INTRODUCTION
Striae distensae, also known as stretch marks, are common linear scars that occur as a result of dermal damage secondary to extensive skin stretching [1]. They are typically associated with rapid weight gain, pregnancy, or systemic corticosteroid use. A remarkably rare phenomenon where interstitial fluid collecting within pre-existing striae distensae may occur in conditions characterized by severe edema such as heart failure, renal impairment, or hypoalbuminemia [2].
OBJECTIVE
Here, we present 2 cases of patients with fluid-filled striae distensae due to hypoalbuminemia of different origin.
CASE REPORT
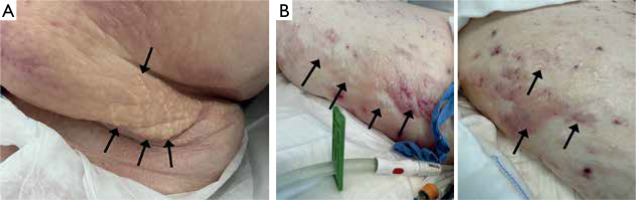
A 30-year-old Caucasian male patient with a history of epilepsy, congenital hearing loss, hypothyroidism, cholecystolithiasis, and obesity was admitted to the intensive care unit due to acute respiratory failure secondary to septic shock. Physical examination revealed generalized edema and numerous linear, fluid-filled skin lesions within pre-existing striae distensae on both of his thighs that flattened with pressure (fig. 1 A). Laboratory investigations showed normal liver function test, blood glucose, and renal function tests, however, sodium and C-reactive protein (CRP) values were increased. Moreover, complete blood count was disrupted and marked hypoalbuminemia (serum albumin 19 [normal 35–50] g/l; urinary total protein 0.26 g/l) was present most probably secondary to sepsis. The lesions resolved gradually following diuresis, nevertheless, the patient’s condition remained serious due to multiple disease burden.
The other patient, a 45-year-old Caucasian female, was admitted to the cardiac intensive care unit for further management of acute heart failure. Medical history was significant for cardiogenic shock, myocarditis, alopecia totalis, paroxysmal supraventricular tachycardia, obesity, and HIV. On examination, linear tense bullae located unilaterally on the skin of the abdomen were found (fig. 1 B). The skin lesions were located within the pre-existing stretch marks after pregnancy. Laboratory tests performed revealed hypoalbuminemia (serum albumin 23 [normal 35–50] g/l), elevated NT-proBNP (24541 [normal < 125] pg/ml), increased CRP level (46 [normal < 5] g/l), and anemia (9.2 [normal 12–15] g/dl). Moreover, left ventricular ejection fraction (LVEF) measured by echocardiography was 17%. The skin lesions gradually disappeared as the patient’s clinical state stabilized, specifically as the albumin levels normalized and the cardiac parameters improved.
DISCUSSION
Fluid-filled striae distensae result from fluid accumulation within pre-existing stretch marks. The pathogenesis is multifaceted, with links, confirmed in the literature, to nephrotic syndrome, heart failure, and systemic lupus erythematosus [3–5]. Lower oncotic pressure caused by hypoalbuminemia is assumed to be the unifying trait of the above. As a result, the fluid leaks into the extravascular regions causing edema. On the other hand, the production of inflammatory cytokines during sepsis enhances vascular permeability and promotes fluid leakage which was the most probable cause in our first patient. While it is a well-established fact that skin within striae distensae is weaker due to less elastin, collagen, and fibrillin contents, excessive fluid accumulates preferentially within the stretch marks [1, 6]. Thus far, no particular treatment has been suggested. Although puncture and aspiration of fluids alone would cause fast fluid re-accumulation, addressing the underlying disease with diuresis can result in a spontaneous remission.
CONCLUSIONS
Fluid accumulation within striae distensae is a benign phenomenon sparsely reported in the medical literature, yet it can present dramatically. Awareness of this unusual skin finding in patients with edema can prevent excessive and unnecessary interventions. In the differential diagnosis, bullous infections and autoimmune skin with bullae conditions must be taken into consideration. A dermatologist’s role in identifying such lesions remains fundamental.