Introduction
Lung cancer is the second most common cancer diagnosis in men and women (after prostate and breast cancer, respectively), accounting for millions of annual diagnoses and deaths. With increased access to tobacco and industrialization in developing countries, the incidence of lung cancer is increasing worldwide. The average age of diagnosis is 70 years. Men are twice as likely to be diagnosed with lung cancer, largely reflecting differences in tobacco consumption, although women may be more susceptible due to higher rates of epidermal growth factor receptor mutations and estrogen activity [1].
Lung cancer most often originates from epithelial cells. There are four basic histological types: squamous cell carcinoma, small-cell carcinoma, adenocarcinoma, and large-cell carcinoma [2].
According to data from the National Health Fund (NHF), the number of patients treated for lung cancer in Poland was steadily increasing over the five-year period (2015-2020). Taking into account the diagnosis (diagnosis of new cases) and the criterion of survival with a diagnose, approximately 10% of new patients are added each year. The NHF data concerns all patients with lung cancer, regardless of the stage of advancement and type of cancer. Lung cancer is one of the biggest challenges in terms of malignant neoplasms in Poland. Similar trends apply to Europe and the rest of the world where such statistics are kept. A large number of late diagnosed cases and unfavorable prognosis generate economic consequences, which is a serious burden on the health care system of many countries [3,4].
Despite progress in oncology (generations of drugs, gene therapy, imaging diagnostics, mass prevention possibilities), the treatment of lung cancer is not effective enough to achieve long-term survival rates. The prognosis is particularly poor for patients diagnosed with small cell carcinoma, with survival time up to 2 years and very rare complete cure. More favorable cure statistics are achieved in patients with non-small cell lung cancer [5,6].
Oncology is a dynamically developing field of medicine, new methods of treatment, innovative drugs and methods of their application, as well as new organizational solutions are being introduced. During hospital treatment, non-therapeutic procedures supporting treatment are important: psychological care, rehabilitation, and nursing care. Oncological patients are sensitive due to reduced immunity (the principle of asepsis during all invasive procedures, e.g. catheterization, intravenous and intramuscular injections) [7-9].
Aim of the work
The aim of the study was a two-year observation of the population of patients treated in the oncology ward, taking into account admission mode, discharge mode, medical procedures, treatment methods used, imaging diagnostics, and nursing care.
Material and methods
A pooled analysis of patients treated in the ward of clinical oncology and radiotherapy of a specialist hospital in the Mazovian Province was used. Our analysis is descriptive due to the retrospective nature of the quantitative data collected in databases, without the possibility of entering and describing clinical data, as described in the Limitations section of the paper.
The analysis included the ward’s statistical data from 2020-2021:
total number of hospitalizations during the observation period,
commencement of hospitalization by each patient (year, month, day),
completion of hospitalization by each patient (year, month, day),
gender of patients included in the analysis,
age of the patient at the commencement of hospitalization,
principal diagnosis,
co-occurring diagnoses,
mode of patient admission,
mode of patient discharge,
medical procedures performed, correlations between age and gender of patients in the study population.
Study inclusion criteria:
patients who started treatment in the oncology ward in the period 1 January 2020-31 December 2021,
disease codes according to the International Statistical Classification of Diseases vol. 10 (ICD-10) were taken into account – mainly with the C34 code (lung cancers) taking into account the location.
The presence of other disease codes in the patient’s ICD-10 diagnosis regarding co-occurring chronic diseases did not disqualify patients from the study population [10].
In October 2022, a consent of the Director of the medical facility (hospital) was obtained for access to the medical records of the ward. The analysis was carried out in the patient population of the Ward of Clinical Oncology and Radiotherapy. The ward conducts chemotherapy and immunotherapy for breast, lung, gastrointestinal cancers, including the esophagus, stomach, colon, pancreas, genitourinary system cancers (kidney, prostate, bladder, testicular cancers), head and neck cancers, reproductive organ cancers, and hematological cancers (leukemia, lymphoma, myeloma). Care is also provided to patients referred from higher reference centers for continuation of chemotherapy and patients with complications of oncological treatment or requiring palliative care [11].
Statistical analysis
The database was prepared in Microsoft Excel using MS Office 2016 for Windows 10. Descriptive statistics were used to characterize variables. The following measures were calculated for variables: mean (M) and standard deviation (SD), median (Med.), minimum value (Min), maximum value (Max), chi-square test.
In the comparative characteristics, the one-way analysis of variance (ANOVA) test was used. Simple linear regression analysis (Pearson) was used to detect and describe the strength and direction of the correlation between the length of stay and age. Qualitative variables (age, gender) were presented as quantitative values (n) and percentages of the entire group (%). In the comparative characteristics of age, the Student’s t test was used. Statistica 15 software (Stat Soft Inc., Tulsa, OK) was used for statistical analysis. The level of significance was assumed to be p<0.05.
