INTRODUCTION
Menopause is a natural and physiological phenomenon in a woman’s life that occurs in middle or late middle age (about 45 to 55 years of age) [1]. It is associated with complications such as hot flashes, night sweats, mood changes, sleep disorders, and changes in sexual desire and function [2]. Menopause can cause great, disabling stress in women who experience it [3, 4]. The hot flush is the most common complication in this period, and postmenopausal women referred to treatment clinics commonly complain of this complication. Hot flashes begin with the transition to menopause, and are characterized by a periodic increase in body temperature, and sudden sweats along with shivering, palpitations, and anxiety. This condition lasts from several seconds to several minutes (rarely lasting for as much as an hour), and its frequency is on average between 5 and 10 times a day [5]. The prevalence of hot flush is 67-82% in the United States [6], 70-85% in Europe [7], and 62.5-79.9% in Iran [8]. It is problematic for about 20-25% of women. Stress, increased central body temperature, drinking hot beverages and alcohol, physical activity, and emotional reactions can exacerbate hot flashes [9]. There are a variety of therapies to control this complication. Hormone therapy, for instance, is an effective method for their reduction of severity and frequency of hot flashes. However, the results of women’s health studies by the National Institute of Health have shown that there is a risk of breast cancer, thromboembolic complications, stroke, and heart disease in women receiving hormone therapy [10]. As a result, the use of this method has been withdrawn since 2003 [9]. Since non-hormonal mechanisms play a major role in hot flush pathophysiology, the use of new non-pharmacological therapies such as counseling and complementary and alternative therapies (CAM) including medicinal herbs (phytoestrogens), exercise, nutrition, and respiratory and relaxation techniques has received scholarly attention [11, 12].
In a study conducted by Bahri et al. (2017) [13] in Gonabad, Iran, 51.7% of the postmenopausal women studied were looking for treatment of menopausal symptoms, with hormone therapy (59.5%) being the most frequently used and acupuncture (2.9%) the least. In another study conducted by Obermeyer (2005) [14], two thirds of the Spanish women studied received treatment for menopausal symptoms, with 10% using hormone therapy and one fifth using complementary and alternative therapies. The rate of using complementary and alternative medicine among postmenopausal women was reported to be 91% in Lunny et al. (2010) [15]. Astrand et al. (2013) [16] found that relaxation techniques are significantly associated with a reduced rate of hot flashes. Counseling, especially the cognitive-behavioral approach, which is one of the practical methods in this respect, is nowadays proposed to postmenopausal women so that they can cope with hot flashes [9]. It helps patients identify and correct their distorted thinking patterns and inefficient behavior [17]. Counseling is performed in a variety of modes, including face-to-face, or by phone, video communication, and e-mail [18]. In this regard, phone counseling is a very useful and inexpensive option [19]. It is also a valid and reliable method with which to treat and follow up some diseases [20]. For example, Stefanopoulou et al. (2013) [21] showed that cognitive-behavioral therapy through self-help phone counseling led to a significant reduction in the severity and frequency of hot flashes and night sweats in postmenopausal women. The results of another study by Larroy et al. (2015) [22] in Spain showed that using cognitive-behavioral techniques led to a significant reduction in women’s hot flashes, depression, and anxiety. Green et al.’s study (2013) [23] in Canada showed a reduction in hot flashes in women receiving cognitive- behavioral therapy. Although counseling is one of the appropriate treatment methods for menopause symptoms, the best means of its implementation has not yet been discovered. Therefore, this study was conducted to compare the effect of face-to-face versus phone counseling based on cognitive behavioral therapies.
Methods
The present study was a parallel randomized controlled clinical trial. The design of this study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IR.AJUMS.REC. 2018.289). The study was registered in the Iranian Registry for Clinical Trials with the reference number (IRCT20180918041065N1). All women provided written informed consent prior to data collection, which began in December 2018 and finished in March 2019.
Study group and design
Based on the inclusion criteria of the study, a sample of n = 40 was selected from among post-menopausal women with complaints of hot flashes admitted to the gynecology clinic of the Imam Khomeini Hospital in Ahvaz, Iran. This sample size was calculated assuming a 95% confidence interval, a power of 90% [9], and a 10% attrition rate.
