Introduction
Acute pancreatitis (AP) is an inflammatory process of the pancreas that can range from mild, self-limited disease to severe disease, potentially resulting in death [1, 2]. In the United States, AP has become one of the most common gastrointestinal causes of hospitalisation [1, 2]. Although overall mortality has decreased, the incidence of AP is increasing [1]. Severe episodes of AP, specifically those cases associated with organ failure and infection, are more likely to result in prolonged hospitalisation and increased mortality [1]. Reliable means of early detection and indicators of severity in AP remain a challenge, hence the continued efforts of the medical community toward developing improved prognostic tools [3]. There are various scoring systems available that are aimed at classifying severity of AP. Many of these scoring systems have practical limitations, are complex, and remain underutilised. As a result, the investigation of biological markers that can predict prognosis of AP has been a topic of interest [1]. Sharma et al. examined the value of arterial blood gas (ABG) in a study that showed low arterial pH and bicarbonate levels and higher base deficit at presentation of AP predicted organ failure, need for intervention, and mortality with higher frequency [4]. Obtaining an ABG can be cumbersome and is a more expensive laboratory test when compared to peripheral blood sampling, particularly in areas with limited resources [2, 5]. A review of the literature shows that venous and arterial bicarbonate levels have sufficient agreement to be used interchangeably in many circumstances [5–8]. Most patients who present to the emergency department routinely have peripheral venous labs drawn.
Aim
Based on this data, we aim to investigate whether peripheral venous bicarbonate levels can be used as a marker of predicting severity in acute pancreatitis.
Material and methods
Patients
Patients were selected by conducting a chart review for patients between the ages of 18 and 80 years, from September 2015 to August 2017, who were diagnosed with AP. Largo Medical Centre is an acute-care community teaching hospital facility in Florida, which has 425 beds and includes four Intensive Care Units. Patients with established stage 4 or 5 chronic kidney disease (CKD), end-stage renal disease (ESRD), chronic respiratory failure, chronic pancreatitis, and/or pancreatic cancer were excluded.
Data collection
Severity of AP was defined as increased length of stay, organ failure, need for intervention, and/or mortality. Length of stay was quantified by the number of days elapsed from date of admission to date of discharge or expiration. Mortality was identified by encounter type, discharged versus expired. Organ failure was defined as the number of diagnoses that included acute kidney failure, acute respiratory failure, acute respiratory distress syndrome, and shock. Need for intervention was defined as the number of related procedures the patient underwent during their stay and included drainage or excision of the pancreas. Bicarbonate levels were obtained from peripheral venous sampling on the date of admission from the Basic Metabolic Panel (BMP) or Comprehensive Metabolic Panel (CMP). Patient demographics of gender, ethnicity, and race were also collected. The associations between bicarbonate level and length of stay, encounter type, organ failure, and need for intervention were analysed. Associations between bicarbonate levels and patient gender, ethnicity, and race were also examined.
Statistical analysis
The first data analysis examined the relationship between peripheral bicarbonate levels and length of stay. The data was modelled using a negative binomial distribution with a log-link function.
The second data analysis examined the relationship between the independent variables listed in Table I and dependent variable bicarbonate level. This data was modelled using a Gaussian distribution with an identity-link function. As multiple measures were analysed per individual, robust clustered standard errors were used. RStudio and R3.2.2 were used for all statistical analyses and significance was accepted at p < 0.05.
Table I
List of independent variables
Results
Ninety-nine patients were included in the final statistical analysis. The total sample size in the data set includes 106 encounters due to the fact that seven patients were re-admitted during the selected time frame.
Forty-three patients were male (43.4%) and 56 (56.6%) were female. The mean age for all patients included was 54.3 ±12.1 years. Ninety-two (92.9%) patients self-identified as non-Hispanic while 7 (7.1%) self-identified as Hispanic. Eleven (11.1%) patients self-identified as black, 78 (78.8%) as white, and 10 (10.1%) as other.
Results indicated a significant association between bicarbonate levels and both discharge type and number of diagnoses. A significant association was also found between bicarbonate levels and ethnicity. Bicarbonate levels were not found to be significantly associated with need for intervention or length of stay, nor were they related to any other patient demographics examined.
Mortality and organ failure
There was a significant association between bicarbonate levels and discharge type. Expired patients had statistically significant lower bicarbonate levels than discharged patients (95% CI: 0.62–10.04). A significant association was also observed between bicarbonate levels and organ failure, defined in the study design as the number of diagnoses. For every one-unit increase in the number of diagnoses, bicarbonate levels were decreased by 0.10 (95% CI: 0.01–0.20).
