Introduction
The term “weekend effect” applies to patients admitted during a weekend (Saturday or Sunday) rather than on a weekday. Many hospitals operate at reduced staffing capacity during weekends, a situation that suggests hospital care during weekends is of quality limited enough to increase the risk of complications over patients admitted during a weekday when the hospital is fully staffed.
Acute pancreatitis, a systemic disease, develops when premature activation of pancreatic proenzymes causes acute inflammation of the pancreas. The damage that results varies in severity according to the damage done to the pancreas, adjacent tissues, and even organs elsewhere in the body.
The incidence of acute pancreatitis (AP) has been trending upward in recent years, with a current average of 72 cases per 100,000 people in the general population [1]. Of all gastrointestinal and liver diseases, AP is ranked as the 14th highest to cause death [2]. The mortality rate for AP in general is between 2% and 10%, but the mortality rate increases to approximately 30% when fulminant AP is diagnosed [3].
A limited number of recent studies have found an increase in mortality rates for some acute medical conditions when patients are admitted for hospitalisation during a weekend [4]. This increased mortality rate may be the result of increased severity of illness rather than weekend admission, even when admitted to hospitals that operate under limited staffing conditions during weekends [5].
Previous studies suggest a number of factors that might account for increased mortality and morbidity rates during weekends, including a reduction in medical staff, limited resources, and restricted access to diagnostic and therapeutic tools [6, 7]. Some studies have demonstrated unfavourable outcomes of the weekend effect on certain medical conditions such as pneumonia [8], acute kidney injury [9], and dysrhythmia [10]; favourable outcomes for these medical conditions rely on time-sensitive interventions and admission to intensive-care units. The findings of these studies have generated a significant degree of discussion on the validity of the weekend effect and its relationship to reduction in-hospital staffing practices for weekend shifts, a bias toward disease severity, and comorbidities associated with patients seeking hospital care during the weekend [11, 12].
There is little known at this time, however, on the weekend effect on AP specifically, even though the incidence of the condition has increased during the past 20 years [13, 14]. Two recent retrospective studies evaluated the differences in outcome for AP patients admitted during the week versus those admitted on a weekend and found no increased in-hospital mortality between the two groups, suggesting there is no weekend effect when treating AP [15, 16].
Aim
This prospective, observational study focused on a single medical facility operating under jurisdiction of the Department of Gastroenterology in Poland. Our goal was to evaluate the relationship between AP outcomes and weekend admissions to the hospital.
Material and methods
A total of 126 prospective patients were included in this study. Each patient was assessed using the revised Atlanta criteria and each was observed until discharge or in-hospital death. A subsequent comparison between weekend and weekday admissions was made for aetiology, severity of disease, length of hospital stay, and in-hospital mortality.
All patients in the study were admitted to the Department of Gastroenterology of the Central Clinical Hospital of the Ministry of Interior (Poland) and each diagnosed with AP disease onset within 48 h prior to admission. Each patient was recruited for the study within 24 h of hospitalisation (n = 126).
This observational study was conducted at the Department of Gastroenterology of the Central Clinical Hospital of the Ministry of Interior in Poland. Each of the 126 patients was diagnosed with AP within 24 h of admittance; this assessment, based on the revised Atlanta criteria, included establishing a score based on the Bedside Index of Severity in Acute Pancreatitis (BISAP). Diagnosis was also based on physical examination, serum lipase and/or amylase levels ≥ 3 times the upper normal limit, and computed tomography (CT), magnetic resonance imaging (MRI), or ultrasonography (US). Organ failure was assessed with the Modified Marshall Scoring System.
Acute pancreatitis diagnosis was based of any two of these three features:
Abdominal pain typically associated with AP.
Serum lipase and/or amylase levels ≥ 3 times the upper normal limit.
Findings that suggest AP when using CT, MRI or US for diagnosis.
The presence of persistent organ failure occurring for more than 48 h was the basis for classifying patients as having severe (SAP) or moderate (MAP) acute pancreatitis [17]. The Modified Marshall Scoring System was used to determine the presence of organ failure. The Bedside Index of Severity in Acute Pancreatitis (BISAP) score was determined for all patients within 24 h after hospitalisation.