The women were eligible to participate in this study if they were aged 40 to 60 years, had normal menopause, with a minimum of one year and a maximum of five years after the end of their menopause, had at least 20 hot flashes per week for at least one month, were literate, and obtained a score more than one from the Kupperman hot flash index. The exclusion criteria were as follows: known psychological and physical illness, drug abuse, and the use of medications for hot flashes.
Eligible women were screened via phone and were briefed on the research procedure and its objectives. The women were assured that their information would remain confidential.
Measurements
Eligible women were asked to complete a demographic questionnaire and Kupperman Index. They received a diary to record their daily symptoms of hot flashes and night sweats. Out of the 48 eligible women invited to the clinic, 40 signed the consent form. After the conducting of the interviews and the necessary examinations, the participants were randomly assigned into phone or face-to-face counseling groups using the permuted block technique with a block size of 4 and allocation ratio of 1 : 1. The phone counseling group received 6 weekly 30-40-minute counseling sessions based on cognitive-behavioral therapy. Due to the need for direct training on breathing and relaxation techniques and how to complete the diary, and in order to monitor the correct performance of the tasks, Sessions 1 and 4 were held in person while the other 4 sessions were held via phone. The face-to-face counseling group received 6 weekly 30-60-minute cognitive-behavioral counseling sessions. The members of both groups received an audio CD on breathing and relaxation techniques for daily practice. The Kupperman index was completed by both groups at the outset of the study, and immediately and 8 weeks after the completion of the intervention.
Due to the nature of this study, the blinding of researchers and participants was not possible, but after randomization, the codes dedicated to each participant were kept with the clinic clerk for concealed preservation. Therefore, neither the participants nor the researcher was aware of the allocation order until the commencement of intervention.
Statistical analysis
All data were analyzed using SPSS version 22. For continuous and categorical data an independent t-test and χ2 test were used, respectively. The paired t-test was used for comparison of pre- and post-intervention scores. Because the measurements were repeated three times (before, immediately after, and as a follow-up), repeated measures ANCOVA was used to show the differences between the two groups in these three measurements. Cohen’s d effect size was used to indicate the standardized difference between two means in the independent t-test. P < 0.05 was considered statistically significant.
Results
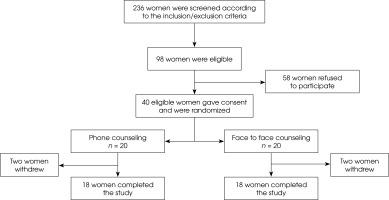
In this study, of the 40 participants initially invited 36 completed the study in face-to-face and phone counseling groups (Figure I). The results showed that the groups did not differ significantly in terms of age, duration of experience of menopause, body mass index, educational attainment, economic status, and other demographic characteristics (Table 1).
Table 1
Demographic characteristics of participants in the two study groups
The results showed a significant within-group difference between the phone and face-to face groups in terms of the frequency, severity, and duration of hot flashes, as well as the frequency and severity of night sweats before, immediately, and eight weeks after intervention (p < 0.001). The weekly frequency of hot flashes decreased after the intervention in both groups (from 31.92 ± 7.98 to 18.83 ± 7.35 in the face-to-face group vs. from 33.32 ± 7.77 to 19.53 ± 7.7 in the phone counseling group). Hot flash severity was reduced from 2.24 ± 0.28 to 1.21 ± 0.23 in the face-to-face group while in the phone counseling group it fell from 2.23 ± 0.24 to 1.20 ± 0.18. Hot flash duration was reduced from 4.22 ± 1.17 min to 2.79 ± 0.91 min in the face-to-face group whereas the phone counseling group experienced a decrease from 4.29 ± 1.23 min to 2.68 ± 0.95 min.
Night sweat frequency was reduced from 2.34 ± 0.31 to 1.21 ± 0.24 in the face-to face group in comparison to 2.33 ± 0.31 to 1.14 ± 0.16 in the phone counseling group. Also, night sweat severity was reduced from 1.70 ± 0.34 to 1.03 ± 0.29 in the face-to-face group compared to 1.59 ± 0.34 to 1.01 ± 0.30 in the phone counseling group. The effect of the intervention in both groups still persisted 8 weeks after the completion of intervention.
