Gastrointestinal stromal tumours (GISTs) are the most common mesenchymal tumours of the gastrointestinal tract. They arise most commonly in the stomach (60–70%) and small intestine (20–25%), while other sites of origin are rare [1, 2]. In many cases, they are diagnosed accidentally due to their indolent clinical course; however, 10–30% of these have malignant potential [2–4]. Symptoms depend mostly on tumour localization and size. Around 70% of tumours present with abdominal pain, and 20–50% present with gastrointestinal bleeding, which is predominantly intraluminal, and rarely an exophytic type of GIST may rupture and bleed into the peritoneal cavity [3, 4]. GIST of the small bowel can lead to intestinal obstruction, while oesophageal GIST causes dysphagia. Gastric and oesophageal GISTs carry a better prognosis than small bowel GISTs of similar size and mitotic rate [4]. Tyrosine kinase inhibitors (imatinib or sunitinib) are the main chemotherapeutic options in unresectable, metastatic, or recurrent GISTs.
A 41-year-old man with no significant comorbidities presented to the emergency department with syncope and diffuse abdominal pain of 24-hour duration. No abdominal trauma was reported by the patient. The patient reported bloating and intermittent abdominal pain without nausea for the last 2 weeks. On physical examination upon admission, his vital signs showed tachycardia of 112 beats/min and hypotension of 90/60 mm Hg. An abdominal examination revealed periumbilical tenderness and abdominal distension. Laboratory tests revealed low haemoglobin (8.7 g/dl) and no other unusual findings. Computed tomography (CT) scan was performed to rule out intraabdominal haemorrhage, and it revealed a large expansive mass in the upper abdomen attached to the greater curvature of the stomach and left liver lobe and extending inferiorly to the level of the umbilicus.
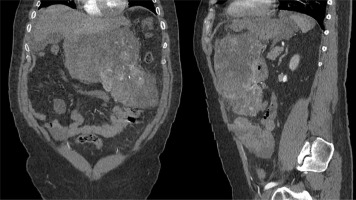
It had axial dimensions of 21 × 8.3 cm and contained hyperdense areas that suggested active bleeding. There was dense free fluid in the perisplenic and perihepatic area. Haemoperitoneum was suspected, and urgent exploratory laparotomy was performed (Figures 1, 2).
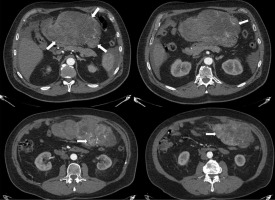
Figure 1
Axial CT images showing hypervascularised exophytic tumour originating from the gastric body, with haemorrhagic areas within the tumour (white arrow)
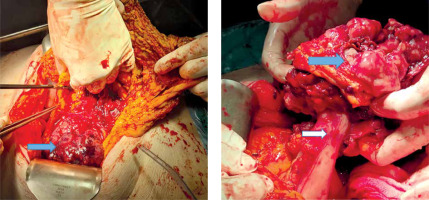
Intraoperatively, 2000 ml of intraperitoneal blood was found originating from a large exophytic necrotic tumour that arose from the front wall of the stomach body. The haematoma was evacuated, and a partial wedge stomach resection with the tumour using the stapling device was performed. Macroscopically, no other tumours or metastases were detected. The patient received 6 doses of packed red cells in the perioperative period (Figure 3).
Figure 3
Intraoperative photo showing hypervascularised exophytic tumour (blue arrow) originating from the gastric body (white arrow)
The postoperative course was uneventful, and the patient was discharged on the 11th postoperative day. Pathohistological exam confirmed ruptured stomach GIST (T4, N0, M0) with a mitotic index of more than 5 per high-power field, which indicated high progression risk. Imatinib mesylate therapy was initiated, and after one year of follow-up there is no sign of disease recurrence.
In most cases GISTs present as a slow-growing tumour with slowly progressive symptoms. Complete surgical resection is the mainstay treatment, and the prognosis is primarily dictated by tumour aggressiveness, size, and mitotic index [5]. The development of imatinib mesylate has significantly improved the prognosis for advanced stages [1, 5, 6]. Surgical urgencies related to GIST include gastrointestinal obstruction, perforation, and tumour-related haemorrhage. Haemorrhage is predominantly intraluminal and rarely leads to hypovolaemic shock. Intraperitoneal bleeding is rare, and there are few reports in the literature [6–9]. Such bleeding is life-threatening because symptoms may be mild and nonspecific until serious blood loss develops when signs of haemorrhagic shock become apparent. Our case describes a rare clinical scenario in which an exophytic giant tumour led to a rupture and serious intraperitoneal haemorrhage. The diagnosis was established intraoperatively, and despite the emergent procedure, radical (R0) resection was achieved with uneventful postoperative recovery. In such cases, it is important to perform abundant peritoneal lavage to remove all tumour tissue and completely evacuate the haematoma in order to prevent tumour spillage and dissemination. Differential diagnoses of ruptured GISTs may include liver haemangioma, splenic rupture, splenic pseudoaneurysm rupture, aortal aneurism rupture, or ruptured tubal pregnancy [2, 8, 10]. In all these cases, a quick diagnosis of intraperitoneal bleeding and recognition of haemorrhagic shock is mandatory to proceed with adequate management.
Extraluminally growing tumours should be considered when patients present with acute nontraumatic haemorrhagic shock or haemoperitoneum.