Introduction
Nonalcoholic fatty liver disease (NAFLD) is defined as hepatic steatosis in the absence of alcohol use and other causes of fatty liver. It is considered as the leading cause of chronic liver disease, with a global prevalence of 25.24% [1]. Nonalcoholic steatohepatitis (NASH) is a subgroup of NAFLD, which leads to cirrhosis and hepatocellular cancer. The NAFLD has strong association with metabolic syndrome and insulin resistance [2]. The estimated global prevalence of NAFLD in type 2 diabetes mellitus (DM) is 60% [3, 4]. Additionally, type 2 DM in NAFLD is associated with increased incidence of cirrhosis, hepatocellular cancer, and increased mortality (liver and cardiovascular related) [5–7]. The fat accumulation in the liver leads to liver inflammation, which can present as elevated transaminases, typically alanine transaminase (ALT) greater than aspartate transaminase (AST). The AST levels can increase with advance in fibrosis, and the AST : ALT ratio is high in cirrhosis [8, 9]. The subgroup of patients who progress to NASH require close monitoring and interventions to delay the progression of disease. The literature has shown improvement of hepatic steatosis and inflammation with thiazolidinediones and glucagon-like peptide 1 agonist, but the American Association for the Study of Liver Diseases (AASLD) does not recommend use of these agents specifically for NASH [2].
The inhibitors of sodium glucose cotransporter (SGLT-2 inhibitors) improve glycaemic control by reducing the renal glucose reabsorption. They also improve the cardiovascular outcomes as compared to placebo; as a result, the medications from this class are widely used in clinical practice [10, 11]. The EMPA-REG H2H-SU trial [10] has shown that empagliflozin use for 2 years caused a decrease in visceral and subcutaneous fat as compared to placebo. This indicates that the use of SGLT-2 inhibitors can be beneficial in terms of reducing hepatic steatosis [12]. The literature review showed few studies that measured the effects of SGLT-2 inhibitors on liver enzymes and hepatic steatosis.
Aim
In the present systematic review and meta-analysis, we aim to establish whether sodium glucose cotransporter inhibitors offer benefits in non-alcoholic fatty liver disease.
Material and methods
The study complies with preferred reporting items for systematic review and meta-analysis guidelines (PRISMA) and meta-analysis of observational studies and epidemiology (MOOSE) [13, 14]. The study was considered exempt by our institutional review board. The study was registered with PROSPERO (ID: CRD42021244301).
Database search and retrieval of the primary studies
The Pubmed, Medline, CINAHL, and Cochrane databases and ClinicalTrial.gov were searched through July 2020. The search items included sodium glucose cotransporter-2 inhibitor, canagliflozin, empagliflozin, dapagliflozin, luseogliflozin, ipragliflozin, liver enzymes, hepatic steatosis, non-alcoholic fatty liver disease, body weight, and liver fibrosis (Supplementary Tables SI A–D). In addition, we searched the references of the selected articles [10, 15–23] to find related articles that were not identified by the electronic searches. Pertinent studies were initially searched based on the title and the abstract, then the full text was read to verify the relevance. The search, title, abstract, full-text screening, and data extraction were completed in duplicate. A third investigator was brought in to resolve differences when needed. We also contacted all primary investigators listed on the NIH Clinical Trial Registry from eligible studies identified during the title screening to inform them of this review and inquire about information regarding any publications resulting from their trials. This review placed no constraints on language or date of publication. Animal studies and incomplete studies (pilots, preliminary reports) were excluded. Studies without comparison groups were also excluded (i.e. case-reports or case-series).
Inclusion criteria
We used the following inclusion criteria: prospective studies in type 2 diabetes mellitus patients with a control group, which looked at liver enzymes, hepatic steatosis, and body-weight change with sodium glucose cotransporter-2 inhibitor. Length of follow-up was from 8 to 52 weeks. The studies without control groups were excluded.
Primary and secondary outcomes
The primary outcome was change in alanine transaminase and aspartate transaminase, and secondary outcomes were change in body weight index, liver fibrosis (measured by fibrosis-4 score), and hepatic steatosis (measured with MRI-estimated proton density fat fraction).