Although within-group differences in both groups were significant (p < 0.001), the between-group comparison showed that there was no significant difference between the two groups regarding the mentioned variables (Table 2). The effect size (Cohen’s d) for independent t-test was < 0.003, which shows that the differences between the two interventions were negligible.
Tables 2
Frequency, severity and duration of hot flashes, and the frequency and severity of night sweats in two groups receiving face-to-face and phone counseling
Discussion
This study was designed to compare the effects of phone versus face-to-face counseling based on the cognitive behavioral therapy for hot flashes and night sweats in postmenopausal women.
Hot flash is the most common and annoying complication in postmenopausal women, reducing their quality of life [5]. Several therapeutic approaches, including cognitive-behavioral therapy, have been proposed to mitigate against the effects of this complication. The results of statistical comparisons in the present study showed that the two counseling groups did not differ in terms of the factors affecting hot flashes, and the effect size was too small to identify any difference between the groups, indicating that the two groups did not show any difference. Thus, any change in the symptoms of the participants in the two groups could be attributed to the use of CBT. The results of this study suggest the significant effect of different methods of cognitive-behavioral therapy with the same protocol on reducing vasomotor symptoms in postmenopausal women. Hardy et al. (2018) [24] found that cognitive-behavioral therapy applied in a self-help manner significantly reduced the severity and frequency of hot flashes and night sweats at 6 and 20 weeks after the intervention. Ayers et al. (2012) [9] also found that cognitive-behavioral therapy had a significant effect on reducing the severity of hot flashes and night sweats in both self-help and group counseling contexts. The results of research conducted by Mann (2012) [17] showed that the use of cognitive-behavioral therapy could significantly reduce the severity of hot flashes and night sweats in postmenopausal women suffering from cancer.
In recent years, counseling has been proposed as one of the methods with which to help women cope with hot flashes, and cognitive-behavioral therapy has been one of the practical counseling approaches in this regard [9]. This approach can be used as an intervention method that can reduce menopausal complications and help patients identify distorted thinking patterns and ineffective behaviors through regular discussions and structured behavioral assignments (Mann et al., 2012) [17]. It is also aimed at presenting adaptive coping responses and controlling negative emotions by correcting false interpretations, guiding negative self-talk, and correcting irrational patterns of thinking and ineffective recognition [25]. Several studies have reported the positive effects of cognitive-behavioral therapies in health-related areas, including the reduction of menopausal symptoms. Phone counseling is one of the most useful and inexpensive methods [19], leading to economic savings, improved service quality [26], and reduced work load on the health system [27]. In many advanced medical centers around the world, phone counseling is used to reduce costs and unnecessary visits. One of the disadvantages of this method, however, is the potential risk of things being missed in counseling due to the lack of visual cues and non-verbal communication, which causes the consultant to rely on the voice of clients rather than paying attention to the visual cues [11]. The results of the present study showed that the way cognitive-behavioral therapy counseling is implemented has no effect on the outcome, and that both face-to-face and phone methods can be equally effective. Thus, given the benefits of phone counseling, this method can be recommended for the reduction of the vasomotor symptoms in postmenopausal women who have difficulty reaching treatment centers in person.
Limitations of the study
In this study, the severity and frequency of hot flashes and night sweats were examined before, immediately after, and eight weeks after intervention. Assessment of the frequency and severity of hot flashes and night sweats was made on the basis of the diaries completed by the participants, which may have been affected by recall bias. Second, mental examination of the participants and their possible mental disorders such as depression were not assessed by standard questionnaires in this study, and this may have affected the severity of hot flashes and night sweats.
Conclusions
According to the results of this study, the use of face-to-face and phone counseling based on cognitive behavioral therapy could significantly reduce the severity, frequency and duration of hot flashes as well as the severity and frequency of night sweats, with no significant difference being observed between the two intervention methods. Using phone counseling for women who have difficulty attending the clinic is recommended. Also, other studies with larger sample sizes could add to our knowledge in this respect.