INTRODUCTION
For almost two years, the world has been struggling with the global pandemic caused by the spread of the SARS-CoV-2 coronavirus, which first appeared in the city of Wuhan, Hubei province, China in late 2019. In early 2020, the disease caused by the virus was designated as COVID-19, and on March 11, 2020, WHO declared it to be a pandemic. The clinical course of the disease varies from mild or even asymptomatic to severe respiratory failure and death. The prognosis is worse in the elderly and in patients with comorbidities. So far, it has been shown that over 80% of deaths from COVID-19 are among people over 60 years old [1-3]. According to WHO [4], almost 250 million people in the world have been infected and almost 5 million have died. The first case of COVID-19 in Poland was recorded on March 4, 2020, and by November 8, 2021 more than 3 million people were infected, of whom almost 80,000 had died. Of the confirmed cases worldwide, health care workers accounted for 6% [5].
COVID-19, like other contagious diseases which cause epidemics, affects not only physical health but also mental functioning. As a global threat to public health it requires drastic control measures and has disrupted almost every aspect of everyday life [6]. Fear of infection, danger to life and health, isolation, reduced social contact, school and workplace closures, and significant restrictions on activity and freedoms can all be stressful for society as a whole. However, health care workers are the group most exposed to stress. From the beginning of the pandemic, thousands of health care workers have been infected with COVID-19, and many have died. In such a dramatic situation, doctors are exposed to high risk of contracting the disease, as well as increased risk of developing mental health symptoms [7, 8]. The risk of infection, and working with higher workloads in terms of working hours and patient numbers may lead to severe stress [9]. This has already been proven during previous SARS and Ebola pandemics [10, 11].
Increased levels of stress among medical workers may be a result of the fear of COVID-19 [12]. Human fear is a hallmark of any epidemic. During the COVID-19 pandemic, there is fear of being infected, of dying and losing a loved one, and of contact with people who might be infected [13]. Fear is related to the speed at which the virus spreads. People also fear the serious health complications of COVID 19, forced hospitalization, and long periods of quarantine. Another cause of fear is the possibility of spreading the infection to relatives who may not survive the disease. Fear of the coronavirus stems from its novelty, and uncertainty as to how the epidemic will develop. Therefore, the fear of COVID-19 is much greater than the fear of seasonal flu [1].
Since the outbreak began, a huge amount of research has been published on the mental health effects of the outbreak among health care workers. Although the burden, stress and anxiety of health care workers are often studied, their job satisfaction during an epidemic has been much less analyzed. There is as yet not much research on how the psychological consequences of COVID-19 affect the occupational functioning of health care workers. Since unmanaged fear related to COVID-19 can potentially lead to long-term effects on job performance and job satisfaction, leading to frequent absenteeism and possible job rotation [14, 15], it is extremely important to analyze whether the fear of COVID-19 is related to perceived stress and job satisfaction.
Job satisfaction can be defined as a feeling of pleasure or unpleasantness, experienced as a result of performing specific roles or tasks [16]. Its consequences are having negative or positive feelings towards the duties performed at work [17]. People who are satisfied with their work show more initiative, are open to various opportunities and new patterns, and show greater loyalty to the employer and the workplace [18]. It can be said that the dimension of professional satisfaction is influenced by subjective assessment, emotions experienced, and reflection. People with a high level of job satisfaction feel that they have achieved success. They believe that their work brings joy and allows them to implement certain values. Job satisfaction includes two aspects: the cognitive, related to what the employee thinks about their work, and the emotional, consisting of the employee’s feelings in relation to the work performed [19]. The emotional aspect includes emotional experiences at work and attitude towards the profession. It is believed that the emotional aspect can be considered a positive or negative dimension of a person’s emotions in relation to work or its assessment as satisfactory or unsatisfactory.
Based on theoretical concepts about job satisfaction, it can be assumed that the fear of COVID-19 experienced at work due to the spread of the coronavirus and the stress associated with additional burdens will be negatively related to job satisfaction. Many studies to date have shown a link between fear of COVID-19 and stress [20-22], including among healthcare professionals [12]. Studies also show that fear of COVID-19 reduces job satisfaction and increases health care workers’ willingness to change jobs [23]. Many studies conducted during the pandemic have shown that fear of COVID-19 can act as a mediator, e.g. between stress-related uncertainty and well-being [24] or between perceived risk and welfare [25].