Study selection and data identification
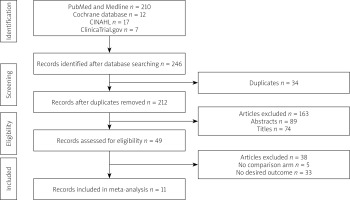
The studies were selected following PRISMA guidelines, which include identification, screening, eligibility, and inclusion in a systemic review or meta-analysis if applicable. Duplicate studies and those that did not meet the inclusion criteria were excluded (Figure 1). Two authors (WA and AM) determined the eligibility criteria and selected studies evaluating the effect of SGLT-2 inhibitors on liver enzymes, body mass index (BMI), hepatic steatosis, and hepatic fibrosis. Any differences between the findings of the 2 reviewers were resolved after independent assessment by a third reviewer (WQ). The data extraction was started once there was consensus between 3 reviewers.
The authors collected the following data: name of the author, year of publication, region, journal, type of clinical trial, number of subjects, dosages of SGLT-2 inhibitor, follow-up duration, comparative group, AST, ALT, patients’ demographics, hepatic steatosis, and hepatic fibrosis. After the completion of data extraction, the data sheet was compared between 2 reviewers and any differences were discussed with the third reviewer to reach a consensus.
Statistical analysis
The results of all selected clinical trials were pooled by generic invariance methods, and a random effects model was used to report the estimated outcome. The outcomes were presented as standard difference of mean (SMD) with 95% confidence interval (CI). We assessed the quality of clinical trials using Cochrane’s risk of bias tool, mentioned in the Cochrane’s Handbook, Chapter 8 [24, 25]. The tool includes 7 main domains: randomization, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, attrition bias, reporting bias, and other bias. Funnel plot for asymmetry was used to assess the publication bias. The study demographics, clinical characteristics, event rates, and 95% CIs for the outcomes were extracted. We extracted the standard difference of mean (SMD) for SGLT-2 inhibitors in NAFLD studies from published studies. The effect sizes were obtained from intention-to-treat analyses and fully adjusted models in the included clinical trials. The primary analysis measured the pooled estimate of improvement in liver inflammation. To study heterogeneity, we hypothesized that the effect sizes might differ because of the methodological quality of the studies. Thus, we utilized a random effects model as described by DerSimonian-Laird [26], which assumes that the studies included in the meta-analysis are a random samples of hypothetical study populations.
Statistical heterogeneity was assessed and quantified using the chi-square test and I2 statistics. If I2 < 50%, p > 0.1, we assumed minimal heterogeneity was present and chose a fixed effects model. A random effects model was used when the I2 statistic was ≥ 50%, p ≤ 0.1. We assessed publication bias subjectively by visual inspection of Begg’s funnel plot [27] and objectively by Egger’s regression asymmetry test because funnel plots may be inaccurate in the assessment of very large studies [28, 29]. If the meta-analysis has captured all relevant studies, then the funnel plot is expected to be symmetric. However, if there is asymmetry in the plot, it is expected that some studies are missing from the analysis. All analyses were performed using STATA (College Station, Texas).
Results
Literature search
The initial search yielded 246 studies. There were 34 duplicate studies, and 163 records were excluded after reviewing the title and abstracts. In total, 49 articles were thoroughly reviewed. After using the inclusion criteria, 11 studies were selected for the analysis. Five studies had no control group, and 33 studies did not study the desired result (Figure 1).
The details of the demographic and clinical characteristics of 11 studies were included in the analysis. The inclusion and exclusion criteria were included. All studies were double blinded trials. Four studies were conducted in Japan, 2 in the USA, and 1 each in Finland, Sweden, and India. The EMPA-REG trial included 42 countries, including North America and Asia [10].
A total of 10,555 patients were included in this meta-analysis. Among these patients 7125 received SGLT-2 inhibitors and 3430 were given placebo treatment. The placebo treatment included non-insulin standard type 2 diabetes treatment, i.e. metformin, glimepiride, pioglitazone, and DPP-4 inhibitor. Of these 11 studies, 10 RCTs studied the effect of SGLT2 inhibitor on alanine transaminase, 8 RCTs studied the effect on aspartate transaminase, 4 RCTs studied hepatic steatosis (3 with magnetic resonance imaging-derived proton density fat fraction MRI-PDFF and 1 with controlled attenuation parameter CAP score). The duration of the treatment was 8 to 52 weeks. Only 3 studies included the effect of treatment on liver fibrosis using the fibrosis-4 (FIB-4) score. Table I shows the study characteristics, and Table II shows the baseline characteristics of the study subjects.
