Introduction
Alzheimer’s disease is a progressive and irreversible form of dementia that affects cognitive functions and the ability to function independently. The etiology of the disease is still not fully understood. It is most often diagnosed in people over the age of 65, but also in younger individuals [1]. Characteristic symptoms of the disease include memory loss, difficulties in everyday activities, disorientation, problems with concentration and spatial orientation, and many other disorders related to the improper functioning of the brain [2]. According to the Institute for Health Metrics and Evaluations (IHME), in Poland in 2019, the estimated percentage of people suffering from Alzheimer’s disease and related diseases was 1.5% (585,000 people), which was 0.2 percent higher than in 2014. In 2022, in Poland, 357,000 people were diagnosed with Alzheimer’s disease and related diseases [3]. The clinical picture of the brain of a person with Alzheimer’s disease shows the accumulation of proteins in and around cells – amyloid and tau proteins [4]. The former are extracellular beta-amyloid protein aggregates formed by the breakdown of the precursor protein – amyloid. The most important is the soluble form, which spreads with the cerebrospinal fluid and binds to receptors in the brain. The second element playing role in the pathogenesis of Alzheimer’s disease are neurofibrillary tangles caused by the entanglement of incorrectly hyperphosphorylated tau protein [1]. However, the clinical picture is not identical in all patients. Only in later stages the disease produces characteristic symptoms [5]. This is due to the presence of over 20 subtypes of the disease (based on the OMIM database).
Aim of the work
The aim of the study is to conduct molecular analysis of the role of the apolipoprotein E (APOE) gene as a risk factor for Alzheimer’s disease and lipid metabolism disorders. By carefully examining the molecular mechanisms involved in the expression of the APOE gene and its interactions with the processes of lipid metabolism, authors of the study aim to better understand the pathophysiological mechanisms of Alzheimer’s disease and the potential links with lipid disorders. The analysis may lead to identification of new therapeutic targets and preventive strategies in the treatment and prevention of Alzheimer’s disease and related lipid metabolism disorders.
Methods
To prepare this review paper, databases, such as PubMed, Google Scholar and PEDro were comprehensively searched. The keywords included “APOE”, “Alzheimer disease”, “mutation”, “APOE diseases” and “Alzheimer’s disease”. The search was limited to articles published between the years 1980 and 2023, with the greatest focus on the last 10 years. The first stage of the selection was based on the analysis of titles and abstracts for compliance with inclusion and exclusion criteria. This analysis helped in selecting articles consistent with the topic of the paper. The next stage of the study included thorough assessment of the full texts of potentially eligible articles and the selection of the most relevant information.
Literature review results
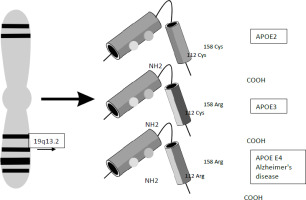
Mutations in the APOE gene, which is responsible for the production of the apolipoprotein E protein – APOE, are one of the factors that increase the risk of Alzheimer’s disease and cardiovascular disorders [6]. The APOE gene is located on the long arm of chromosome 19 q13.2 [7]. It has three isoforms Ɛ2 (APOE ε2) rs28931578, Ɛ3 (APOE ε3) rs121918393, Ɛ4 (APOE ε4) rs7412 or rs429358 [8]. The structure of the isoforms is shown in Figure 1. Individual isoforms are created when amino acids, arginine and cysteine, are present in codons 112 and 158 of the APOE gene [9]. An increased risk of Alzheimer’s disease is observed in the presence of the APOE ε4 isoform [10]. This is related to the impact on the microglia reactivity, abnormal lipid transport and glucose metabolism, as well as reduced synaptic integrity and plasticity. However, the APOE ε2 polymorphism reduces the likelihood of developing Alzheimer’s disease (protective function), despite the development of amyloid β pathology. A difference in the structure of isoforms is the result of non-synonymous mutations, and the consequent changes in the structural and functional properties of the protein [11].