Therefore, the aim of our research was to determine the relationship between fear of COVID-19, stress and job satisfaction. Based on data from the literature, we hypothesize that: (1) fear of COVID-19 is correlated with job satisfaction and perceived stress; (2) fear of COVID-19 and perceived stress are predictors of job satisfaction; (3) fear of COVID-19 mediates the relationship between perceived stress and job satisfaction.
METHODS
Participants
The study included 97 doctors. Taking into account age, the largest group were those aged 41-50 (n = 37). There were 61 women and 36 men. Most respondents lived in small-sized cities (n = 52) and worked in hospital wards other than those directly dealing with infectious diseases (n = 45). Most of doctors in our sample reported that they were not in a high-risk group for COVID-19 (n = 65) (Table 1).
Table 1
Descriptive statistics of the surveyed group of doctors (N = 97)
Research methods
Three questionnaires were used in the study. The perceived level of stress was measured with the Perceived Stress Scale (PSS-10) [26]. This is a 10-item questionnaire with a 0-4 answer scale (0 – never; 4 – very often). It showed good psychometric properties in the current study (Cronbach’s α = 0.87).
Fear of the coronavirus was measured with the Fear of COVID-19 Scale (FOC-6) [20] – a 6-item questionnaire with a 1 (strongly disagree) to 5 (strongly agree) scale. The sample items are: “I’m afraid of losing my life due to coronavirus infection” and “I am afraid of serious health complications due to coronavirus infection”. They represent emotional reactions of fear caused by the coronavirus pandemic. The scale presented good psychometric properties (Cronbach’s α = 0.79).
Job satisfaction was measured with the Brief Job Satisfaction Scale (BJSS,) which is the Polish adaptation of the Bray-field and Roche scale [27]. The scale measures the cognitive aspect of overall job satisfaction, using five statements, for example: “I am quite happy with my current job”. The Cronbach’s α reliability for the sample was 0.88.
Procedure
The study was conducted at the beginning of the COVID-19 pandemic in Poland. The participants were doctors from the Provincial Specialist Hospital in Czestochowa and Hospice Care in Czestochowa. Due to the epidemiological threat, the surveyed doctors received a questionnaire in the electronic form. They were informed about the anonymity of the study and that they could discontinue completing the survey at any time and without giving any reason. All doctors gave their informed consent to participate in this study.
RESULTS
The mean scores of scales used were perceived stress (M = 22.18), fear of COVID-19 (M = 22.98) and job satisfaction (19.31). To verify correlational relations between perceived stress, job satisfaction and fear of COVID-19 it was decided to perform Pearson’s r correlation analysis. It turned out that fear of COVID-19 is correlated with job satisfaction (r = –0.21; p = 0.035) and perceived stress (r = 0.35; p < 0.001). The relationship between work satisfaction and perceived stress is also statistically significant (r = –0.39; p < 0.001) (Table 2).
Table 2
Pearson’s r correlation coefficients in the group of doctors (N = 97)
| 1 | 2 | 3 | |
|---|---|---|---|
| 1. Perceived stress | –0.39 | 0.35 | |
| 2. Job satisfaction | –0.39 | –0.21 | |
| 3. Fear of COVID-19 | 0.35 | –0.21 |
Regression assumptions were checked in order to find out the extent to which the variance in job satisfaction is explained by perceived stress and fear of COVID-19. According to the Durbin-Watson test (DW = 1.73) residuals were not autocorrelated. The variance inflation factor for predictors (VIF = 1.55) was lower than 10, which is considered as a threshold value for collinearity [28].
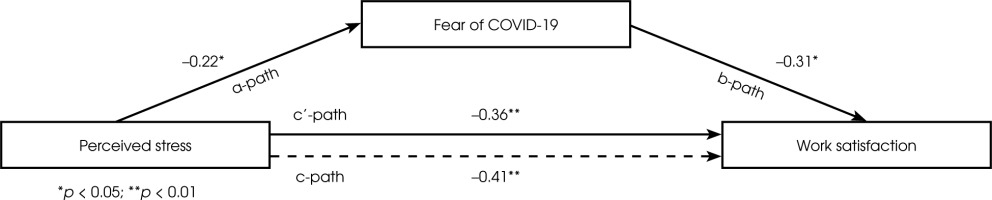
To assess the influence of fear of COVID-19 on the relationship between perceived stress and work satisfaction (Figure I), a mediation analysis was performed. We used PROCESS 3.4 macro [29] with 5000 bootstrapped samples and 95% confidence intervals. The standardized regression coefficient between perceived stress and fear of COVID-19 was statistically significant and positive (β = 0.22; 95% CI: 0.07; 0.38). Regression of fear of COVID-19 and work satisfaction was negative, and significant (β = 0.23; 95% CI: –0.43; –0.02). The direct effect was also significant and negative (β = –0.36; 95% CI: –0.49; –0.02). The total effect had the same direction and was stronger (β = –0.41; 95% CI: –0.49; –0.22). It appeared that fear of COVID-19 is a significant mediator in this model (completely standardized indirect effect [β = –0.07; 95% CI: –0.10; –0.01]). It increases the negative impact of perceived stress on work satisfaction. More detailed results are presented in Table 3.
