Introduction
Gallstone disease (GSD) is a common gastroenteric disorder, occurring in 10–15% of the adult population [1]. An increase in its incidence is characterized by a higher frequency of development of a complicated form (up to 35%) [2, 3]. Due to its relatively high complication and mortality rate, surgical treatment of GSD complicated by obstructive jaundice (OJ) is a pressing issue nowadays [4–6].
Despite a significant improvement in treatment outcomes, the mortality rate for complex GSD forms after emergency surgery remains several times higher than for elective surgical interventions. For instance, various statistical data report that the postoperative mortality of patients with complicated GSD ranges between 6.2% and 13.6%. Hence, the intensity of OJ defines the frequency of hepatic function impairment [7]. On the other hand, the OJ intensity depends on the level of biliary hypertension.
At present, the development of abdominal surgery is characterized by the widespread introduction of new, highly informative methods of diagnosis and minimally invasive surgical procedures into clinical practice. They can reduce surgical risk and expand treatment options for patients. Also, these methods have taken the lead in treating numerous patients with complications, universally replacing traditional methods [8, 9]. However, much of the scientific literature is devoted to the use of new technologies in managing simple GSD forms [10].
Dissatisfaction with treatment outcomes in GSD patients with OJ and purulent cholangitis specifies complex treatment using endovideosurgical technology, as well as endoscopic and endobilliary procedures [11].
Recent publications point to approaches that are opposed to surgical solutions to this issue. Thus, some authors prefer retrograde endoscopic transpapillary interventions to dissection of the duodenal papilla with endoscopic papillosphincterotomy (EPST), lithotripsy, endoprosthesis, nasobiliary rhenium plating, followed by cholecystectomy [12, 13]. Other authors suggest a method in which common bile duct (CBD) surgery and cholecystectomy are carried out with less traumatic access such as laparoscopy or mini-laparotomy [14]. Laparoscopic cholecystectomy (LC) has become the benchmark for treating cholelithiasis, with promising results [15]. The disadvantage of laparoscopy in choledocholithiasis treatment is the complexity of manipulations on the CBD and prolonged stressed carboxyperitoneum, which significantly increases the risk of surgery outcome in patients with cardiopulmonary pathology. Moreover, this technology is quite costly, which prevents the spread of the method [16].
While new diagnostic and surgical techniques develop rapidly, they are often used randomly and yield inconsistent results [17, 18]. Therefore, the variety of treatment options available for complicated GSD forms and the ambiguous attitude toward them complicate the correct tactical decision in each case. The high mortality rate and unsatisfactory surgical treatment outcomes of patients with GSD complicated by OJ defined this study’s primary aim and objectives.
Aim
Thus, this work aims to optimize the surgical treatment of GSD patients with accompanying OJ by introducing a differentiated approach to the choice of surgical intervention tactics. The authors suggest that applying minimally invasive surgery together with the developed tactics of treating GSD patients with accompanying OJ will greatly facilitate the choice of appropriate surgical intervention.
The following tasks were set to achieve this aim:
Developing optimal treatment tactics with minimally invasive surgical techniques for patients with GSD accompanied by OJ.
Examining the clinical effectiveness of a differentiated approach to surgical treatment of GSD accompanied by OJ.
Carrying out a comparative analysis on the outcomes of minimally invasive and conventional surgical techniques in GSD patients with accompanying OJ based on evaluation of lipid peroxidation and antioxidant protection (LPO-AOP) system parameters and compensatory reserve of the organism.
Material and methods
Sampling
The study examines the treatment results of 384 GSD patients with OJ, who underwent surgical treatment in the hospital surgery clinic of Marat Ospanov West-Kazachstan State Medical University between 2016 and 2020. The examined patients were divided into 2 groups (experimental and control). Each group was divided into 3 subgroups as per the severity of OJ according to Fedorov-Vishnevsky’s classification (2000).