Figure 1
The structure of three isoforms of the APOE gene located on chromosome 19 at position q13.2 Source: Own elaboration based on [12-14].
Apoliprotein E is an important element in the regulation of cholesterol homeostasis. APOE ε2 protein, which contains cysteine at position 158, binds incorrectly to LDL receptors, with the consequent increase in the concentration of atherogenic lipoproteins. The presence of arginine at position 112 in the APOE ε4 isoform results in an increase in LDL levels because it binds to low-density lipoproteins [15]. Apoliprotein E is a protein responsible for the metabolism of lipoproteins involved in the transport of lipids in the bloodstream; it is a marker of neurodegenerative diseases and cardiovascular disorders. APOE gene polymorphisms may have antagonistic effects in viral infections. For instance, the presence of APOE ε4 protein is associated with the increased susceptibility to the herpes simplex and HIV infection. However, it protects against the hepatitis B and C virus infection. This is related to the structure and functionality of the molecule. In people with APOE ε4 and the reduced LDL receptor concentration, HCV or HBV virus is bound to the cell. In HIV infection, this isoform has a lower affinity for binding to the lipoprotein receptor 1 (LRP1) than other isoforms [16]. Apoliprotein E also affects amyloid β, the protein which accumulates in the brain of a sick person, forming the so-called amyloid plaques. It has the property of transforming from the α-helix conformation into β-sheets, which initiates further conformational changes, including the formation of oligomers of this conformer and, ultimately, amyloid fibrils. Research on amyloid β peptide has shown that it can be removed from the brain by lipoprotein receptors, with its accumulation when lipid transport is impaired [17]. Pathogenic variants of the APOE gene lead to phenotypic changes by altering the lipid metabolism of tissues and cells. This results in the development of certain diseases [18].
Type III hyperlipoproteinemia
Type III hyperlipoproteinemia, also called familial hypercholesterolemia, is a rare type of mixed hyperlipidemia in which cholesterol and triglyceride levels are above the normal value [2,7]. The disease may be associated with mutations in two places of the APOE gene, which are inherited in an autosomal recessive manner and lead to impaired fat metabolism [19]. The incidence of the disease in the population is from 1 to 5 cases per 5,000 individuals. The disease is associated with the appearance of a homozygous allele of apolipoprotein 2 (APOE ε2), NM_000041.2(APOE):c.526C>T (p.Arg176Cys) according to the ClinVar database. The presence of this variant contributes to warfarin resistance. However, the mere presence of this polymorphism does not result in the development of the disease. Other genetic and environmental factors must be present for the condition to develop [20]. Type III hyperlipoproteinemia may be asymptomatic. Long- term increases in the levels of blood lipids (e.g. due to obesity) and their accumulation in the body predispose to clinical symptoms. They include yellow petechiae on the skin (deposits) filled with lipids, pancreatitis and atherosclerosis [18,19]. Atherosclerosis is associated with an increase in the amount of low-density lipoproteins and a decrease in the level of high-density lipoproteins. Atherosclerotic plaques are formed, leading to the inflammation of the walls of the arteries, the consequent smaller lumen of the blood vessel and the reduced blood flow to the heart [21].
Sea blue histiocyte disease
Sea blue histiocyte disease is an autosomally inherited disease. The disease, which is also called lipemic splenomegaly, takes its name from the fact that when stained under a microscope, some histiocytes appear light blue [22]. Characteristic symptoms of the disease are increased levels of triglycerides and enlarged spleen [23]. Additionally, a low number of platelets – thrombopenia, as well as abnormal functioning of the liver and heart are observed [22]. The disease is induced by a pathogenic leucine deletion mutation in the APOE gene at position 149. This is the receptor-binding area of the APOE molecule [24]. The manifestation of the disease is influenced by gender, lipid concentration and the presence of other diseases [23].