Results
Patients included in the study constituted 13.68% of the entire population treated in the ward, 14.7% in 2020 and 12.2% in 2021, respectively. Detailed results of the group included in the study are presented in Tables 1 and 2.
Table 1
Characteristics of the group of patients included in the study with regard to gender
| Year | Women | % | Men | % | Total |
|---|---|---|---|---|---|
| 2020 | 80 | 28.5 | 201 | 71.5 | 281 |
| 2021 | 64 | 34.0 | 124 | 66.0 | 188 |
Table 2
Characteristics of the group of patients included in the study with respect to age
| Age | Mean | Min | Max | SD |
|---|---|---|---|---|
| Women | 64 | 45 | 82 | 10.1 |
| Men | 65 | 45 | 83 | 13 |
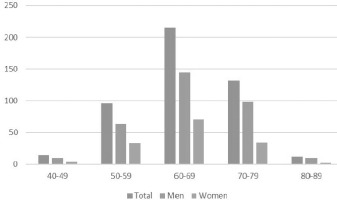
Lung cancer was more common among men. Age of the patients treated in the ward was recorded for the date of hospital admission. The minimum age for both women and men was 45 years (1 man and 1 woman). Details of the age profile of patients are presented in Figure 1.
In the analyzed population in 2020-2021, the largest group of patients were admitted based on the oncological diagnostics and treatment (DILO) card, as part of the Oncology Fast Track. The therapy is dedicated to patients in whom doctors suspect or confirm malignant tumors, regardless of the patient’s age (without age restrictions). Diagnostics and treatment as part of the oncological package are not covered by the NHF limits. Table 3 and Figure 2 present a statistical analysis of patients divided according to the mode of admission for hospital treatment. It was shown that factors such as the age of admission (p<0.001), length of stay in the ward (p<0.001), number of procedures performed (p<0.001) and frequency of referral of the patient for further treatment (p=0.002) depended on the mode of admission.
Table 3
Comparative analysis of patients by admission mode
Figure 2
Median length of stay depending on the variable: admission mode
Notes: DILO – oncological diagnostics and treatment, EMT – emergency medical team.
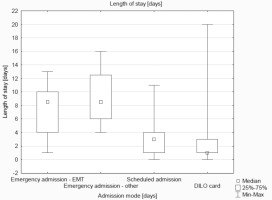
The median value in Figure 3 for the patient’s length of stay differs depending on the admission mode, with the highest values for patients admitted in an emergency mode and those admitted in the EMT mode, and lower values for patients admitted in a planned mode and based on a DILO card (p<0.001).
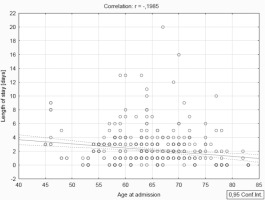
The correlation (R=-0.1985) visible in Figure 3 showed the highest concentration for pairs of variables in the range of 55-75 years and 2-4 days of stay. It was shown that a patient’s age had a statistically significant effect on the length of stay in the ward, i.e. older patients were hospitalized for a shorter time. Patients in the study group were admitted with the main diagnosis Z51.1 – a cycle of cancer chemotherapy, and a coexisting diagnosis from the C34 group. The location of the tumor and the number of sick people in the study group are presented in Figure 4.
Figure 4
Tumor location in the studied group of patients Notes: C34.1 – upper lobe, bronchus or lung, C34.2 – middle lobe, bronchus or lung, C34.3 – lower lobe, bronchus or lung, C34.8 – overlapping lesion of bronchus and lung, C34.9 – bronchus or lung, unspecified.
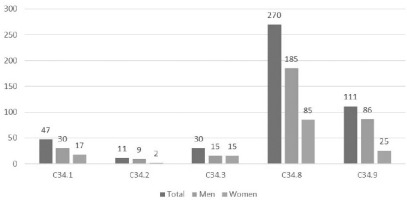
In the observed group, generalized lung cancer exceeding one location predominates, which may be related to late diagnosis, treatment implementation and significant disease progression.
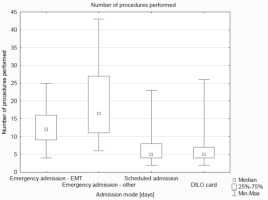
The analysis of subsequent variables showed that the median value of the number of procedures performed was the highest in the group of patients admitted in an emergency mode and in the EMT admission mode, and the lowest in the group of planned admissions and based on DILO cards (Figure 5).