The experimental group (group A) consisted of 220 (57.3%) patients. The first subgroup (A1) included 79 (35.9%) patients with a mild jaundice severity degree, the second subgroup (A2) consisted of 104 (47.3%) patients with a moderate jaundice severity, and the third subgroup (A3) comprised 37 (16.8%) patients with severe obstructive jaundice.
The control group (group B) consisted of 164 (42.7%) patients. Here, the first subgroup (B1) included 56 patients with mild-severity jaundice (34.2%), the second subgroup (B2) comprised 76 patients with moderate-severity jaundice (46.3%), and the third (B3) subgroup involved 32 (19.5%) patients with severe obstructive jaundice.
Patients in the experimental and control groups were comparable in terms of clinical and demographic parameters (Table I).
Table I
Clinical and demographic characteristics of patients in the experimental and control groups
The mean age of the patients was 55 (range: 48 to 66) years in the experimental group and 53 (range: 44 to 64) years in the control group (p > 0.05). As for gender composition, both groups were dominated by female patients: 129 (58.6%) patients in the experimental group and 106 (64.6%) patients in the control group were female.
Study design
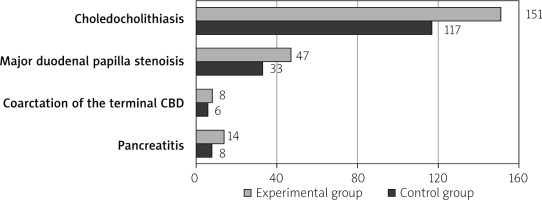
The distribution of patients with OJ was as follows. Choledocholithiasis was noted in 151 (68.6%) patients of the experimental group and 117 (71.3%) of the control group (p = 0.568). Major duodenal papilla stenosis was recorded in 47 (21.3%) patients of the experimental group and 33 (20.1%) patients in the control group (p = 0.767). Coarctation of the terminal CBD was detected in 8 (3.7%) patients of the experimental group and 6 (3.6%) patients of the control group (p = 0.991). Pancreatitis occurred in 14 (6.4%) and 8 (4.8%) patients of the experimental and control groups, respectively (p = 0.536) (Table I, Figure 1).
In the experimental group, 66 (30%) patients suffered from jaundice for up to 7 days, 116 (52.7%) patients for 7 to 14 days, and 38 (17.3%) patients for more than 14 days. In the control groups, the distribution was as follows: 48 (29.3%) patients experienced jaundice for up to 7 days, 80 (48.8%) patients became affect by jaundice 7 to 14 days before investigation, and 36 (21.9%) patients suffered from this condition for more than 14 days. A total of 77 (35%) patients in the experimental group and 62 (37.8%) patients in the control group were diagnosed with acute cholecystitis, while 143 (65%) and 102 (62.2%) patients experienced chronic cholecystitis, respectively.
Ethical statement
A written agreement was signed with all patients, assuring anonymity and confidentiality of the information received. The study was conducted in accordance with international norms of ethics and morality approved at the meeting of the Ethics Committee of Marat Ospanov West-Kazakhstan State Medical University (Minutes No. 339).
Methods
Based on the surgical treatment options, GSD patients with accompanying OJ were divided as follows. A total of 220 patients in the experimental group underwent minimally invasive interventions. Of them, 79 (A1) underwent single-step ablative surgery (A1): LC and EPST in 21 patients; LC and EPST with endoscopic mechanical lithoextraction of concrements in 24 patients, LC and laparoscopic choledocholithotomy (LCL) with drainage of the CBD in 20 patients, and LC with drainage of the CBD as per Holsted-Pikovsky method in 14 patients. Another 104 patients (A2) experienced a two-step surgical correction with endoscopic sanitation of the choledochus at the first stage and LC at the second stage. The same tactics were used in 37 patients of the A3 subgroup. The first stage included minimal surgical intervention aimed at elimination of jaundice nasobiliary drainage (8), stenting (24), and percutaneous transhepatic biliary drainage (5). The second stage used EPST to eliminate stenosis and coarctation (8). The removal of concrements from CBD with cholecystectomy was performed in 29 patients.
