Dermatofibrosarcoma protuberans (DFSP) is a rare soft tissue tumor of unknown etiology [1]. It accounts for less than 1% of all soft tissue sarcomas and is considered an intermediate-grade malignancy [1, 2]. Although the risk of metastasis is low, the tumor presents a high local recurrence rate. DFSP typically involves dermis and subcutaneous tissue. It usually presents as a slowly growing plaque on the trunk of young adults [1]. Excisional biopsy is recommended to reach a definitive diagnosis, however, a punch biopsy that includes subcutaneous adipose tissue may also be performed [3]. DFSP is composed of spindle cells that demonstrate immunohistochemical positivity for CD34, while markers such as factor XIIIa, alpha smooth muscle actin, S-100, desmin and melan-A are negative [1, 2]. The standard treatment is wide local excision, since recurrent tumors tend to be more destructive [3].
Herein, we present a 75-year-old male patient who was admitted with a 2-year history of an erythematous plaque on the right thigh and was diagnosed with DFSP.
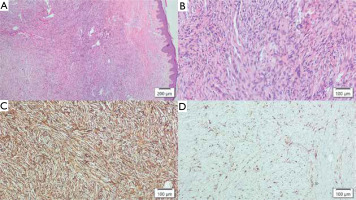
A 75-year-old Caucasian male was admitted with a slightly pruritic, erythematous plaque on the thigh, which had been gradually increasing in size for the last two years. The patient stated that he did not receive any previous treatment. The past medical history was notable for hypertension, while the family history was unremarkable. Dermatological examination revealed an erythematous, firm plaque with overlying nodules on the extensor surface of the right thigh (fig. 1 A). Dermatoscopic evaluation showed a pinkish background with structureless hypopigmented areas that may be consistent with DFSP (fig. 1 B). A skin biopsy was performed, and histopathological examination of the specimen confirmed the diagnosis of DFSP (figs. 2 A–D).
Figure 1
A – Erythematous plaque on the right thigh with crusted ulceration secondary to punch biopsy. B – Dermatoscopic view of the plaque at 20× magnification
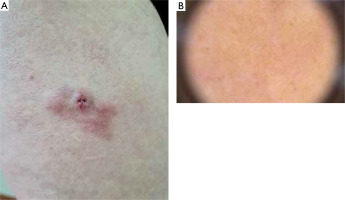
Figure 2
A – Histopathological examination revealed a tumoral lesion composed of spindle-shaped cells with eosinophilic cytoplasm and mild nuclear atypia within the dermis and subcutaneous fat (hematoxylin and eosin 40×). B – Mitoses and necrotic changes were not detected (hematoxylin and eosin 200×). C – Immunohistochemistry revealed spindle-shaped cells to be CD34+ (100×). D – Sparse dendritic cells stained with factor XIIIa (100×)
Among the laboratory tests, the complete blood count revealed a decreased mean platelet volume (8.2 fl, reference range: 9.1–11.9 fl) and an increased absolute basophil count (0.1 × 103/μl, reference range: 0.01–0.07 × 103/μl). The biochemistry panel was within normal limits, except for an elevated blood glucose level (125 mg/dl, reference range: 74–100 mg/dl). Ultrasonography showed reactive cervical lymph nodes measuring less than 1 cm, as well as reactive lymph nodes in the bilateral inguinal regions, with a maximum size of 40 × 10 mm on the right and 22 × 9 mm on the left). Magnetic resonance imaging (MRI) of the right thigh revealed a 16 × 9 mm soft tissue lesion demonstrating heterogeneous enhancement following contrast administration. The lesion was confined to the skin and subcutaneous tissue without a muscle involvement. Therefore, surgical excision was recommended for the treatment of the tumor and the patient was referred to the department of plastic and reconstructive surgery.
DFSP is a rare tumor of the skin and subcutaneous tissue with an annual incidence of 0.8 to 4.5 per million. The muscles and fascia may also be involved [1]. The tumor affects females more commonly compared to males. It usually occurs in young and middle-aged individuals, between the ages of 25 and 45 years [2]. Skin trauma has been implicated in the development of DFSP, however, the etiopathogenesis of the disease remains unknown. The chromosomal translocation t(17;22)(q22;q13) contributes to its pathogenesis by leading to the formation of the abnormal fusion protein COL1A1-PDGFB [4]. DFSP is characterized by a slow-growing, asymptomatic, skin-colored or hyperpigmented plaque [1]. If left untreated, the lesion may progress to nodules or tumors, and may eventually ulcerate or bleed [3]. The trunk is the most commonly affected site, however, the shoulders and pelvic area can also be involved [1]. The differential diagnosis of DFSP should include spindle cell lipoma, melanoma, keloid, morphea, dermatofibroma and angiosarcoma clinically, and cellular fibrous histiocytoma, solitary fibrous tumor and cutaneous leiomyosarcoma histopathologically [4, 5]. The definitive diagnosis of DFSP is made based on histopathological examination. Contrast-enhanced MRI is used to assess the extent of the tumor, while computed tomography shows bone involvement. Surgical excision is the treatment of choice [6]. Distant metastasis is rare and reported in 1% to 4% of patients [1]. The rate of local recurrence can be as high as 60% even after wide local excision [6]. The case we presented is a good example of DFSP. Prompt diagnosis and timely intervention are crucial to prevent this rare tumor from invading deeper layers of the skin and underlying tissues. Given the high local recurrence rates, close and long-term follow-up is of utmost importance in the management of patients with DFSP.