Discussion
Approximately 70% of cancers are caused by harmful environmental factors and bad habits. Therefore, shaping proper pro-health behaviors is important from the youngest age. The risk of developing cancer is proportional to the length of exposure to harmful factors. In the case of cancer, prevention is particularly significant. Avoiding contact with carcinogens, preventive examinations, self-observation (self-observation, observation of skin lesions, control of unplanned weight loss) are of great importance in oncology. The activities will increase the chance of detecting a small, easier to treat lesion. Modern medicine is still not very effective for most developed cancers [12].
Oncological prophylaxis provides great protection against the effects of a developed disease. Despite the growing awareness among Poles, screening tests for cancer detection are still too little popular. The relations of early cancer therapy between Poland and Western European countries are unfavorable, only 20% of cancer patients in Poland are diagnosed early, while in other developed countries (e.g. the USA and wealthier countries of the European Union, the early diagnosis rate reaches 70%. The World Health Organization estimates for Poland that by 2040 the number of cancer cases will double and 20% of diagnoses will end in death due to cancer [13].
Effective public awareness of the significance of oncological prevention can translate into greater awareness of control tests and early detection of changes. Oncological prevention as an effective weapon against the development of neoplastic diseases may be the main goal of medical activities of the future. In every developed country it should be an important goal of healthcare to improve the effectiveness of secondary prevention, including activities aimed at increasing the effectiveness of screening tests for cancers that have the highest share of diseases in the general population of Poland and Europe, involving primary care physicians and occupational medicine in preventive activities. Apart from systemic solutions (financial outlays, programs), educating patients and their families by nurses in outpatient (pre-hospital) care on avoiding risk factors and self-observation, regular taking of medications is of great importance. The data obtained in our own study indicates a significant contribution of the family doctor institution in the diagnosis and referral of patients to a specialist ward [14-16].
There were no pregnant women in the observation population, mainly due to the age of patients admitted for treatment, and the obtained data did not include information on cigarette smoking.
Some of the patients treated in the hospital in our own study were admitted to the ward as a result of transfer by the Emergency Medical Services. In the authors’ opinion, it may mean that the people had been previously diagnosed with a diagnosed tumor, and the intervention and subsequent transport were related to the intensification of symptoms in the course of the neoplastic process. The analysis dated back to 2022 of the Emergency Medical Services interventions for oncological patients presents data according to which approximately 65% of patients go to the Hospital Emergency Ward, some of them need implementation of pain medication, and some of them need pharmacology related to symptoms (shortness of breath, vomiting). In the analysis, the common diagnosis was the code C34 – tumor in the lungs [17].
Patients treated in the oncology ward undergo specialist therapeutic and diagnostic procedures. Nursing procedures described in more detail in the 2022 paper [18] and foreign reports [19,20] constitute an important part of stay in the ward. The authors list the following as the main problems in the scope of nursing care for a patient diagnosed with cancer: chest pain, resting dyspnea, cough, hemoptysis, problems with expectoration of secretions, excessive sweating, elevated body temperature. The tasks of the nursing staff are aimed at minimizing the ailments resulting from the disease.
Lung cancer, as was the main focus of our observations, is a common cause of disease in the group of oncological diseases and remains the most common malignant tumor in Poland, with a tendency for late detection and unfavorable prognosis for the patient. Data confirming the tendency can be found in other medical centers in Poland [21,22].
Limitations
Our observations have 3 main limitations:
In the analysis, a complementary research technique in the form of interviewing patients was not possible because the analysis is retrospective. All patients had completed hospital treatment before obtaining consent for the study, access and analysis of data.
Lack of access to information on whether patients treated for lung cancer in the oncology ward had smoked cigarettes before. Nicotine addiction as a significant risk factor for lung cancer has been confirmed as a key risk factor in many studies, but the epidemiological data obtained from the ward did not include patients’ medical history, previous history, lifestyle and use of stimulants. The database included only the period and information directly related to treatment in the oncology ward [23,24].
The analysis did not include the TNM (tumor, nodules, metastases) classification, which, according to many available scientific data and the recommendations of the European Society for Medical Oncology, may correlate better with the advancement of the neoplastic disease than the ICD-10 classification. In the databases made available to the authors, there was no data classifying patients according to TNM [25-27].
Conclusions
The most common location of lung cancer in the study group was C34.8 (overlapping lesion of bronchus and lung), which indicates late diagnosis. Emergency admission by transferring the patient by the emergency medical team was associated with a longer hospital stay and a greater number of medical procedures performed, which is associated with a previously unplanned medical intervention as a result of sudden symptoms in a patient without a specific previous diagnosis. The patient’s age is not a prognostic factor in terms of the mode of admission to the ward. Admission of the patient to the ward based on the DILO card is the most effective mode in both clinical and economic terms. The procedures performed are selected in a targeted manner and may condition a shorter stay of the patient in the ward.