Table 3
Mediation role of fear of COVID-19 in the relationship between perceived stress and work satisfaction in the group of doctors (N = 97) – detailed results
| Path | β | SE | t | p | 95% CI | |
|---|---|---|---|---|---|---|
| LLCI | ULCI | |||||
| X -> M | 0.22 | 0.07 | 2.99 | 0.04 | 0.07 0.38 | |
| M -> Y | –0.23 | 0.10 | –2.23 | 0.03 | –0.43 –0.02 | |
| X -> Y | –-0.41 | 0.07 | –6.26 | < 0.001 | –0.49 –0.22 | |
| X(M) -> Y | –0.36 | 0.07 | –5.30 | < 0.001 | –0.49 –0.02 | |
DISCUSSION
The COVID-19 outbreak has affected almost every aspect of human life. The high prevalence of the virus, its novelty and highly contagious nature, and the associated morbidity and mortality rates are related to an unprecedented demand for health care workers. Therefore, it can be said without doubt that COVID-19 is a significant source of stress for medical workers. One of the methods used to measure the level of perceived stress is the PSS-10 scale, which is being widely used by researchers during the current pandemic. In current research we found that the level of stress experienced by doctors is high. The current study’s mean result in the PSS-10 questionnaire (22.18) is higher compared to the result recorded for the general Polish population during the current pandemic (20.6) [30]. It is also higher than the population average (< 13 according to Cohen [31]); 16.6 for the Polish population according to Juczyński [32]. It is, however, slightly lower than the average level of stress experienced by Polish nurses (26.26) [12].
During the pandemic many new demands have been placed on healthcare professionals. These demands must be met by an already exhausted workforce which has been even more depleted due to infection or self-isolation. The crisis caused by COVID-19 is putting enormous pressure on doctors. They experience an increase in the intensity of their work and have to adapt to new protocols. Many critically ill patients have appeared in hospitals and doctors observe their deaths on a daily basis [12]. Therefore, it is not surprising that perceived stress is related to fear of COVID-19. This relationship has already been demonstrated in many studies [20-22], including among healthcare professionals [12, 23]. The fear of COVID-19 experienced by health care workers may be similar to that of the general population. During the COVID-19 pandemic this has involved fear of being infected, of dying and losing a loved one, and of contact with people who might be infected [13]. People also fear the serious health complications of COVID-19, hospitalization, and prolonged quarantine [1]. In addition to the fear that is typical of the population, doctors can feel fear because of a lack of personal protective equipment, no access to COVID-19 testing, fear of transmitting coronavirus at work and unknowingly infecting others. Medical workers are also afraid of working in an infectious diseases ward unfamiliar to them and the lack of accurate information about COVID-19 [33].
Medical workers during are exposed during the pandemic to a greater workload [34, 35] a greater risk of infection and greater physical and mental stress [36-38], which is a challenge for their job satisfaction. Therefore, work in life- and health-threatening conditions, during which one feels fear and stress, may be less satisfying. In the current study we found that fear of COVID-19 and perceived stress are related to job satisfaction. The stronger the perceived stress and the greater the fear, the lower the job satisfaction. The study has also shown that perceived stress and fear of COVID-19, as predictors of work satisfaction, turned out to be statistically significant and explained 15.7% of job satisfaction variance. Fear of COVID-19 was a mediator between perceived stress and job satisfaction. It increases the negative impact of perceived stress on job satisfaction. Doctors feel stressed because they are overloaded with work in difficult conditions, and their health and lives are at risk due to the pandemic. In addition, contact with people who are sick or dying, and news about colleagues and co-workers who have been infected or have died increases fear of COVID-19. The fear of COVID-19, of being infected, complications, and spreading the virus to others makes work more threatening than satisfying. Because healthcare professionals are directly involved in patient care, the risk of contracting COVID-19 is higher than in the general population. This can contribute to the fear of infection or unknowingly infecting others, including family members or friends. In addition, concerns about the pandemic, such as increased patient numbers and patient burden, shortage of personal protective equipment [39], social distancing and community quarantine may exacerbate fear among medical workers, affecting their mental and emotional well-being and their work performance and satisfaction.