Table I
Characteristics of the study
| Studies and year of publication | Design | Region | Comparative treatment | Follow-up | Number cases/control | Inclusion criteria | Exclusion criteria | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Latva-Rasku 2019 [15] | RCT-DB | Finland | Dapagliflozin 10 mg/day vs. metformin ± DPP-4 inhibitor | 8 weeks | 15/16 | Age 35–70, BMI < 40 kg/m2 | Concomitant diabetes medication, CrCl < 60 ml/min, AST and ALT > 3 times UNL or bilirubin > 2 mg/dl, symptomatic heart failure, unstable coronary syndrome, BP > 160/100 mm Hg and alcohol abuse | Improvement in glycaemic control, weight, fatty liver and liver enzymes |
| Aso 2019 [16] | RCT-open | Japan | Dapagliflozin 5 mg/day vs. standard treatment without SGLT-2 inhibitor | 24 weeks | 33/24 | Type 2 diabetes mellitus with NAFLD, age ≥ 20 years, HbA1c 6–12% | Use of insulin for at least 3 months, history of other liver diseases including viral, autoimmune, alcoholic hepatitis | Improvement in hepatic steatosis, liver enzymes, glycaemic control, insulin resistance, BMI, lipid profile |
| Kuchay 2018 [17] | RCT-open | India | Empagliflozin 10 mg vs. standard treatment | 20 weeks | 22/20 | Age > 20 years and had documented MRI-PDFF > 6%, uncontrolled type 2 DM (HbA1c 7–10%) | HbA1c > 10%, history of alcohol abuse, evidence of other liver disease including viral, autoimmune hepatitis, DILI (based on biopsy), history of gastric bypass, use of drugs which can influence liver fat within 30 days of randomization, cirrhosis, HIV, renal disease, HCC, pregnancy | Change in liver fat content, changes in liver enzymes |
| Kurinami 2018 [31] | Non-randomized prospective | Japan | Dapagliflozin 5 mg vs. non-SGLT-2 inhibitors (metformin, sulfonylurea, DPP-4 inhibitor, alpha glucosidase inhibitors, glinide) | 24 weeks | 28/27 | Type 2 diabetes mellitus HbA1c < 7% | Type 1 DM, dementia, inflammation, CKD (GFR < 45 ml/min/ 1.73 m2), BMI > 35 kg/m2, diabetic ketoacidosis, severe liver injury, heavy alcohol use | Liver-to-spleen attenuation ratio, liver size, hepatic insulin extraction ratio, C-peptide to insulin ratio, liver enzymes |
| Shibuya 2018 [18] | RCT-open | Japan | Lusegliflozin 2.5 mg qd vs. metformin | 26 weeks | 16/16 | HbA1c 6–10%, age 20–70 years, absence of viral and alcoholic hepatitis | Myocardial infarction, GFR < 45 ml/min/ 1.72 m2, angina pectoris, use of diuretics, weight loss in last 3 months, cerebral apoplexy | Change in liver spleen ration, glycaemic control, visceral fat volume, BMI, liver enzymes |