Patients with an acute process with marked infiltration and adhesions in the liver gate area when performing LC require conversion. The operation is completed with the mini-laparotomy access using the “MiniAssistant” set of instruments (League-7, the Russian Federation).
The control group included 164 patients with contraindications for laparoscopic and endoscopic surgeries. Patients in the control group underwent surgical interventions using the conventional method in one stage in subgroups B1 and B2, and two stages in subgroup B3. Conventional cholecystectomy, choledocholithotomy, and transduodenal papillosphincterotomy were done. The operation was terminated using different external (according to Holsted-Pikovsky, Vishnevsky, Ker) and internal (choledochodenoanastomosis) methods of biliary tract drainage.
All participants in the experimental and control groups were examined in a similar manner. General clinical methods included collecting and evaluating patient complaints, history of illness and life, objective patient status, and laboratory and instrumental methods. These included abdominal ultrasound, chest and abdominal cavity X-ray, duodenoscopic oesophagus, computed tomography (CT) and abdominal cavity organ magnetic resonance imaging (MRI), endoscopic retrograde cholangiopancreatography.
Given the presence of jaundice and the threat of liver disease progression, all patients were assigned to minimally invasive surgery. In this study, the choice of surgical procedures and their sequencing was tied to the severity of OJ.
Ablative treatment methods like simultaneous laparoscopic cholecystectomy with choledocholithotomy and external drainage of the CBD were used in patients with GSD complicated by mild-degree jaundice, except for those in whom jaundice development was caused by stenosis or concrement entrapment in the large duodenal papilla of the duodenum. In this case, LC and EPST with choledocholithoextraction were performed simultaneously.
A two-step approach was used with patients having moderate and severe jaundice. At the first stage, endoscopic and endobiliary interventions (EPST, choledocholithoextraction) were applied, followed by an LC after 5–7 days at the second stage.
In the presence of severe OJ, drainage operations were performed using minimally invasive interventions (percutaneous transhepatic biliary drainage, stenting or nasobiliary drainage, cholecystostomy). Patients underwent sanitation of extrahepatic bile ducts by endobilliary interventions and LCs were performed in one stage 21–28 days after the bile duct decompression. This operation took place after the resolution of fermentemia and cholestasis, the restoration of the liver’s protein-synthetic function, and after the relief of the hepatorenal syndrome.
A comparative analysis of clinical and laboratory changes in the studied groups was performed to estimate the surgical treatment results of GSD complicated by OJ. The functional state of the liver, LPO-AOP systems, and compensatory reserve of the organism were evaluated. The incidence of postoperative complications, mortality, and length of hospital stay were considered comparative criteria of treatment efficacy in both clinical groups.
Statistical analysis
Data analysis and predictive modelling were performed using R 3.6.3 statistical computing environment (R Foundation for Statistical Computing, Vienna, Austria) with additional third-party packages: lme4 1.1-21, lmer Test 3.1-1, emmeans 1.4.8, car 3.0-7, and MuMIn 1.43. A linear regression model with log2 transformation of the dependent variable and a gamma regression model (with a reverse relationship function) was used. All generalized linear models included correction covariates: patient’s age and gender, and the duration of jaundice. Nagelkerke’s pseudo-R2 was used as a quality metric for the generalized linear models. Regression analysis is suitable for creating predictive models for hard-to-measure indicators. This analysis may also be applicable to living individuals.
Linear mixed-effect models were used to evaluate the effect of surgery on laboratory index dynamics. A unique patient index was included in the model as a random effect. The independent variables in the model were incorporated after the log2 transformation. In addition to the above variables, the corresponding laboratory index log2-transformable before surgery was used as the correction covariate. The quality of the model was assessed employing the marginal coefficient of determination (R2).
