight and obesity is almost twice as high compared to men with normal weight. In women with overweight and obesity, the risk of sleep disturbances was almost half that of men. This indicates that the risk of sleep disturbances is higher in men than in women based on overweight and obesity. A previous meta-analysis showed that women with obesity were more likely than men to suffer from restless legs syndrome [53]. It has also been shown that the prevalence of insomnia is higher in women than in men [88, 89]. What is clear is that in the current meta-analysis, the focus was also on obstructive sleep syndrome, so this difference in results could be due to the varying prevalence of different types of sleep disturbances in men and women, as studies have shown that obstructive sleep syndrome has a higher prevalence in men compared to women [90-93]. On the other hand, it should be noted that the current study examined sex differences in sleep disturbances based on BMI, and therefore the results may be different from those that have dealt with the prevalence of sleep disturbances in men and women.
Another finding on the relationship between BMI and types of sleep disturbance showed that overweight and obesity have the highest risk for obstructive sleep apnea syndrome, doubling the risk of it. In the next ranks were insomnia and excessive daytime sleepiness. This high risk of obstructive sleep syndrome in people with obesity has been shown in studies to be up to three times higher than in normal-weight people [94-96]. Mechanisms through which obesity can increase the risk of obstructive sleep syndrome are listed [49], including an accumulation of fat in the respiratory tract and in the chest and abdomen that can cause problems with the respiratory system [49, 97, 98].
It should be noted that this study was able to provide a systematic review and meta-analysis of the association between BMI and sleep disturbances. On the other hand, overweight and obesity were studied separately, and also the results were studied based on sex and type of sleep disturbance. Due to the limitations of the existing literature, it was not possible to study other types of sleep disturbance. A methodological limitation was the high degree of heterogeneity in the studies included in the meta-analysis. Some studies included in the meta-analysis did not control confounder’s variables well, which is a limitation.
CONCLUSIONS
The present study showed that with increasing BMI, the risk of sleep disturbances increases. Considering that the role of overweight and obesity in many health problems has been identified, paying attention to the impact of overweight and obesity on sleep disturbances can play a vital role in levels of prevention as well as treatment. Therefore, this finding could provide insights into how to reduce the existing levels of sleep disturbances.