| Ito 2017 [19] | RCT-open | Japan | Ipragliflozin 50 mg qd vs. pioglitazone 15–30 mg qd | 24 weeks | 32/34 | Type 2 DM with HbA1c 7–11%, NAFLD, BMI < 45 kg/m2 | Other causes of liver disease (viral, autoimmune, alcohol), GFR < 45 ml/min/ 1.72 m2 or serum creatinine > 1.5 mg/dl, serious diabetes complication, insulin dependence, heart failure NYHA III, IV, myocardial or cerebral infarction, decompensated cirrhosis | Liver spleen ration, glycaemic control, changes in body weight, AST, ALT, abdominal visceral fat and FIB4 score |
| Bando 2017 [20] | RCT-open | Japan | Ipragliflozin 50 mg vs. placebo | 12 weeks | 40/22 | Age 20–65 years, with T2DM for at least 12 weeks, (BMIs) of 24.0–40.0 kg/m2, and HbA1c 7.0–10.0% | Fasting triglycerides > 400 mg/dl, type 1 diabetes, GFR < 60 ml/min/ 1.73 m2, alcohol use > 2 g/day, hepatitis B & C, autoimmune hepatitis, neurogenic bladder, BPH, history of cardiac event, pregnancy, breastfeeding, immunosuppressed | Changes in ALT, visceral and subcutaneous fat area, liver-to-spleen attenuation ratio, body weight |
| EMPA-REG 2015 [10] | RCT-DB | 42 countries | Empagliflozin 10–25 mg vs. placebo | 28 weeks | 4342/2148 | Age ≥ 18 years, BMI ≤ 45 kg/m2, GFR < 30 ml/min/ 1.72 m2, on glucose stabilizing therapy for at least 12 weeks, HbA1c 7–10% | Death from cardiovascular disease, nonfatal cardiovascular disease, unstable angina | |
| Leiter 2016 [21] | RCT-open label | North America | Canagliflozin 100 and 300 mg vs. placebo including sitagliptin | 52 weeks | 1667/646 | Adults > 18, type 2 diabetes mellitus | Canagliflozin 100 mg add on to metformin | Glycaemic control, liver enzyme change, change in body weight |
| Cefalu 2013 [22] | RCT-DB | USA | Canagliflozin 100 mg qd or 300 mg qd vs. glimepiride | 52 weeks | 482/483,485* | Age 18–80 years, HbA1c 7–9.5%, on standard metformin therapy ≥ 1.5 gm qd for 10 weeks | Severe hyperglycaemia episode in last 6 months, GFR < 60 ml/min/1.73 m2, thiazolidinedione with 16 weeks | Glycaemic control |
| Eriksson 2018 [23] | RCT-DB | Sweden | Dapagliflozin 10 mg qd vs. placebo | 12 weeks | 21/21 | Age 40–75, type 2 DM, on metformin ± sulfonylurea for 3 months, BMI 25–40 kg/m2, had MRI-PDFF | Use of SGLT2i, GLP1 agonist, and insulin, alcohol use, inability to undergo MRI, other liver diseases, CrCl < 60 ml/min | Change in HbA1c, non-esterified fatty acid, fasting insulin, HOMA-IR, PDFF content |
[i] RCT-DB – randomized control trial double blinded, DPP4 – dipeptidyl peptidase, BMI – body mass index, UNL – upper normal limit, AST – aspartate aminotransferase, ALT – alanine aminotransferase, CrCl – creatinine clearance, HbA1c – glycosylated haemoglobin, SGLT-2 – sodium glucose cotransporter 2, DM – diabetes mellitus, NAFLD – nonalcoholic fatty liver disease, MRI-PDFF – magnetic resonance imaging-derived proton density fat fraction, HOMA-IR – Homeostatic Model Assessment of Insulin Resistance, GFR – glomerular filtration rate.