Results
Cholestasis and cytolysis parameters on admission in both groups exceeded the reference value several fold, depending on the OJ severity. Thus, the average bilirubin level on admission exceeded the reference values by 2–3-fold in subgroups with a mild degree of OJ, 7–8-fold, and more than 15 fold in subgroups with moderate and severe degrees (Table II).
Table II
Bilirubin levels in patients of the control and experimental groups
Statistical processing of the obtained data in the linear mixed-effects regression model (Table III) revealed differences between the groups in terms of the average total bilirubin concentration irrespective of its pre-operative level, the severity of OJ, patient’s age and gender, as well as the duration of jaundice and the nature of the inflammatory process (p < 0.0001). The surgery effect depended on the severity of OJ (p < 0.0001): the most significant differences between the groups were observed in case of severe OJ course during the first 5 days after the operation.
Table III
Results of deviance analysis for total and direct bilirubin, ALT, AST, and GGT blood levels according to a linear mixed-effects regression model
Reduction of the total bilirubin level in dynamics was statistically significant in comparison groups of corresponding subgroups. Thus, in a linear regression model with mixed effects, the level of total bilirubin was 1.4-fold lower in the experimental group compared with the control in patients with a mild degree of OJ severity on day 5 (0.74 (95% CI: 0.70; 0.79); p < 0.0001), and in the subgroup with a moderate degree – on day 7 (0.74 (95% CI: 0.70; 0.780; p < 0.0001). Following 14 days of postoperative intervention, bilirubin levels were 1.9-fold lower in the subgroup with severe OJ than in the control group (0.52 (95% CI: 0.42; 0.64); p < 0.0001).
A similar picture was found concerning the average level of direct bilirubin. Thus, a clearly positive dynamic of bilirubin level in the experimental group of patients was found. Significant reduction in bilirubin indicator mainly due to direct fraction indicates adequate restoration of liver pigment function.
On admission, the 2 groups of patients demonstrated elevated concentrations of AST, ALT (cytolysis markers), and GGT (cholestasis markers) (Table IV).
Table IV
Levels of AST, ALT, and GGT in the control and experimental groups
The biochemical blood analysis indicated significant abnormalities in the functional activity of the liver in patients with different OJ severity.
A linear regression model with mixed effects revealed statistically significant differences between the groups concerning the mean serum ALT level regardless of its pre-operative level of OJ severity, as well as corrective covariates (p < 0.0001). The effect of surgical intervention depended on the severity degree (p < 0.02): the most significant differences between the groups were observed for severe OJ courses (Table II). The same picture was observed for the mean serum AST level (Table II). Thus, in the postoperative period, ALT and AST levels in the experimental group were on the average 1.2 fold-lower (p < 0.0001) compared to the subgroup with a mild degree of OJ, 1.1-fold lower (p < 0.0007, p < 0.0002, respectively) in the subgroup with moderate OJ, and 1.3-fold (p = 0.0013) and 1.5-fold (p = 0.0267) in the subgroup with severe OJ, respectively.
Statistically significant (Table V) but less pronounced differences between the groups were found for the mean serum GGT level regardless of its pre-operative level and the values of other covariates (p < 0.0001). The effect of surgical intervention weakly depended on the severity of OJ (p = 0.04). Thus, the GGT level in patients in the experimental group was significantly lower at all follow-up periods. Compared to controls, it was on average 1.5-fold lower (0.66 (95% CI: 0.62; 0.71) p < 0.0001) in the subgroup with a mild degree of OJ severity, 1.4-fold lower (0.73 (95% CI: 0.70; 0.77) p < 0.0001) with moderate, and 1.3-fold lower (0.77 (95% CI: 0.62; 0.96) p = 0.0193) with severe OJ.
