The lymphatic system was first described by Asellius in 1627, and chylous leak (CL) was first reported by Morton in 1691 [1, 2]. It is defined as the leakage of milk-like, triglyceride-rich lymphatic fluid from the lymphatic system in to the peritoneal cavity [3]. It can cause fever, abdominal pain, abdominal distension, and abnormal white blood cell count and a delay in the withdrawal of the abdominal drainage tube. Even more serious, improper treatment will lead to celiac infection and abdominal bleeding, which results in prolonged hospitalization and increased costs. The incidence of CL after gastrectomy with D1–2 dissection is reported as 1.99%; however, D3–4 lymphadenectomy is associated with a higher incidence of CL of up to 6.3% [4], indicating that locally advanced diseases and extensive lymph node dissection lead to a higher incidence of CL. Laparoscopic gastrectomy (LAG) with lymphadenectomy has recently been accepted as a safe and effective surgical treatment for gastric cancer [5]. There have been very few reports focused on CL after LAG [3] and D1-D2 dissection [6, 7], especially in locally advanced and semi-elective cases.
A 62-year-old male presented with complaints of nausea, vomiting, decreased appetite, and significant weight loss for 3 months. He had no history of additional disease or previous abdominal surgery. His body mass index was 18 kg/m2, and his Eastern Cooperative Oncology Group (ECOG) performance status was 1.
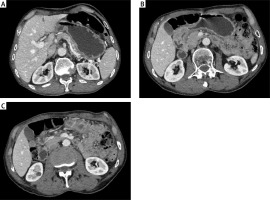
In the laboratory evaluation, haemoglobin was 12 g/dl, platelet count 272,000/ml, albumin 3.4 g/dl, total protein 6.2 g/dl, and tumour markers were normal. Upper gastrointestinal endoscopy revealed a stomach filled with solid food debris and a mass protruding from the antropyloric region of the stomach, which did not allow the passage of the scope (Figure 1). Endoscopic biopsy report of the mass showed high-grade dysplasia. Contrast-enhanced thorax, abdomen, and pelvis computer tomography showed clinical T3N+M0 gastric cancer (Figures 2 A–C). The patient was optimized for surgery and later underwent laparoscopic distal gastrectomy with D2 dissection and gastrojejunostomy with Roux-en-Y reconstruction. Intraoperatively, there were no adhesions, ascites, or omental deposits. Three 16 french, silicone drains were placed: one in the foramen of winslow, one behind the gastroenterostomy, and one in the pelvis.
Figure 2
Contrast-enhanced computed tomography. A – Dilated stomach due to gastric content; B – Distally localized, obstructive gastric cancer; C – Enlarged suprapyloric lymph node
In the macroscopic evaluation of the surgical specimen, an ulcerovejatan mass of 5 × 3.7 × 0.8 cm, which almost encircled the lumen, was observed. The histopathological examination report revealed intestinal type (Lauren classification) adenocarcinoma, grade 2, perineural and lymphovascular invasion, invasion to the subserosal adipose-connective tissue, and 4 of the harvested 32 lymph nodes were metastatic, HER-2: Positive (score 3+), with TNM staging pT3N2 (AJCC 8th edition 2020).
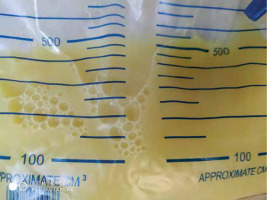
On postoperative day 3 (POD 3) the patient was given clear liquids. On POD 4 a soft diet was started. The abdominal drain outlet was serous until the POD 5. On the morning of POD 5, the drains located in the foramen of Winslow and behind the anastomosis were removed. In the evening, the colour of the pelvis drain changed to milky white (Figure 3). The patient’s regimen was then stopped. On POD 6, the triglyceride level of the drain content was found to be 210 mg/dl and a low fat-diet was arranged by the dietitian. Day by day, the daily drainage colour changed to clear. The drain tube was withdrawn and the patient was discharged on POD 15. After 2 weeks, the patient was asymptomatic, and no collection was observed in the control USG.
CL after gastric cancer surgery is an infrequent postoperative complication that has been described in reports of abdominal and retroperitoneal surgeries. The incidence of CL after gastrectomy with D1–2 dissection is reported as 1.99%; however, D3-4 lymphadenectomy is associated with a higher incidence of CL of up to 6.3% [4]. Clinical data concerning the complications of laparoscopic gastrectomy, especially for the CL, remain scarce because the majority of reports on this topic focus on comparing the effectiveness and advantages of this procedure with open surgery.
There are some suggestions for potential types of lymphatic injury that may cause chylous leak [8]. First, lymph node metastasis leads to flow obstruction and increases the pressure within the lymph duct stump, which does not completely close with vessel closing and cutting devices. Second, the No. 8 or No. 9 lymph nodes are among the most densely clustered areas of the lymphatic trunk and its major tributaries. It is conceivable that removing these lymph nodes during laparoscopy causes a tear in the lymphatic channels. Third, poor nutritional status, which is commonly seen in gastric cancer patients, may prevent self-healing closure of lymphatic channels by solidified lymphatic fluid or wound inflammation. Fourth, As the number of resected lymph nodes increases, the probability of CL development may increase. To prevent this complication, during the operation, if we determine large lymph nodes around the celiac artery, major lymphatics should be controlled by using clips. At the end of the LN dissection, the surgeon should carefully determine if a coarse nonvascular tissue cord stump is present in the dissection area.
First-line treatment of CL usually includes cessation of oral feeding plus TPN [9]. Another treatment modality is the implementation of a diet solely with MCTs (medium chain fatty acids, with 6–12 carbon). MCTs might decrease lymphatic flow and provide regular nutrition because it is directly transported to intestinal cells [3]. Cárdenas et al. recommended a diet with MCTs as the first-line medical care [1]. Some authors have presented somatostatin or octreotide administration as an effective treatment [10]. In patients for whom conservative treatment remains ineffective, surgical intervention is advised [11].
In conclusion, the presented case confirms that CL can lead to prolonged drain maintenance and prolonged hospitalization time. Locally advanced disease, extensive lymph node dissection, high positive lymph node ratio, and malnutrition may increase the risk. Conservative treatment is a curative option in most cases.