Patient demographics and bicarbonate levels
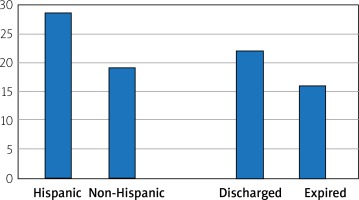
In a separate analysis, various patient demographics were also examined in relation to bicarbonate levels. A significant association was observed between bicarbonate levels and ethnicity. Non-Hispanic patients possessed significantly lower bicarbonate levels (95% CI: 1.12–17.72) than Hispanic patients (Table II, Figure 1).
Table II
Bivariate results
| Variable | Measure | N (%) | Bicarbonate Mean (SD) | Age Mean (SD) | LOS Median (IQR) | Procedures Median (IQR) | Diagnosis Median (IQR) |
|---|---|---|---|---|---|---|---|
| Gender | Female | 43 (43.4) | 19.62 (8.00) | 54.8 (11.5) | 7 (5–14) | 69 (55–107) | 23 (16–36) |
| Male | 56 (56.6) | 20.09 (9.01) | 53.8 (12.7) | 7 (4–15) | 80 (54–96) | 25 (18–32) | |
| Ethnicity | Hispanic | 7 (7.1) | 28.97 (11.47) | 51.5 (12.8) | 8 (5–14) | 47 (42–70) | 19 (10–28) |
| Non-Hispanic | 92 (92.9) | 19.19 (7.95) | 54.5 (12.2) | 7 (4–15) | 80 (55–104) | 23 (18–34) | |
| Race | Black | 11 (11.1) | 20.20 (5.78) | 50.3 (15.4) | 10 (2–26) | 77 (63–136) | 25 (22–39) |
| White | 78 (78.8) | 19.19 (8.29) | 53.8 (12.5) | 7 (4–14) | 69 (44–79) | 18 (10–28) | |
| Other | 10 (10.1) | 25.00 (11.70) | 54.9 (11.7) | 9 (7–14) | 82 (54–103) | 23 (18–33) | |
| Discharge status* | Discharged | 82 (77.3) | 21.99 (7.31) | 53.4 (11.5) | 8 (5–14) | 77 (52–101) | 23 (17–34) |
| Expired | 15 (14.1) | 15.97 (7.22) | 58.7 (15.0) | 5 (2–15) | 92 (61–115) | 26 (22–33) | |
| Other | 9 (8.6) | 21.78 (4.24) | 48.4 (15.9) | 0 (0–2) | 71 (58–107) | 19 (16–36) |
Discussion
Developing accessible and reliable predictors of severity in AP remains a clinical challenge. Several severity scales are currently available, which examine various lab values; however, the utility of venous peripheral bicarbonate levels has never been investigated to the best of our knowledge. Sharma et al. examined the utility of ABG in predicting severity of AP and found that lower arterial pH and bicarbonate levels predicted adverse outcomes of organ failure, need for intervention, and death with higher frequency. Our analysis found that lower bicarbonate levels were significantly associated with organ failure and mortality. In our analysis bicarbonate levels were obtained from peripheral venous sampling on the day of admission, suggesting that bicarbonate levels from BMP and/or CMP may be an under-recognised value that can potentially provide a predictor of severity. It remains unclear if bicarbonate levels obtained from ABG are superior to peripheral venous sampling values, because they can differ under certain circumstances. It also remains ambiguous whether, on admission, ABG should be obtained in the setting of AP when there is an absence of other compelling indications to obtain an ABG, such as respiratory distress or altered mental status. Further studies that directly compare bicarbonate levels from ABG to those from BMP and/or CMP should be performed to further investigate.
Interestingly, non-Hispanic patients were found to have overall lower peripheral mean bicarbonate levels than Hispanic patients. The mean bicarbonate level in the non-Hispanic group was 19 ±7.95 mmol/l. In the Hispanic group, the mean bicarbonate level was 28.97 ±11.47 mmol/l. This is a substantial difference in mean bicarbonate levels, but we feel that it cannot be concluded that non-Hispanic patients are more likely to progress to a severe course of AP when compared to Hispanic patients. Our study comprised 92.9% non-Hispanic patients and only 7.1% Hispanic patients. The above findings may be attributed to the fact that, overall, more non-Hispanic patients were included in the study. Further studies should be conducted where a larger Hispanic sample size is available to further investigate if ethnicity is a factor in the likelihood of increased severity of AP.
Lastly, prospective studies examining the utility of peripheral venous bicarbonate levels in the setting of AP should be conducted to determine whether our retrospective analysis findings are reproducible.
Conclusions
In our retrospective analysis, lower peripheral venous bicarbonate levels were significantly associated with increased organ failure and mortality in the setting of AP. Peripheral venous sampling should be promptly obtained upon admission in the setting of AP because it can be a useful, easily obtained data point that may assist in the prediction of severity in AP.