Table V
Analysis results of MDA and catalase deviation in the linear mixed-effects regression model
The OJ is accompanied by a significant increase of primary and secondary lipid peroxidation products in blood, which is one of the objective criteria of disturbed liver function. Therefore, we investigated the parameters of LPO-AOP systems in the main and control groups.
A significant deviation in plasma LPO products with toxic properties aggravating the pathological process was diagnosed on admission (Table VI).
Table VI
Levels of malonic aldehyde (nmol/ml) and catalase activity (µCat/l) in patients from the experimental and control groups
As for the AOP indicators, there was a decrease in activity in all the groups at admission (Table VI).
A linear mixed-effects regression model revealed differences between the groups concerning MDA level regardless of its pre-operative level and OJ severity (Table III), as well as other covariates (p < 0.0001). The most pronounced differences between the groups were observed for the severe OJ course on the first day after surgery.
The resulting marginal estimates of mean MDA levels reflected a downward trend in this index in the postoperative period in both groups. However, mean MDA levels in patients in the experimental group were on average 1.2-fold lower in the subgroups with mild (0.85 (95% CI: 0.80; 0.90); p ≤ 0.0001) and moderate (0.86 (95% CI: 0.81; 0.91); p ≤ 0.0001) degrees of OJ severity and 1.4-fold lower (0.74 (95% CI: 0.60; 0.91); p = 0.0051) in the group with severe OJ compared with controls, indicating a shorter time of indicator normalization in the respective group (Table V).
The differences were also established between the groups in terms of catalase level regardless of its pre-operative level and the OJ severity, as well as corrective covariates (p < 0.0001). The effect of the operative intervention depended on the degree of OJ severity (p < 0.0001). The most pronounced differences between the groups were observed for a severe OJ course on the first day after the surgery. The most negligible differences were registered at a medium degree of OJ severity.
The increase in catalase activity after surgery in the comparison groups reflects marginal mean level estimates of this index. However, the rate of increase in the experimental group was higher, which is confirmed by significant differences between the subgroups with mild (p = 0.0003) and severe (p ≤ 0.0001) degrees of OJ severity over the entire follow-up period. The differences were more pronounced in patients with severe OJ, with catalase being 1.3-fold (1.27 (95% CI: 1.15; 1.410; p ≤ 0.0001) higher in the experimental group than in controls.
Thus, minimally invasive surgical treatment of GSD, complicated with OJ, has a more significant corrective effect on the LPO-AOP system parameters manifested in a higher rate of LPO inhibition and increased activity of AOP enzymes than during conventional (open) surgical interventions.
The influence of minimally invasive and traditional surgical interventions on the compensatory reserve of an organism in patients with GSD complicated by OJ was examined to determine the body’s reaction to the operative trauma. The stress index (SI from 80 to 150 conventional units as a reference value) is a highly sensitive test testifying to activation of vegetative homeostasis and allowing for compensatory reserve estimation.
A linear mixed-effects regression model revealed differences between the groups in terms of the stress index regardless of its level before surgery, the OJ severity (Table VII), and other covariates (p < 0.0001).
Table VII
Analysis results of deviations in SI and cortisol level in a linear mixed-effects regression model
As can be seen from the Table, the postoperative stress index in the studied groups reflects the decrease of the SI values in the experimental group and its increase in the control group (Figure 2).
Figure 2
Assessment of Stress Index dynamics (with corresponding 95% CI) in the studied groups as a function of the OJ severity
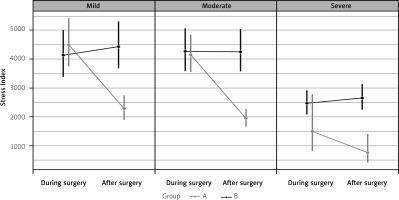
The pairwise comparison of mean SI values between groups showed statistically significant differences between the subgroups after surgery.
