Issues raised by a national-level analysis of burnout, well-being, and self-reported medical errors among physicians have raised significant attention worldwide [1, 2]. However, healthcare workers’ physical and mental exhaustion and its impact on their conduct and professional discharge have been lurking for quite some time. While previously well-hidden and embroiled with the frantic rhythms of our daily lives, the pandemic-related stress, often fueled by social and political upheaval, has exposed intrinsic, work-associated strains and injuries interfering with one’s ability to uphold the Hippocratic oath. Nevertheless, ostrich-like behavior or disdaining a problem has never yielded favorable outcomes. It may sound paradoxical, but we should ‘embrace’ the recent major epidemiologic crisis to unearth such issues; we believe this will allow bold ideas to manage the problem.
Burnout is common among physicians. It concerns medical professionals of various healthcare sectors and disciplines. For instance, in a Professional Life Survey of the American College of Cardiology (ACC), addressing burnout and its drivers, authors reported “that approximately 27% of U.S. cardiologists were burned out, while almost 50% of cardiologists reported being stressed with less energy“ [3]. In addition, women report more burnout than men (45.3% vs. 33.5%). It is noteworthy that mid-career cardiologists present the highest levels of burnout (45.3%) compared with early-career (35.4%) and late-career ones (31.5%). Burnout was highest among cardiologists who worked > 60 h per week (41.5% of whom reported burnout) and those who relayed a ‘hectic work environment’. Approximately 40% of German psychiatrists reported having had a history of depression, and 31% of Canadian psychiatrists endorsed having had an experience with mental illness [4]. However, the excess risk of suicide is even more shocking, with a 40% higher risk in men and 130% in women. In a recent systematic review, Ong et al. [5] presented data from 11 studies, reporting a high prevalence of burnout among gastroenterologists, ranging from 18.3% to 64.4%. Burnout symptoms showed a geographical variation associated with work overload, age, and gender [5]. There are also well-documented burnout issues related to ethnicity and perceived isolation from most of the population [6].
However, despite a variety of reports addressing burnout among healthcare professionals, there are some critical methodological problems with the definition itself. Across the studies, burnout has not been measured in a uniform way as various authors proposed different definitions, suggesting it was just stress, other say it is a form of depression or chronic tiredness. According to the Merriam-Webster dictionary, burnout is defined as “exhaustion of physical or emotional strength or motivation usually as a result of prolonged stress or frustration or to cause to fail, wear out, or become exhausted especially from overwork or overuse”. In medical environment, “burnout” can be defined as negative psychological symptoms, triggered by chronic exposure to stressors at workplace [7]. The major components of burnout include (i) emotional and physical exhaustion, (ii) depersonalization, and (iii) decreased sense of personal accomplishment. Top drivers of burnout include the system (e.g. work load, efficiency, flexibility and/or control and community at work) and individual-related stressor (e.g. work-life integration, culture and values or meaning in work) and can be used to provide a basis for identifying factors aggravating and alleviating burnout among healthcare professionals [8]. In this data background, the micro and macro-environment of the human condition do not lend themselves readily to all or nothing decision of overly simplistic patient management pathways. As physicians, we need to learn from the paradox of hypotheses of quantum mechanics, where random events are tolerated to infinite yet impractical levels. Wiliam Osler’s words ‘The good physician treats the disease; the great physician treats the patient who has the disease’, seem more apt now. Indeed, holistic medicine remains both science and art. As most of the studies addressing the problem of burnout in healthcare at the same time show relatively high discrepancies in its prevalence rates. This observation calls for a systematic approach in future studies in order to translate the data into daily practice [9].
Recent surveys results are in line with conclusions of previously published polls, where less experience, younger age and hours spent at a hospital, those working at weekends or involved in legal medical issues, doctors lacking autonomy, administrative support or with a poor workplace or home relationships reported a more severe burnout effect [7, 10]. Furthermore, burnout in healthcare seems to be of concern among all medical societies as it may severely alter physicians’ health-inducing depression, risk of substance misuse, or increase the risk of suicide. In addition, biological changes were observed because of burnout, such as hypertension, myocardial infarction and increased cortisol levels, maladaptive behavior such as disordered eating, drug and alcohol abuse, and more social consequences such as isolation and relationship breakdown.
Notably, most of these reports come from the era before the COVID-19 pandemic, bringing new and extraordinary demands on all medical professionals. With all the national healthcare systems under significant strain, it is worth mentioning that the numbers of physicians per 100,000 population are low, and the profession in some countries is in turmoil [8, 11]. It is known that physician burnout negatively impacts patient care [9, 12]. Concerns have been raised lately about the increased rate of possible resignations, which can set off a chain reaction known as ‘turnover contagion’ [10, 13]. Furthermore, a meta-analysis by Salyers et al. shows a strong association between physician burnout and suboptimal quality of care, patient safety, and patient satisfaction [11, 14]. Based on their conservative base-case model on a simulated population of U.S. physicians, Han et al. estimated that more than $4.5 billion in costs related to physician turnovers and reduced clinical hours were attributable to burnout each year in the U.S. [12, 15]. The authors suggested substantial economic value for policy and expenditures devoted to burnout reduction programs for medical doctors [12, 15].
