Liver transplantation has gained broad acceptance as a therapeutic modality for hepatocellular carcinoma (HCC), with better overall survival than liver resection [1].
The United Network for Organ Sharing (UNOS) adopted Milan criteria for liver transplantation in patients with HCC (single lesion, diameter ≤ 50 mm, without vascular invasion, and with no metastasis) to improve survival [2]. Yang et al. reported that the median overall survival is 5.75 years after transplantation for patients meeting UNOS criteria [1].
So, even though choosing these criteria is a focal point, there is another important topic, i.e. knowing the causes of death after selecting these criteria. However, the causes of death are unclear.
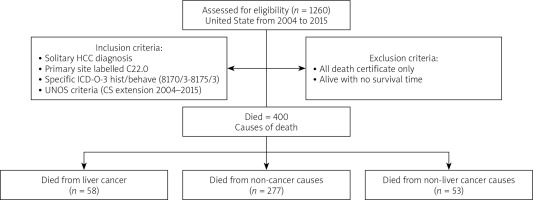
We used Surveillance, Epidemiology, and End Results (seer)*stat software, latest version 8.3.9.2 in our study to access SEER plus data, 18 registries [3, 4]. We identified the solitary HCC diagnosis with the primary site labelled C22.0, specific ICD-O-3 hist/behave (8170/3 – 8175/3) and concerning UNOS criteria (CS extension 2004–2015). We evaluated causes of death (ICD-10 identifications) and calculated the standardized mortality ratio (SMR), which represents the number of observed deaths from a specific cause to the number that would be expected to die over a given period. Therefore, understanding the distribution of different causes of death after liver transplantation among HCC patients is helpful in counselling patients regarding their care and survivorship.
We reviewed 1260 US patients with solitary HCC who had undergone liver transplants during the period 2004–2015 (Figure 1). Most patients were aged between 45 and 79 years (1204; 95.6%), were white (1002; 79.5), male (960; 76%), married (805; 63.9%), and with a localized stage (1227; 97.4%). Of the included patients 400 (31.7%) died during this period, with a mean age of death of 62.7 years. 137 patients died within the first 2 years after transplant, 105 deaths occurred within 2–5 years, and 158 deaths occurred more than 5 years after transplantation. The most common causes of death were non-cancer causes (277 (71, 4%); 3.71 (3.29–4.18)) followed by liver cancer and other cancers. Generally, liver cancer was the most common cause of death (58 patients (14.5%); SMR 33.11 (25.15–42.81)), while the most common non-cancer causes were diseases of the heart (32; SMR 1.26 (0.86–1.78)), chronic liver disease and cirrhosis (31; SMR 10.63 (7.22–15.09)), nephritis, nephrotic syndrome and nephrosis (15 (3.8%); SMR 7.80 (4.27–13.09)), and septicaemia (7 (1.8%); SMR 4.39 (1.76–9.04)). Other cancer causes of death are including lung and bronchus (15 (14.5%); SMR 1.52 (0.85–2.51)), miscellaneous cancer (9 (2.3%); SMR 3.69 (1.69–7)), non-Hodgkin lymphoma (7 (1.8%); SMR 6.65 (2.67–13.71)), and acute myeloid leukaemia (3 (0.8%); SMR 5.43 (1.12–15.88)) (Table I).
Table I
Standardised mortality ratios (SMRs) for each cause of death following liver transplant in patients with solitary HCC
Our result showed that there is a statistically significant higher risk of death due to recurrence of HCC and incidence of other cancers. This is consistent with the study by Kim et al. which reported high recurrence of HCC with poor prognosis [5]. Manzia et al. explained the incidence of de-novo cancers due to immunosuppressive drug [6]. There is a statistically significant higher risk of death due to chronic liver diseases and cirrhosis, which can be explained by a recurrence of a pre-existing disease or without evidence of recurrence (other causes like de-novo autoimmune hepatitis or biliary complications) [7]. Our result showed a statistically significant higher risk of death due to nephritis and nephrotic syndrome, and septicaemia, which is consistent with Colliou et al. [8], who reported that kidney diseases are responsible for excess deaths due to multifactorial causes (pre-transplantation, post-operative, perioperative), and the study of Lease et al., which reported that infectious complications remain a significant contributor to death after liver transplantation, which can be explained by post-transplant treatment protocols, long stay in the ICU, and pre- or post-transplant renal replacement therapy [9].
However, diseases of the heart and lungs and bronchus cancer were statistically insignificant compared with age-adjusted and demographically similar populations. We provide new insights for healthcare providers to counsel the HCC survivors post-transplant for future risks.