Thus, in the experimental group, the subgroup with mild OJ severity had a 1.9-fold (0.52 (95% CI: 0.43; 0.62); p ≤ 0.0001) lower stress index. In the subgroups with moderate and severe OJ, it was 2.1-fold (0.46 (95% CI: 0.38; 0.55); p ≤ 0.0001) and 3.4-fold lower (0.29 (95% CI: 0.14; 0.57); p = 0.0005), respectively, compared to the control group. This can be due to the significant surgical aggression of traditional surgical interventions.
The study of compensatory reserve in patients with GSD complicated by OJ has shown that the staged approach using endovideoscopic surgical interventions reduces overstrain of the adaptive mechanisms, thereby providing a lower degree of surgical aggression.
For a comparative assessment of the postoperative period course, the length of patients’ stay in the hospital was investigated.
The results obtained within the gamma regression model showed differences in the average length of hospitalization between the studied groups irrespective of OJ severity, patients’ age and gender, duration of jaundice, and character of the inflammatory process (p < 0.0001). The severity degree was also a statistically significant predictor (p < 0.0001). The effect of surgical intervention depended on the severity degree (p < 0.0001): the most significant differences between the groups were observed for severe OJ.
In the experimental group, the mean length of hospital stay was 7.23 (95% CI: 7.50; 6.98) bed-days for mild OJ, 13.17 (95% CI: 13.63; 12.74) bed-days for moderate, and 8.75 (95% CI: 10.21; 7.65) bed-days for severe OJ. In controls, it was 11.82 (95% CI: 12.40; 11.29), 16.56 (95% CI: 17.24; 15.93) and 17.15 (95% CI: 18.10; 16.29) bed-days, respectively (Figure 3). There was a reduction in length of hospital stay in patients in the experimental group compared to the control group, i.e. 1.6-fold for mild OJ, 1.3-fold for moderate OJ, and 1.9-fold for severe OJ. From the data presented, the differences between the groups being compared are significant.
Figure 3
Mean number of bed-days (with corresponding 95% CI) spent in hospital in the study based on the OJ severity
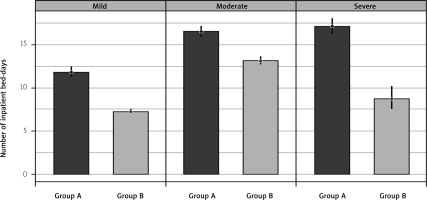
As a result, the use of minimally invasive procedures in patients significantly reduces the length of stay in the hospital compared to patients who underwent traditional surgery.
The effectiveness of OJ-complicated GSD treatment was also assessed in terms of the presence and severity of postoperative complications and lethal outcomes. The nature of postoperative complications is shown in Table VIII.
Table VIII
Postoperative complications in patients of the experimental and control groups
A binary logistic model revealed differences in the risk of postoperative complications between the study groups irrespective of the OJ severity and corrective covariates (p = 0.0115), while the severity degree of OJ was also a statistically significant predictor of such an outcome (p = 0.0005). The marginal estimate of the probability for postoperative complication development was 0.07 (95% CI: 0.17; 0.03) in the experimental group with mild OJ severity, 0.15 (95% CI: 0.25; 0.09) with moderate, and 0.14 (95% CI: 0.80; 0.01) with severe OJ. In the control group, these values were 0.15 (95% CI: 0.31; 0.07), 0.27 (95% CI: 0.4; 0.17), and 0.56 (95% CI: 0.74; 0.37), respectively (Figure 4).