As the number of patients with cancers, psychiatric and neurodegenerative diseases, and gut-brain interaction disorders (DGBIs) will rise, physician burnout should be considered inevitable. Therefore, we need new solutions to maintain physicians’ health and quality of medical care. In addition, the recent pandemic has significantly impacted psychology and outcomes, even those not directly affected [13, 16]. In the pro-COVID-19 era, strategies such as self-knowledge, self-awareness, mentorship, and professional coaching were suggested as solutions. However, all these strategies seem ineffective as the COVID-19 crisis reveals a more accurate scale of the global healthcare systems’ gaps, deficits, and deficiencies.
Our group has been involved in the COH-FIT (The Collaborative Outcomes study on Health and Functioning during Infection Times – https://www.coh-fit.com) project. COH-FIT aims to collect global data to understand better the impact of the COVID-19 pandemic on physical and mental health in various population groups, including healthcare workers, who could be at increased risk of poor health and well-being during infection. We aim to assess, quantify and understand the impact of the COVID-19 pandemic and related protective measures on health and well-being, as well as on social, behavioral and coping strategies and health-service functioning in the general population and across specific population risk groups [14, 15, 17, 18]. To date, out of 185,000 responses from 155 countries on five continents, more than 20,000 questionnaires filled in only by medical professionals have been analyzed within the COH-FIT project. All health determinants significantly worsened due to the COVID-19 pandemic, including anger, boredom, fear, focus, frustration, helplessness, resilience and social functioning. In addition, the current pandemic significantly worsened the psychosocial functioning of healthcare workers. However, the adverse effects of stress related to the pandemic were often compensated by contact with other people (often remotely), physical activity, work/hobbies, and media use.
Burnout has already been addressed by the Agency of Healthcare Research and Quality (AHRQ) in a funded MEMO (Minimizing Error, Maximizing Outcome) project, where more than 400 general practitioners and internists at 119 ambulatory care clinics conducted surveys among 1795 patients, reviewing their medical records for information on the quality of care and medical errors [19, 20]. Most common physicians’ complaints were related to a lack of time allocation for patients’ consultations. In addition, MEMO found that fully developed EHR systems and short-time consultations were associated with doctors’ stress, burnout, and will to abandon the profession. Perez et al. recently analyzed MEMO data to determine how chaos in the clinic was associated with working conditions and quality of care measures and found that chaotic clinics had higher rates of medical errors and missed opportunities to provide preventative care [20, 21].
Examples of supportive initiatives to overcome these problems include efforts already undertaken by the Rome Foundation GastroPsych group, dedicated to the science and practice of psychogastroenterology, a burgeoning field with roots in behavioral intervention science, cognitive science and experimental psychology focused on fostering professional growth and collaboration among clinicians and scientists engaged in the treatment of disorders of gut-brain interaction and other chronic digestive disorders (https://theromefoundation.org/rome-gi-psych-committee). Also, the World Gastroenterology Organization (WGO), in the ongoing Train The Trainers (TTT) program, which took place last summer (2022) in Warsaw, Poland (Figures 1, 2) has executed a new teaching module addressing resilience strategies to overcome burnout among physicians. Relevant topics discussed at TTT included: (i) staying healthy – preventing endoscopy-related injuries by focusing more on endoscopy ergonomics, (ii) leadership, (iii) communication, physician involvement and culture change at institutional levels, and (iv) wellness programs in order to promote resilience and self-care. The Train The Trainers (TTT) has been a very successful program designed to disseminate teaching skills to gastroenterologists who already underwent training programs and hold professional positions in their own countries. TTT continues to provide an excellent platform for the exchange of ideas and networking among scientists around the globe, enabling them to conduct learning and teaching as well as maintaining scientific and personal interactions.
Figure 1
The multinational participants of Train The Trainer Program of the World Gastroenterology Organization, Warsaw, 2022. The TTT program included a new module on Career Longevity addressing burnout issues among healthcare professionals. The Train The Trainer (TTT), since its inception more than 20 years ago, has been a very successful program designed to disseminate teaching skills to gastroenterologists who already underwent training programs and hold professional positions in their own countries. TTT continues to provide an excellent platform for the exchange of ideas and networking among scientists around the globe, enabling them to conduct learning and teaching as well as maintaining scientific and personal interactions

Figure 2
Warsaw 2022 Train The Trainer Program WGO Faculty. TTT program organized by WGO in collaboration with the Polish Gastroenterology Society (PTG-e) represented by Prof. Grażyna Rydzewska

Together with other groups of clinicians and scientists we developed similar activities aimed to foster cross-disciplinary collaborations and awareness towards novel technologies in the field of gastroenterology [21–23] and mental health [23, 24]. In the era of globalization and dynamic social and political changes, in our view, these collaborative efforts are very important to support individual’s self-confidence and lower the risk of burnout. Together with others in the field, we believe this article is a desperate call for maximizing the use of novel technologies, including robots in gastroenterology and cardiology care, multi-omics-based microbiome research.