Guidelines for treatment established by the Polish Pancreatic Club [18] were followed when treating the patients in the study. The hospital ward under study operated 7 days a week, and the workload was not significantly reduced on weekends. Weekend admission was defined as occurring on either Saturday or Sunday. Saturday SAP admissions (n = 7) were higher to a statistically significant degree than Sunday admissions (n = 2), leading to the decision to expand the study to compare Saturday admissions against all other days of the week. Even when compared to all other days, Saturday admissions were the highest proportionally.
Results
Patients were divided into two groups based on the day each was admitted for hospitalisation: weekday (n = 99; 78.6%) or weekend admission (n = 27; 21.4%). Tables I and II show the baseline characteristics of all study participants. All were well matched with no statistically significant differences between the groups.
Table I
Characteristics of patients with AP included in the study
Table II
Factors associated with the severity of AP, grouped and compared by time of week
Of the group admitted during the weekend, the impact of AP aetiology was found not to be statistically different (p > 0.623).
Thirty-three patients were diagnosed with severe AP (SAP) (n = 33, 26.2%), 37 moderately severe (MSAP) (29.4%), and mild AP (MAP) was diagnosed in 56 (44.4%) patients.
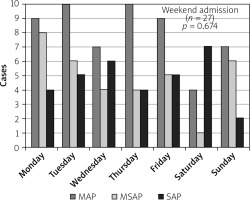
Diagnostic distribution of SAP was found to be not statistically significant between the two groups (p > 0.674) (Figure 1).
Figure 1
Distribution of severity of AP by day of week
AP – acute pancreatitis, SAP - severe acute pancreatitis, MSAP – moderately severe acute pancreatitis, MAP – moderate acute pancreatitis.
The in-hospital mortality rates between the weekday and weekend admissions were also found not to be significantly different: 5 (5.1%) for weekday admissions versus 1 (3.7%) for weekend admissions, with p = 1.000.
Additionally, no statistically significant differences in length of hospital stay were found between the two groups. The median hospital stay was 9 days for those admitted during the week and 10 days for weekend admissions (p > 0.714) (Table III).
Table III
Severity, length of hospitalisation, and in-hospital mortality of patients admitted with AP, grouped and compared by time of week
During the course of the study, seven SAP patients were admitted on Saturday and two on Sunday. When Saturday admissions were compared to admissions occurring on other days of the week, there were no statically significant differences with regard to AP severity (p > 0.58), in-hospital mortalities (p > 0.81), and length of hospital stay (p > 0.68).
Discussion
An increase in mortality rates for patients admitted to hospitals during weekends is becoming a global concern. The term weekend effect is often used to explain this increase in mortality. Unsubstantiated conclusions have been drawn as to probable causes of the weekend effect on mortality rates, including healthcare management policies that encourage limited care and hinder 24/7 access to life-saving diagnostic and therapeutic procedures, as suggested by Freemantle et al. [19]. Logistical and organisational processes, along with a critical reduction in weekend staffing policies, are all thought to contribute to the weekend effect.
Other studies, however, dispute or question the existence of the weekend effect, especially with regard to AP. Martin McKee identifies previous studies that do identify the weekend effect affecting stroke patients in the United Kingdom (UK), but also identifies a study that finds that the riskiest time for admission for stroke in the UK is a weekday night [20]. There is the real possibility that the level of care and mortality rates vary according to time of admission, as presented by Pauls et al., but the Pauls study was not observational – it was a meta-analysis of 97 studies covering 51 million patients admitted to hospitals for all reasons every day of the week [21]. There is little agreement, however, on the possible causes of the weekend effect and their ramifications on outcomes based on time and/or day of admission for hospitalisation. It is likely that any weekend effects are driven by mechanisms more complex, multi-faceted, and difficult to prove than merely the day of admission.
