PURPOSE
This case report aims to increase our knowledge about neuropsychiatric disorder as one of the comorbidities of the disease. Tic is a purposeless movement involving several muscle groups, with repetitive movement patterns which vary from one individual to another. Tourette syndrome is a complex neuropsychiatric disorder characterized by motor and vocal tics; it can be found in children and young adults aged 5 to 21, most frequently in children with an average age of 6 [1]. Prevalence in ethnic groups is similar worldwide but is rare in African Americans. There are more male sufferers than female ones, at a ratio of 4 : 1 [2]. Several studies have identified genetic factors, such as Slit and Trk-like 1 (SLITRK1) and histidine decarboxylase (HDC) genes, which are correlated with Tourette syndrome. However, the research has yielded no consistent results to date [3]. Here, we report on a case of an intellectual disability patient with Tourette syndrome; it is hoped that increased knowledge and a better understanding of the pathophysiology of the disease may help with the management of it.
CASE DESCRIPTION
The 12-year-old patient’s parents reported that he had uncontrolled repetitive movements throughout the body since he was one year old. The first symptoms appeared, simultaneously, with the involuntary blinking of an eye, facial grimacing and shrugging of the shoulders. According to his mother, these movements have become more frequent as the patient ages. When the patient is tense or stressed, these movements happen more often. However, when the patient is sleeping, they seem to happen less often, but are still present occasionally. When these movements occur, the patient always makes sounds like hiccups. This is the patient’s first visit since the complaint appeared.
The patient was born normal at term, with a birth weight of 3,200 grams. His growth and development were within normal limits. The family realized that the patient had a slower understanding compared to his classmates when he was seven years old. The family also complained about the patient’s emotional characteristics and low cooperative abilities, which were difficult to control. There was no history of these complaints in the family.
The patient’s vital signs were within normal limits. On examination, he showed an involuntary movement that met the criteria for motor tics followed by vocal tics (hiccups). To exclude metabolic disorders, we performed laboratory tests such as complete blood count, renal function test, liver function test, and electrolyte concentrations; all were within normal limits. Electroencephalography showed a generalized diffuse slowing of brain activity with a frequency of 5-6 Hz, suggesting generalized mild encephalopathy (Figure I). A contrast-enhanced head MRI showed bilateral hippocampal sclerosis with decreased hippocampal volume (Figure II).
Figure I
Electroencephalography showed generalized diffuse slowing of brain activity with a frequency of 5-6 Hz, which suggests generalized mild encephalopathy
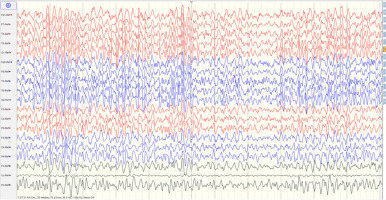
Figure II
Magnetic resonance imaging showed bilateral hippocampal sclerosis with decreased volume of both hippocampi

We diagnosed the patient with Tourette syndrome and consulted the pediatric and adolescent psychiatry departments to look for comorbidities. The patient could not complete the Wechsler IQ test due to being unco-operative but scored 82 on the Kaufman Brief Intelligence Test 2nd edition (below average). The psychiatry department assessed the patient with mild intellectual disability and behavioral impairment. The patient was then scheduled for psychoeducation and supportive therapy. For pharmacological therapy, we avoid using neuroleptics due to potential significant side effects such as sedation, extrapyramidal syndrome, and weight gain. The patient was treated with nightly doses of 10 mg clonazepam every 24 hours and sodium valproate every 12 hours.
After a week of treatment, the patient returned to a state of improved control with less movement than before, and was scheduled for relaxation therapy and supportive psychotherapy in child and adolescent psychiatry.
COMMENT
Tourette syndrome is a movement disorder characterized by motor and vocal tics. According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) classification, it is a neuropsychiatric developmental disorder characterized by multiple motor and vocal tics for one year, with onset in childhood or adolescence and appearing in the first and second decades, so there is a suspicion that a brain development disorder causes this syndrome [1, 2]. The presence of neurodevelopmental disorders like ADHD, autism spectrum disorders, and intellectual disability might be a sign of Tourette syndrome [4].
The criteria for Tourette syndrome, in the DSM-V, are given below:
Multiple motor symptoms and one or more vocal tics are present at some time during the illness although not necessarily concurrently.
The tics may wax or wane in frequency but have persisted for more than 1 year since the first tic onset.
Onset is before age 18 years.
The disturbance is not attributable to the physiological effects of a substance (e.g., cocaine) or a general medical condition (e.g., Huntington’s disease, post-viral encephalitis) [5].
The global prevalence of Tourette syndrome has been estimated to be 0.5% [6]. The symptoms of Tourette syndrome begin in childhood and among pre-school age children at 3-9/1,000. The average age at which the first episode of motor tics occurs is 4-6 years. The syndrome is more common in males than in females, with a prevalence of 3-4 : 1. The exact cause is thought to be related to polygenic hereditary disorders, where several different genes are involved in the disorder. The negative effects of the environment such as maternal stress in pregnancy, smoking, infections, fetal hypoxia, and stressful events in the child’s life may also contribute [7].
