Introduction
Pentalogy of Cantrell or Cantrell Syndrome is a rare developmental disorder in the course of which some characteristic birth defects are observed: loss of the anterior abdominal cavity above the level of the navel, developmental disorders of the lower part of the sternum, loss of the diaphragmatic part of the pericardium and congenital defects of the heart or large vessels [1,2]. This defect usually arises between the 14th and 18th day of embryonic life, and the conditions underlying its emergence are disorders of mesoderm migration [3,4]. This syndrome was first described in 1958 by Cantrell, Mark and Ravitch [1]. The incidence of pentalogy of Cantrell is quite difficult to estimate, but according to researchers it is about 5.5:1 million births and generally affects boys [4,5]. Although in most cases this disorder occurs sporadically, inheritance may be presumably related to the X chromosome.
There are many variants of this disorder, where a different constellation of coexisting defects is observed in both prenatal and postnatal ultrasound studies [6]. Based on 60 cases described in the literature, in 1972 Toyama proposed the pentalogy of Cantrell classification, which allows for better planning of diagnosis and treatment, as well as curability prognosis. This division includes three groups, the first group being patients with a full range of symptoms – five different developmental disorders, and the diagnosis is certain. The second group includes patients with a syndrome suspicion. Four symptoms are present, but a heart defect and developmental disorder of the anterior abdominal cavity need to coexist. In the third group of cases, where the diagnosis is incomplete, only some symptoms of the syndrome are observed, such as a defect in the sternum [7,8]. Pentalogy of Cantrell is already diagnosable in the first trimester of pregnancy. Usually, the rupturing of the continuity of the anterior chest cavity and abdominal walls is established. The presence of an ectopic heart and omphalocele is also characteristic and attention should be paid to the physiological omphalocele, which occurs before the 12th week of pregnancy, when only intestinal loops are outpouched into the umbilical cord.
The type of coexisting heart defect is crucial for the prognosis. In the case of pentalogy of Cantrell, the most commonly observed defect is the interventricular septum defect, and in half of the cases also the interatrial septum defect. Other less frequently diagnosed abnormalities are Fallot’s tetralogy, pulmonary valve stenosis or double outlet right ventricle (DORV) [9]. The coexistence of Cantrell Syndrome with extended nuchal translucency has also been described [10].
Case description
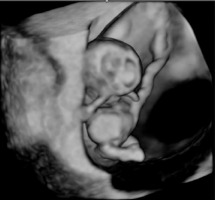
A thirty-three-year-old pregnant woman in her second pregnancy (the first pregnancy was unsuccessful – miscarriage at week 8 of pregnancy), visited a gynecologist for a routine check-up at week 12 of pregnancy, during which developmental disorders were found in the anterior chest cavity and abdominal walls. The woman was healthy, denied having chronic diseases, and was taking folic acid and vitamin preparations for pregnant women. The patient also denied the existence of any infections at an early stage of pregnancy. The woman was referred to the Laboratory of Prenatal Research, where, during prenatal ultrasound examination, the fetus was diagnosed with a complex defect of the skin and division of the body’s cavities in the form of pentalogy of Cantrell. The fetus was diagnosed with umbilical cord omphalocele (Figure 1), diaphragmatic hernia with diaphragmatic defect, sternal defect, ectopic heart and pericardial defect (Figures 2-3).
Moreover, the fetal heart seemed to possess four cavities, two slightly asymmetrical inflows of the ventricles and the origins of two vessels in abnormal relationships were visualized (Figures 4-5).
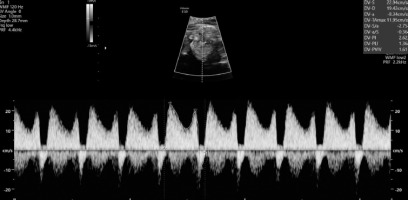
The swelling of the entire fetus was visualized – NT 5 mm (Figure 6) and reverse flow in the ductus venosus (Figure 7).
The patient was presented with possible options for managing the condition: continuing the pregnancy with a poor prognosis of survival, high risk of intrauterine death or death of the new-born after childbirth, as well as the admissibility of terminating the pregnancy at the current stage, in accordance with the Polish legislation due to serious and irreversible defects in the fetus. Throughout the hospitalization period, the patient also had unlimited access to psychological support. In the presence of the medical council, the woman decided to terminate the pregnancy.
Case analysis
Due to the heterogeneous picture of disorders occurring in Cantrell Syndrome and the small number of cases described in the literature, each case should be approached with caution and in an individual manner. Limited data on this disease may result from the high mortality observed in this condition, resulting from the coexisting severe heart defect, as well as from the decision of patients to terminate pregnancy in most cases.
The early diagnosis and determination of the heart defect – already possible in the first trimester of pregnancy – is particularly important, determining the method and order of treatment [6,10-13]. The relatively rare ectopic heart, where the heart muscle located outside the chest may be covered with nothing but the serous membrane or skin, is associated with a mortality rate of up to 95%. Figueroa et al. [14], among the 21 cases of pentalogy of Cantrell described by them, found ectopia and heart defects in 6 new- borns. Unfortunately, treatment attempts were unsuccessful [14]. Similar results were obtained in a study conducted by Malula et al. [15], where 4 out of 5 new-borns died with a diagnosis of ectopic heart. Zidere et al. [16] present more optimistic results in a study from 2008, where in three cases in which Cantrell Syndrome with fetal ectopic heart had been diagnosed, cardiac retraction into the chest was observed in subsequent ultrasound studies. After birth, the newborns underwent multi-stage surgery and survived [16]. Respondek- Liberska et al. [17] from the ICZMP Clinic of Prenatal Cardiology in Łódź in 2000 published a study describing 7 cases of patients in whom fetuses were suspected of Cantrell Syndrome and who decided to continue their pregnancy. Five fetuses had heart defects in the form of ventricular septal defect (VSD), VSD with relocation of large vessels, left heart hypolysis syndrome with relocation of large arterial trunks (HLHS with TGA) and a common atrioventricular canal with patent ductus arteriosus. In addition, one of the following defects was found in each fetus: eventration (7), skeletal defects (5), pleural effusion (3), diaphragmatic hernia (2) and kidney defects (1). Three newborns died after birth, and the other four died in utero.
Conclusions
Pentalogy of Cantrell is an extremely complex defect, where abnormalities in the structure of the heart are crucial for the prognosis, and they are additionally compounded by coexisting disorders. Until the 1990s, the survival rate of patients with Cantrell Syndrome oscillated around 37%, and in the last two decades it increased to about 60% [18,19]. This is undoubtedly related to early diagnosis, detecting specific disorders – especially a severe heart defect, which in turn determines further management and treatment. Huge progress in neonatal and anesthetic care is also important here [20,21].