Table II
Baseline parameters of study population
| Studies and year of publication | Age [years] maen ± SD | Female sex (%) | BMI [kg/m2] mean ± SD | Hepatic steatosis by PDFF (%) | ALT [IU/l] mean ± SD | AST [IU/dl] mean ± SD | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Control | Cases | Control | Cases | Control | Cases | Control | Cases | Control | Cases | Control | ||
| Latva-Rasku 2019 [15] | 62 ±8.4 | 60 ±7.4 | 13.3 | 25 | 32.1 ±3.9 | 31.7 ±5.0 | 22 ±11% | 21 ±9.3 | 50 ±21 | 38 ±14 | 30 ±10 | 32 ±12 | |
| Aso 2019 [16] | 56.2 ±11.5 | 57.1 ±13.8 | – | – | 27.6 ±4.7 | 28.3 ±3.5 | – | – | 38 | 32 ±18 | 28 | 26 | |
| Kuchay 2018 [17] | 50.7 ±12.8 | 49.1 ±10.3 | 9 | 8 | 30 ±3.8 | 29.4 ±3.1 | 16.2 ±7 | 16.4 ±7.3 | 64.3 ±20.2 | 65.3 ±40.3 | 44.6 ±23.5 | 45.3 ±24.3 | |
| Kurinami 2018 [31] | 55.5 ±8.8 | 56.6 ±8.0 | 28.6 | 37 | 28 ±2.6 | 26.7 ±3.4 | – | – | 26.5 (19.0–43.8) | 21.0 (16.5–28.0) | 25.0 (19.0–1.8) | 22.0 (19.5–25.0) | |
| Eriksson 2018 [23] | 65 ±6.5 | 65.6 ±6.1 | 23.8 | 19.1 | 30.5 ±2.8 | 30.3 ±3.1 | 17.3 ±9.1 | 15.1 ±6.5 | – | – | – | – | |
| Shibuya 2018 [18] | 51 ±4 | 60 ±7 | 37.5 | 50 | 27.9 ±1.85 | 27.2 ±5.41 | – | – | 49.5 ±28.89 | 39 ±24.44 | – | – | |
| Ito 2017 [19] | 57.3 ±12.1 | 59.1 ±9.8 | 56 | 47 | 30.7 ±5.0 | 29.9 ±6.2 | – | – | 57.4 ±27.3 | 53.1 ±26.6 | 39.7 ±16.7 | 43.3 ±20.5 | |
| Bando 2017 [20] | 54.8 ±9.3 | 55.4 ±7.5 | 35 | 36.4 | 27.8 ±3.9 | 27.3 ±3.1 | – | – | 49 ±36 | 41 ±35 | 35 ±19 | 30 ±17 | |
| EMPA-REG 2015 [10] | – | – | – | – | – | – | – | – | 25.5 ±13.8 | 26.2 ±15.3 | 22.5 ±9.6 | 22.9 ±10.3 | |
| Leiter 2013 [21]: | |||||||||||||
| Canagliflozin 100 mg | 56 ±10 | 56 ±10 | 51 | 48 | 32 ±6 | – | – | – | 27.8 ±15.3 | 27.6 ±14.3 | 23.0 ±9.6 | 22.9 ±9.9 | |
| Canagliflozin 300 mg | 56 ±10 | 56 ±10 | 52 | 48 | 32 ±6 | – | – | – | 28.6 ±18.3 | 27.6 ±14.3 | 23.7 ±13.1 | 22.9 ±9.9 | |
| Cefalu 2013 [22]: | |||||||||||||
| Canagliflozin 100 mg | 56.4 ±9.5 | 56.3 ±9 | 48 | 45 | 31 ±5.3 | – | – | – | 29.8 ±16.1 | 29.2 ±17.1 | 24.3 ±11 | 23.7 ±10.9 | |
| Canagliflozin 300 mg | 55.8 ±9.2 | 56.3 ±9 | 50 | 45 | 31.2 ±5.4 | – | – | – | 28.9 ±16.7 | 29.2 ±17.1 | 23.5 ±10.8 | 23.7 ±10.9 | |
Effect on the transaminases
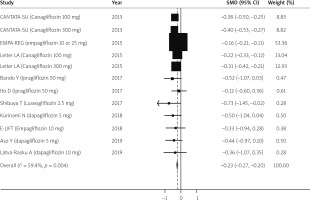
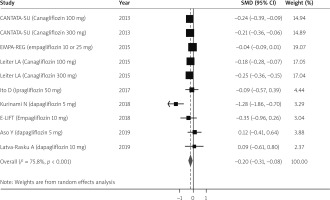
For adults, 10 clinical trials provided the data for the meta-analysis. A total of 7106 cases and 3411 controls had ALT measured over the study period. After combining results, the pooled standard difference of mean (SMD) for improvement in ALT after randomly assigning to SGLT-2 inhibitor treatment as compared to placebo was (SMD = –0.22, 95% CI: –0.27 to –0.20), which indicates a reduction in the ALT levels with treatment. In total, 6793 cases and 3237 controls had AST levels measured. The pooled SMD for improvement in AST levels also favoured the use of SGLT-2 inhibitors (SMD = –0.20, 95% CI: –0.31 to –0.08). Figures 2 and 3 show the forest plots for the estimated effect of treatment with 95% confidence intervals for AST and ALT.