Tics are defined as sudden, rapid, recurrent, non-rhythmic motor movements or vocalization, generally preceded by urge [5]. Tics in Tourette syndrome can be simple or complex movements. Simple movements involve a single muscle group, such as blinking an eye and contraction of the facial muscles, neck, or shoulders. Complex movements involve coordinated movements such as kicking, jumping, scratching, and dystonic movements [2]. Vocal tics are also grouped into simple and complex sounds. Simple vocal tics are grunting, clearing, hiccupping, sniffing, and other sounds, while complex ones can take the form of coprolalia, echolalia, palilalia, and others [8].
The most common and mildest of the idiopathic tic disorders is the transient tic disorder of childhood. This can be differentiated from Tourette syndrome as it does not last for more than 1 year [5]. Another form of tic disorder is persistent (chronic) motor or vocal tic disorder. Both Tourette syndrome and persistent (chronic) motor or vocal tic disorder are indicated by the presence of tics for longer than one year (though intervening tic-free periods are recognized). Persistent (chronic) motor or vocal tic disorder is diagnosed when individuals have exhibited either motor or vocal tics (but not both) at some time during the illness. When both motor and vocal tics have occurred during the course of the disease, though not necessarily concurrently, Tourette syndrome is diagnosed [9].
The pathophysiology of Tourette syndrome is thought to be caused by disturbances in the cortex inhibition of the motoric tracts that are generated in basal ganglia, and also the involvement of the cortico-striatal-thalamic-cortical (CSTC) circuit and neurotransmitters such as dopamine, GABA, and glutamate, leading to disinhibition in the motor and limbic systems. The localization of the tic disorder is unclear, but imaging evidence suggests a decrease in caudate volume compared to the normal population [10]. Some MRIs also show prefrontal, frontal, sensorimotor, cingulate, and temporal changes [8].
As many as 86-90% of patients with Tourette syndrome have at least one comorbid condition or coexisting neuropsychological problem. Children with Tourette syndrome have problems with executive function, such as lower IQ test results, impaired visual perception, and low visual-motor abilities [8]. Learning disorders begin at school and are characterized by low levels of competence in academic skills such as reading, writing, and arithmetic [10]. Learning problems at school are caused by motor tics that get in the way of reading or writing. A social problem also arises due to rejection from classmates and teachers [4].
Diagnosis is made by observation of clinical signs and is supported by the presence of a comorbid behavioral disorder. The result of neurological examination is usually normal, and only tics are found. Computed tomography (CT) scans of the head and MRI are usually normal. However, there is evidence of structural changes in the limbic structures (such as the amygdala and hippocampus) on some MRIs for their functional roles on the CSTC circuit. This patient’s MRI showed a reduced volume of the bilateral hippocampus, which explained his learning disability [10]. This patient’s MRI also showed bilateral hippocampal sclerosis. Hippocampal sclerosis (HS) is the most frequent histopathology found in patients with temporal lobe epilepsy (TLE) [11]. The causes of HS are still controversial and likely multifactorial, such as prolonged febrile seizures (FS). A FEBSTAT study suggests that children with pro-longed FS may have acute hippocampal injury and an increased frequency of hippocampal developmental change. Several family studies have provided some evidence for a genetic predisposition to HS [12].
We have also performed EEG in this patient to differentiate tics from an epileptic seizure. The EEG has evidently showed a generalized diffuse slowing of the brain activity with a frequency of 5-6 Hz, which suggests generalized mild encephalopathy, this is a diagnosis about which we still have some doubts. Some causes of encephalopathy in childhood are multifactorial, whereas others, such as previous viral infection or hepatic or uremic encephalopathy, have a known etiology. Encephalopathy caused by genetic abnormalities such as CPT2 and SCN1A is also being studied [13].
The management of patients with Tourette syndrome does not consist of medication alone. It is necessary to further evaluate the comorbid neuropsychiatric conditions of the patient. The pharmacological management of Tourette syndrome is highly individualized because the severity of the tics can is not uniform, and the comorbidity is different. Some literature shows that antipsychotics have good efficacy but are often avoided because of the undesirable side effect of drowsiness. For our patient, we avoided the antipsychotics due to the side effects. The patient was given sodium valproate instead because we believe it can control the tics by regulating the central GABA function [14]. Benzodiazepines, such as clonazepam, were added to mitigate the tics and alleviate compulsivity directly [10]. In addition to pharmacotherapy, it is also necessary to use neurobehavioral management methods with comorbid patients. Social shame and discomfort usually require professional intervention. For successful and sustainable management of Tourette syndrome, the clinician should focus on educating the family and supporting the patient [2].
Other specific and alternative therapies such as botulinum toxin, neurosurgery, and deep brain stimulation have not yet been considered for this patient, since he has shown a good outcome with the current management. From the literature, most children with Tourette syndrome experience the greatest severity of tics in their early adolescence and will gradually improve as they grow older and their comorbidities are treated [15]. This patient is still being monitored for his global functioning and the tics. Further genetic testing is still unavailable in our center.
The overall prognosis of Tourette syndrome is that it is relatively benign, and most affected children can grow up to work and live as healthy adults. Nearly half of the pediatric patients with Tourette syndrome will have complete remission in adolescence or adulthood, and about another 30% will have alleviated tics in adulthood; up to 20% of the patients will have deferred tics into adulthood, or the rest of their lives [16].
CONCLUSIONS
Tourette syndrome affects up to 1% of the population. Intellectual disability is one of the comorbidities in TS. Management strategies are highly individual. Neuroleptics are the drugs of choice for tic management, but have potential side effects that may not benefit the patient. Psychoeducation and supportive therapy for the comorbid condition often improve the patient’s quality of life.