It is also likely that patients seeking medical care during weekends are in much greater distress than those who wait to see their doctor by appointment the following week. This immediate need for medical intervention might indicate a patient-related factor that explains the difference in outcomes between weekend and weekday admissions. Zhou et al., however, expand the weekend effect to the “off-hours effect”, to include hospitalisation on weekday nights as well as weekends, while Mikulich et al. found that “sicker patients, with a worse outcome” were more likely to be hospitalised on weekends rather than week days [4, 22]. These and numerous other explanations suggest the weekend effect should not be attributed solely to weekend staffing issues and/or accessibility to diagnostic tools and treatment options.
The findings of our study strengthen the argument that there are no statistically significant differences for AP patient outcome regardless of the day of hospital admission at the facility under study. This lack of statistical difference pertains to AP severity, length of stay, and in-hospital mortality rates. These findings are of particular interest in light of the major positive impact achieved by implementing managerial guidelines defined by the Polish Pancreatic Club at the Department of Gastroenterology where the study was conducted.
The number of SAP patients admitted on Saturday (n = 7) identified such an imbalance from the number admitted on Sunday (n = 2) that we decided to expand the study to compare Saturday admissions with admissions on all other days of the week. The hypothesis that the weekend effect is actually a Saturday effect was not corroborated by our work. We found no increased risk of unfavourable outcome for AP patients admitted on Saturday rather than any other day of the week.
When we compared similar, basic endpoints for SAP patients admitted on different days of the week, we found no weekend effect on patient outcomes. A similar population-based, observational study from Japan found results similar to ours, strengthening our finding that the weekend effect on SAP patients has yet to be proven. Hamada et al. concluded that “adjustments to weekend staffing and selective hospital referral of patients admitted at weekends are not indicated for severe acute pancreatitis” [15].
A study by Sharma et al. found that weekend AP admissions were notably linked to ileus and alcohol withdrawal. Patients with these complications were found to be at greater risk for development of acute respiratory distress syndrome, but their risk for in-hospital mortality did not follow the weekend effect theory [16].
We acknowledge that our study was limited to a small number of AP patients hospitalised at a single institution, but it was an observational, prospective study, which relied on systematic observation of patients in real time throughout their hospital stay. This study is not a retrospective analysis of details derived from a database or research conducted by others. Our findings suggest that the diversity of the patient cohort and the hospital system’s ability to respond accordingly may suggest, but do not prove, a weekend effect, a finding that cannot be found when relying solely on Hospital Episode Statistics.
Our work does not support the hypothesis that the weekend effect is a universal phenomenon although it does not rule out the possibility of a weekend effect when associated with certain specific patient subgroups. It is possible that the weekend effect can be felt when a facility interrupts continuity of care during weekend shifts. Scheduled hospitalisations and the absence of patient-centred checklists may exacerbate any perceived weekend effect.
We recommend that all patients admitted for AP be reviewed by a gastroenterologist in the early stage of hospitalisation. We consider this review to be important for identifying high-risk patients and those whose health status is unstable. Care of these patients should be prioritised as early after admittance as possible. Early diagnosis of SAP is essential for providing the best course of treatment and most favourable outcomes, regardless of the day of the week the patient is hospitalised [23–26].
We summarise the findings of this study as follows:
When treating patients according to the current practices recommended by the Polish Pancreatic Club, patients admitted to this facility faced no greater baseline risk when admitted during the weekend than those admitted during the week.
There was no statistical difference in in-hospital mortality rates between the weekend and weekday groups.
Improved outcomes for treatment of AP can be achieved by implementing relevant and systematic policies and practices within the healthcare unit even in the absence of pharmacological therapy targeted specifically for AP.
We find multiple clinical implications from this study that may prove beneficial in enhancing the care of patients hospitalised during a weekend. First, this study illustrates the value of consistently following best practices for AP treatment and providing the same or similar levels of care for all AP patients, regardless of the day of the week they are admitted to the hospital.
Additionally, an abundance of published literature on the weekend effect focuses on the phenomenon itself rather than on solutions taken to mitigate the effect. While it is important to identify the presence of a weekend effect when it affects certain situations or conditions, it is equally important to design and develop methods to overcome the weekend effect in facilities where these procedures do not exist. One such method might be to increase weekend staffing, so levels of care are consistent with those that the patient experiences during the week.