Although the job satisfaction of health care workers is not as often studied and analyzed as fear and stress during a pandemic, several studies have already been conducted to assess job satisfaction among medical professionals during the pandemic and the variables associated with it. One of the first of these studies was that of Yu et al. [40]. This study defined the job satisfaction of medical staff as “relatively decent”. Factors affecting job satisfaction include education, years of work experience, pandemic-related shift in working hours, and length of daily sleep.
One study found that health care workers experiencing a high level of fear are more likely to believe conspiracy theories and that the virus was produced in a laboratory. The same study found that belief in a conspiracy theory was associated with lower job satisfaction among health care professionals [41]. Based on this, it can be concluded that the fear of COVID-19 prompts the use of defense mechanisms and reduces job satisfaction. Studies have also shown that fear of COVID-19 reduces job satisfaction and increases the willingness of nurses to change jobs. As a psychological response to a threatening situation or stimulus, the fear of the coronavirus can affect medical workers’ productivity, leading to higher levels of job dissatisfaction and an increased desire to leave the organization and profession [23]. This finding is congruent with previous research in other sectors in which workers who exhibited a high level of fear found work events more stressful, affecting their overall performance and job satisfaction [42, 43].
Another study found that access to personal protective equipment and the risk of COVID-19 infection were predictors of the job satisfaction of healthcare professionals. Fear of COVID-19 may be related to the risk of infection, which increases when PPE (personal protective equipment) is scarce. Access by healthcare professionals to PPE was associated with better physical health and job satisfaction, and less stress. In addition, it was shown that health care workers who were unsure whether they had COVID-19 were significantly more stressed, depressed, and anxious, and had less job satisfaction. This finding suggests the need to prioritize health care tests, when tests are available, or otherwise prioritize them for mental health support. Working under conditions of stress, depression, anxiety and lower job satisfaction over a long period of time can be very harmful to healthcare professionals in this unprecedented health crisis [44].
Job satisfaction is very important for health care workers, especially during the COVID-19 pandemic. Good job satisfaction favors productivity and is key to the quality of healthcare and the effectiveness of epidemic prevention. Job satisfaction is related to how the work environment meets the needs of the individual and how the individual is able to meet the demands of the work. During the pandemic, these demands on healthcare professionals have increased dramatically and the responsibilities of many have changed. The COVID-19 outbreak has led to severe stress in the healthcare community, which has worsened the physical and mental health of healthcare workers. Healthcare workers face existing social pressures and increased responsibilities, resulting in a less satisfying working environment [45].
Despite obtaining significant results, the study is not free from limitations. The presented mediation models are treated as causal; however, the analyzes applied do not allow to us to make inferences about the direction of the impact of the tested variables. In order to verify the presented relationships more accurately, more advanced qualitative longitudinal studies should be performed. It would also be worth conducting research on a larger number of healthcare professionals and conducting further research on a group of healthcare professionals taking into account other factors. It is also worth noting that the level of job satisfaction of health care workers during the pandemic may be influenced by other factors, such as personal resources [46], coping strategies [47], personality factors [48], and a sense of threat and risk perception [12].
CONCLUSIONS
In this research we found that fear of COVID-19 was a mediator between perceived stress and job satisfaction. It increases the negative impact of perceived stress on job satisfaction. Research emphasizes that the mental well-being of health care workers, including their fear and stress, is very important for their functioning in the workplace and for the effectiveness of their work, maintaining their employment and performance at work. Research also shows that the mental health of health care workers has a significant impact on their professional functioning. This is especially important in places where healthcare resources are already limited, such as hospitals treating people with COVID-19 [38]. Working psychologically on fear of COVID-19, ensuring staff availability for testing, PPE, and vaccination as soon as possible can improve healthcare professionals’ well-being, reduce stress levels and increase job satisfaction.