Lipid metabolism disorders
Dyslipidemia is one of the diseases associated with lipid metabolism disorders. In this condition, too few enzymes that break down lipids are produced or they function incorrectly. As a result, harmful amounts of lipids are accumulated and cells and tissues are damaged, including the brain, liver and spleen [24]. Dyslipidemia may be caused by genetic changes (primary) or external factors (secondary). Obesity is closely related to dyslipidemia [25]. The APOE ε4 polymorphism is mainly responsible for the development of this disease [26,27]. Apopoliproteins influence the development of obesity through lipid metabolism, energy expenditure and the inflammatory response [25,27]. The level of APOE gene expression is related to lipid metabolism abnormalities and the degree of obesity – the higher the TG (triglyceride) level, the lower the concentration of APOE proteins [26].
Alzheimer’s disease
The exact causes of Alzheimer’s disease are not known, but the development of the disorder may be influenced by various factors, both genetic (e.g. APOE gene polymorphism) and environmental, of which old age is most often mentioned [28]. Education also has an impact on the development of Alzheimer’s disease. Dementia is more often noticed in people who have completed education earlier than in those with higher education. Gender is also mentioned among predisposing factors, with women being more likely to develop the disease [3]. Also, social factor plays a role. A loner, who spends most of time alone and avoids contact with other people, is at higher risk of developing the disease. Other predisposing factors include diet and stimulants, in particular alcohol and cigarettes [29,30]. Alzheimer’s disease is a neurodegenerative disorder in which neurons are lost. Genetic changes are observed mainly in the following genes: APP – In approximately 15% of Alzheimer’s disease in younger patients, PSEN1 – approximately 80% of cases, PSEN2 – in 5% [29]. The pathogenic effect is most closely related to the APOE ε4 polymorphism. This factor is expressed in over 50% of patients, but it has not been thoroughly investigated. The risk of Alzheimer’s disease with two APOE ε4 alleles increases up to 12 times. The process of lipidation with the participation of ABCA1 and ABCG1 enzymes is important to the formation of functional APOE protein. The reduced amount of ABCA1 leads to the smaller amount of APOE protein, which quickly degrades [31]. The presence of APOE ε4 does not determine the development of Alzheimer’s disease, but these people are at risk [29]. APOE ε4 is also associated with abnormal synaptic plasticity and hippocampal volume loss, leading to the loss of dendritic spines [31]. Genetic tests for factors predisposing to the development of Alzheimer’s disease are still being developed. Diagnostics for the presence of the APOE gene, especially APOE ε4, is performed only in clinical tests. The test cannot clearly determine whether a person is just a carrier of an abnormal variant or whether he or she already suffers from Alzheimer’s disease [32]. Magnetic resonance imaging is also important in diagnostics. The technique is used to detect atrophy of the temporal lobe, but it may also show other neurodegenerative diseases. PET examination allows for an early and differential diagnosis. The test uses a glucose analogue for the identification of regions where glucose metabolism in the brain has been reduced [33].
Conclusions
The APOE gene, which is responsible for the production of APOE protein, is associated with the development of cardiovascular disorders and Alzheimer’s disease. There are three polymorphic forms: Ɛ2 (APOE ε2), Ɛ3 (APOE ε3) and Ɛ4 (APOE ε4). Apoliprotein E is responsible for the metabolism of lipoproteins related to the transport of lipids in the bloodstream, and cholesterol homeostasis. The presence of any of these polymorphisms may lead to the development of type III hyperlipoprotinemia and atherosclerosis, as well as sea blue histiocyte disease, lipid metabolism disorders and Alzheimer’s disease. Mutations in the APOE protein can cause lipid metabolism disorders. However, their presence alone does not translate into the manifestation of the disease as other environmental factors and diet also have their influence. Alzheimer’s disease is the most common disorder associated with the APOE gene. Studies have shown that the development of this disease is most closely related to the APOE ε4 polymorphism. It is expressed in over 50% of patients, and its appearance in both alleles increases the risk of the disease by as much as 12 times. However, the presence of APOE ε4 alone does not determine the development of the disease. The most frequent risk factors of the disease are age and gender. Diagnosing Alzheimer’s disease is not easy as genetic tests are constantly being improved and are only performed in clinical trials.