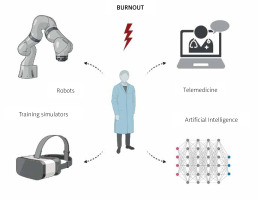
In the era of neural networks and artificial intelligence (AI), we have openly advocated for the role of telemedicine solutions in gastroenterology and cardiology [16, 25]. Some of the latest developments in these fields are highly relevant: (i) gastric examination by guided magnetic capsule endoscopy [17, 26], (ii) the CardioCube voice AI medical chatbot deploying Amazon Echo clinically validated at Cedars-Sinai Medical Center (Los Angeles, California, U.S.) and implemented in routine clinical practice, helping tele-nurses to manage patients with heart failure (H.F.) (https://fcncare.com/) [18, 27]; (iii) FDA clearance for remote at home small bowel capsule endoscopy services; and, (iv) various robotic simulators for mastering skills of gastroenterologists in training [19, 28]. With these in mind, we also need to overcome the burden associated with electronic health record (EHR) demands, which have been reported to impact doctors’ stress and emotional exhaustion, distorting their well-being and relationships. All these new technologies will be soon implemented into teaching curricula at universities to familiarize future doctors with friendly digital technologies. Also implementing various simulators (examples of available devices in GI training are listed Table I) into medical teaching might overcome the problems with real-life training, which in the era of current and future pandemics might contribute to burnout of individuals involved in teaching. Another problem, which is out of the scope of the article, though requires attention as well as solutions, is persistent overuse of digital media among healthcare professionals. This factor is also an important contributor to chronic burnout. The simplified scheme of the interplay between digital technologies and burnout are presented in Figure 3.
Table I
Examples of various simulators useful in gastroenterology training programs [28]. Implementing various simulators into medical teaching might overcome the problems with real-life training, which in the era of current and future pandemics might contribute to burnout of individuals involved in professional education
Figure 3
In the era of neural networks and artificial intelligence (AI) some of the latest developments in these fields are highly relevant. We have openly advocated for the role of telemedicine solutions, robots and mini-invasive diagnostic solutions (e.g. capsule endoscopy) as well training simulators in gastroenterology and cardiology. There is an urgent need to implement them into clinical practice to minimize physicians’ burnout, but also a great need to work on strategies aimed at minimizing digital burnout among healthcare professionals
Medical schools and professional associations need to teach new values to physicians, such as blame-free culture, acceptance of clinical uncertainty, practitioner/provider-patient dialogue, and help-seeking for mental health problems and burnout among healthcare workers. Anticipation and uncertainty have never been so palpable as we face global aftershocks in political and social life. Remarkable changes have also occurred in understanding the disease, whereby the previous paradigm of Koch’s postulates for therapeutic goals seems now more distant than ever. Examples of the new complex interfaces include many microbiome influences, genomics/omics and sequential stem cell controversies
Nevertheless, the most important is that each society must decide what type of healthcare it wants. Do we continue with understaffed hospitals, with a lack of updated technology in district hospitals and a lack of all subspecialties? It is time to decide what healthcare we want for the next 15 to 20 years. We need brave minds and solutions, thinking ‘out of the box’ to sustain and thrive in these most uncertain times. Because one is sure COVID-19 showed that the emperor’s new clothes are, in fact, naked. COH-FIT is a global consortium that is well placed to undertake systematic reviews, analyses of real-world data and meta-analyses to ensure that iterative real-time learning and support can evolve in medicine. At the policy level, the bill of Dr Lorna Breen Health Care Provider Protection Act has been submitted to the U.S. Senate. This bill has already got the green light for grants and raised calls for activities among hospitals, medical professional associations, and other healthcare entities to promote mental health and resiliency among healthcare providers. These activities will be coordinated by the Department of Health and Human Services, which will study and issue future policy recommendations for novel solutions to overcome barriers to patients’ care [25, 29].
Governments and healthcare institutions in other countries should follow these initiatives or create new ones. Burnout and stress among healthcare professionals are essential areas of research, and well-designed investigations based on global surveys are urgently needed. In addition, novel research evaluating organizational-level attempts to remedy sources of healthcare burnout and stress is urgently required [26, 30]. As the medical community, we will make all efforts to implement, teach and familiarize physicians with new technologies as well as foster global collaborations to prevent burnout and promote transition to a sustainable, fairer, more resilient and healthier healthcare systems [27, 31, 32].