Effect on body weight and hepatic steatosis
The largest study of this meta-analysis, EMPA-REG, did not analyse the effect of the treatment on hepatic steatosis and BMI [10]. Three studies evaluated the hepatic steatosis with MRI-estimated proton density fat fraction (MRI-PDFF) [15, 17, 23] and 1 study with continuous attenuation parameter (CAP score) [16]. Another study from Germany demonstrated improvement of fat content with Empagliflozin; the steatosis was measured using volume-selective proton magnetic resonance spectroscopy (H-MRS) [30].
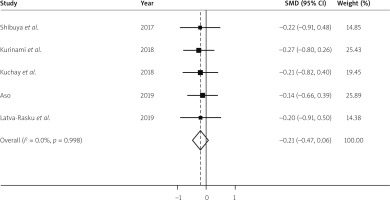
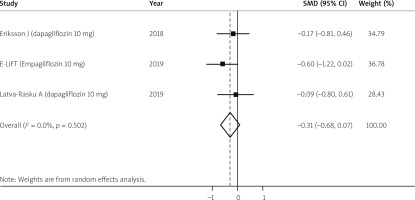
The SGLT-2 inhibitor treatment did not cause a significant decrease in body weight as compared to the placebo (SMD = –0.21, 95% CI: –0.47 to 0.06) (Figure 4). Hepatic steatosis was measured in 56 cases and 55 controls utilizing MRI-PDFF. The analysis shows that as compared to controls the SGLT2 inhibitor treatment caused trends toward a decrease in hepatic steatosis but was not statistically significant (SMD = –0.31, 95% CI: –0.68 to 0.07) (Figure 5). The 2 studies that showed improvement in steatosis utilizing H-MRS and CAP score were not included in this analysis because the parameters were different as compared to MRI-PDFF [16, 30].
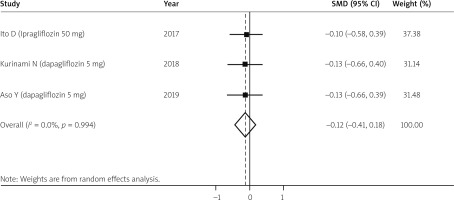
Hepatic fibrosis
Only 3 studies measured fibrosis utilizing the FIB-4 score during the treatment [16, 19, 31]. There were 93 patients who received SGLT2 inhibitor and 85 received placebo. Although there was a trend towards improvement of hepatic fibrosis it was not statistically significant (SMD = –0.12, 95% CI: –0.41 to 0.18) (Figure 6).
Adverse events
Fewer serious adverse events were seen in the SGLT-2 inhibitor as compared to the control group. The side effects from these medications were mild to moderate. Polyuria and urine tract infection were commonly seen in the treatment group but did not lead to discontinuation of treatment. Other uncommon side effects included dizziness, fatigue, arthritis, and balanoposthitis [17, 21, 22, 23].
Heterogeneity and bias assessment
There was minimal heterogeneity in the assessment in measurement of BMI, steatosis, and fibrosis (I2 < 25%), but the ALT and AST analysis showed moderate to high statistical bias (I2 > 50%). Funnel plots were created for ALT and AST, and some asymmetry was noticed in the included clinical trials (Supplementary Figures S1 A, B). Few studies on the right side of the plot were missed. Statistically significant results are published more commonly and faster, which creates a bias in the literature and can overestimate the effect of intervention [32]. The funnel plots for hepatic steatosis, fibrosis, and BMI measurement were symmetrical (Supplementary Figures S2 A–C).
We found an overall moderate risk of bias in qualities of study. All studies adequately reported the randomization of patients, except for Kurinami et al. [31]. Regarding allocation concealment, only 2 studies were put at high risk of bias because their allocation methods were open [17, 31]. Regarding the blinding, we noted that 7 of the included studies [16–21, 31] were not blinded (open-label trials). Other domains of bias were found to be at low risk (Supplementary Figure S3).