Figure 4
Marginal estimates of the risk for postoperative complications in the study groups based on the OJ severity
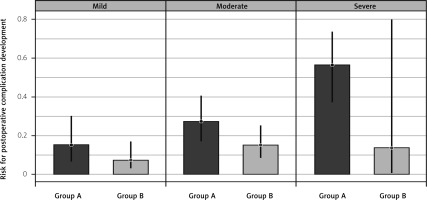
Reduced postoperative complications were reflected in the mortality of patients in the compared groups. The causes of lethal outcomes in the groups were acute pancreatitis, PATE, myocardial infarction, damage in the duodenum’s posterior wall, and progressive hepatic and renal failure. In patients with a mild OJ severity, the lethality was 1.2% in the experimental group and 1.8% in the control group; in patients with moderate OJ, it was 2.8% and 5.2%, respectively. In patients with severe OJ, the lethality was 5.4% in the experimental group and 9.3% in the control group. Comparative study of the surgical treatment results in patients with GSD complicated with OJ testifies to the advantage of minimally invasive techniques that reduce the risk of postoperative complications and decrease mortality almost two-fold.
Discussion
According to the data of earlier research efforts, the differential approach to treatment with minimally invasive technologies was reduced to applying a two-stage technique in the experimental group and a traditional approach in the control group without considering the degree of OJ severity [7, 8, 19–21].
Thus, a differentiated approach in the surgical treatment of GSD complicated with choledocholithiasis and obstructive jaundice using minimally invasive interventions significantly changed the surgical tactics. Also, it allowed avoidance of some severe complications in the one-stage correction of biliary pathology using traditional wide laparotomy.
Conclusions
The obtained results allow the following conclusions to be drawn:
Differentiation of minimally invasive surgical techniques for GSD with accompanying OJ based on jaundice severity allows decreased bilirubin levels: 1.7-fold (p ≤ 0.0001) in mild patients, 1.4-fold in moderate patients (p ≤ 0.0001), and 1.9-fold (p = 0.0017) in severe patients. Unlike traditional surgical interventions, the differentiated surgical approach allows the concentration of transaminase to be reduced (1.2- (p < 0.0001), 1.1- (p < 0.0007, p < 0.0002), and 1.3-fold (p = 0.0013, p = 0.0267) in mild, moderate, and severe patients) and GGT (1.5- (p < 0.0001), 1.4- (p < 0.0001), and 1.3-fold (p = 0.0193), respectively). In doing so, it helps to accelerate the resolution of intoxication, cholestasis, and cytolytic processes in the liver.
Application of minimally invasive surgery in patients with GSD complicated by OJ reduces hospitalization time by 1.6-fold at mild OJ, 1.3-fold – at moderate degree, and 1.9-fold – in the case of severe OJ (p ≤ 0.0001). Also, it reduces the number of postoperative complications in all subgroups depending on the OJ severity (p = 0.0005): 14.3% to 7.5%, 26.3% to 14.4%, and 46.5% to 21.6% in the case of mild, moderate, and severe OJ, respectively. The lethality dropped from 1.8% to 1.2%, from 5.2% to 2.8%, and from 9.3% to 5.4%, correspondingly, compared with the conventional surgery.
Due to a less traumatic effect, the differentiated approach to surgical correction in patients with GSD complicated by OJ helps to decrease the stress index: 1.9-fold (p ≤ 0.0001) in patients with a mild OJ, 2.1-fold (p ≤ 0.0001) in patients with moderate OJ, and 3.4-fold (p = 0.0005) in patients with severe OJ. Accordingly, the cortisol level was reduced 1.3- and 1.4-fold in patients with mild and moderate OJ, respectively, (p ≤ 0.0001) compared with open surgery. It resulted in reducing overstress adaptation mechanisms and preventing the inhibition of the body’s compensatory reserve.
Minimally invasive surgery in complex treatment of GSD complicated by OJ has a positive effect on LPO parameters expressed in a significant reduction of MDA emergence (1.2-fold in subgroups with a mild and moderate degree of OJ (p < 0.0001) and 1.4-fold (p < 0.0001)) – with severe degree). Besides, compared to traditional surgery, the catalase activity increased 1.1-fold in subgroups with a mild and moderate degree of OJ severity (p < 0.0001) and 1.3-fold – with severe OJ form (p < 0.0001).