Discussion
This systematic review of existing clinical trials of sodium glucose cotransporter 2 inhibitor in adults with type 2 diabetes mellitus showed that the use of these medications reduced the ALT and AST when compared with other non-insulin-based diabetes treatments. The decrease in AST and ALT were more prominent in studies where the baseline levels were higher. Although there was a trend for improvement, the use of SGLT-2 inhibitors did not show statistically significant improvement of steatosis, fibrosis, and BMI. The common side effects include polyuria and urinary tract infection.
The SGLT-2 inhibitor effect on glycaemic control is independent of insulin sensitivity and β-cell function, and they do not cause hypoglycaemia unlike other type 2 diabetes mellitus treatments. A mouse study showed that empagliflozin has an anti-steatotic, anti-inflammatory effect and reduces the development of NASH [33]. It is unknown if the improvement in glycaemic control causes improvement of liver functions. A study showed that better glycaemic control and weight control may have contributed in the improvement of hepatic steatosis and liver enzymes [21]. The EMPA-REG trial showed improvement in ALT independently of the glycaemic control [8, 10], and the E-LIFT trial showed that there was no relation between the improvement of fat content and glycaemic control [17].
The available prospective studies suggest that the use of SGLT-2 inhibitors in type 2 diabetes mellitus is associated with significant reduction of liver enzymes, particularly ALT, as compared to standard treatments including metformin [15, 17], dipeptidyl peptide-4 (DPP-4) inhibitors [15, 21], and glimepiride [22]. A retrospective study from Canada showed weight, glycaemic control, and independent improvement of ALT levels with SGLT-2 inhibitors as compared to incretins [34]. The study by Ito et al. [19] showed improved weight with an SGLT-2 inhibitor as compared to pioglitazone but no significant benefit in terms of liver enzyme improvement and glycaemic control. A few studies from Japan measured fibrosis using the Fib-4 score [16, 19, 31]. The pooled analysis did not show any benefit in terms of fibrosis improvement as compared to controls, but the Aso et al. [16] group showed improvement in liver stiffness with 24 weeks of using dapagliflozin using the same cohort [35]. The AASLD suggests possible benefit with the use of pioglitazone in NASH patients based on the RCTs which showed improved histology. There is no comment on the use of SGLT-2 inhibitors for NAFLD treatment [2, 36, 37]. Although the studies regarding the effect of SGLT-2 inhibitors on the liver fibrosis are insufficient to draw firm conclusions, there was a trend towards the regression of fibrosis, but it is not statistically significant.
The strength of our meta-analysis is the novelty of the study. There are only a few systematic reviews in the literature that demonstrated improvement in liver enzymes and cholesterol. These reviews missed the major studies (CANTATA-SU and EMPA-REG), and retrospective studies were included. Also, women were underrepresented in the included clinical trials [38, 39]. Our study showed the same results. We performed a comprehensive search, so there is less likelihood that any eligible study has been missed. The included studies are diverse; they were conducted in Asia, Europe, and the United States, so the results can be generalized.
Our study has some limitations. First, we did not have access to the patient data and used the pooled data from prospective studies. Second, the effect of fibrosis was collected in only 3 studies and the follow-up period was not long enough. The outcomes were measured with either blood test or imaging, which are not as accurate as liver biopsy. There is only 1 prospective single-arm study which showed histological improvement of fibrosis and inflammation with canagliflozin [40]. The study population was small, and there was no comparison group, so it is hard to draw firm conclusions. Third, most of these randomized trials were focused on the treatment of type 2 diabetes mellitus and metabolic syndrome rather than NASH; the patients with elevated liver enzymes were assumed to have NASH.
Conclusions
Type 2 diabetes mellitus is commonly associated with non-alcoholic fatty liver disease. The use of sodium glucose cotransporter-2 inhibitor in type 2 diabetes mellitus use can improve liver inflammation as compared to standard medical treatment. This anti-inflammatory effect was also seen with modest doses. There was a trend towards the improvement of liver fibrosis and steatosis. Studies based on liver biopsy with longer follow-up are recommended to get a better understanding. The beneficial effect on glycaemic control and liver enzymes, and the low adverse event profile suggest that these medications are potential treatment options for NAFLD.