Introduction
Distal malignant biliary obstruction (MBO) is usually caused by primary biliary and pancreatic tumours [1–5]. Between 42% and 77% of patients with distal MBO suffer from pancreatic carcinoma (PC) [4, 6, 7]. PC itself is a highly malignant tumour; moreover, when it is the cause of distal MBO, surgical resection is only possible in a minority (10–20%) of cases, and even then the 3- and 5-year survival rates of these patients are just 18–52% and 5–31%, respectively [8]. When patients are diagnosed with MBO caused by PC, only palliative treatment options are feasible.
At present, endoscopic or percutaneous metal stenting is the first choice for patients with distal MBO caused by PC [9, 10]. However, stenting alone cannot treat or cure the PC, and tumour progression usually limits both the stent patency and the long-term overall survival (OS) of the patient. Therefore, anticancer treatments in addition to stenting should be used for patients with distal MBO caused by PC. Several anticancer treatments, including chemotherapy, radiotherapy, and combination chemoradiotherapy, are used to extend both stent patency and patient OS [8–10]. At present, advances in the use of high-intensity focused ultrasound (HIFU) ablation in addition to stenting to treat PC have been made owing to the non-invasive and non-toxic nature of this therapeutic modality [11–15]. Here, we have investigated the efficacy of this treatment combination using a meta-analysis. Meta-analyses can reduce potential sample bias and increase statistical power in comparison to single studies with small samples.
Aim
This meta-analysis aimed to analyse the clinical efficacy of stenting with HIFU ablation for patients with distal MBO caused by PC.
Material and methods
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) reporting guidelines [16]. Databases, including PubMed, Cochrane Library, Embase, Wanfang, VIP, and CNKI, were searched for relevant articles published through March 2021 based on the following search strategy: (((biliary [Title/Abstract]) AND (((stent [Title/Abstract]) OR (SEMS [Title/Abstract])) OR (drainage [Title/Abstract]))) AND (((obstruction [Title/Abstract]) OR (stenosis [Title/Abstract])) OR (stricture [Title/Abstract]))) AND ((high-intensity focused ultrasound [Title/Abstract]) OR (HIFU [Title/Abstract])). This work was registered in https://inplasy.com/ (No. INPLASY 202130047).
Study inclusion criteria were as follows: type of study: comparative studies; disease: distal MBO caused by PC; types of intervention: biliary stenting versus biliary stenting with HIFU ablation; language: any.
The following types of studies were excluded: (a) single-arm studies; (b) case reports; (c) animal studies; (d) review articles.
Data
Data including publication year, study design, authors, baseline patient characteristics, and treatment information were extracted from the identified studies by 2 independent investigators. Any disputes were resolved by consultation with a third investigator.
Quality assessment
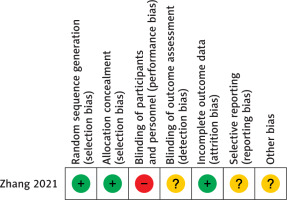
The potential bias in randomized controlled trials (RCTs) was assessed by the Cochrane risk of bias tool for bias risks in detection, selection, reporting, attrition, and performance, amongst others.
Non-RCT studies were assessed with the 9-point Newcastle-Ottawa scale [17]. Scores of < 4, 4–6, and ≥ 7 represented high, moderate, and low bias risks, respectively.
Endpoints and definitions
Stent dysfunction was the primary endpoint. Secondary endpoints included improvement of total bilirubin (TBIL), stent patency, clinical response rate to HIFU, OS, and complications.
Stent dysfunction was defined as the migration or re-obstruction of the stent. A positive clinical response to HIFU was the detection of tumour necrosis or reduction on computed tomography (CT) assessment [11–15]. OS was defined as the interval between stent insertion and death.
Statistical analysis
RevMan v5.3 and Stata v12.0 were utilized for all statistical analyses. The pooled odds ratios (ORs) and 95% confidence intervals (CIs) for dichotomous variables were calculated using the Mantel-Haenszel approach, while pooled estimates of the mean difference (MD) with 95% CIs were determined for continuous variables. Stent patency and OS between groups were compared using hazard ratios (HRs) with 95% CIs. Heterogeneity among the included studies was gauged using the χ2 test and the I2 statistic (I2 > 50% indicating significant heterogeneity). Fixed-effects models were used in the absence of any significant heterogeneity. Sources of potential heterogeneity were identified via sensitivity analysis. The pooled clinical response rates were calculated using Stata v12.0. Funnel plots were used to analyse the potential publication bias.
Results
Studies
Twenty-nine potentially relevant reports were initially identified, and 5 of these were finally included (Figure 1). Four studies were retrospective [11–14], and one was an RCT [15]. These studies included 142 patients who underwent biliary stenting alone and 132 patients who underwent biliary stenting with HIFU ablation (Table I). All the stents were self-expanding metal stents with a diameter of 8 mm.
Table I
Characteristics of the included studies
| Study/year/country | Design | NOS | Stent type | Groups | Sample size | Age [years] | Cancer stage | ECOG PS |
|---|---|---|---|---|---|---|---|---|
| Cao/2010/China [11] | Retrospective | 7 | Metal | Stent | 6 | Not given | Not given | Not given |
| Stent + HIFU | 5 | Not given | Not given | Not given | ||||
| Niu/2016/China [12] | Retrospective | 7 | Metal | Stent | 7 | Not given | Not given | 0, 1, ≥ 2 |
| Stent + HIFU | 9 | Not given | Not given | 0, 1, ≥ 2 | ||||
| Xia/2017/China [13] | Retrospective | 8 | Metal | Stent | 42 | 63.6 | II-IV | 2–3 |
| Stent + HIFU | 38 | 64.6 | II-IV | 2–3 | ||||
| Yang/2019/China [14] | Retrospective | 8 | Metal | Stent | 41 | 63.6 | II-IV | 2–3 |
| Stent + HIFU | 34 | 65.2 | II-IV | 2–3 | ||||
| Zhang/2021/China [15] | Randomized controlled trial | – | Metal | Stent | 46 | 63.2 | II-IV | 2.5 |
| Stent + HIFU | 46 | 64.9 | II-IV | 2.5 |
The included RCT was an open-label study. The outcome assessment blinding, selective reporting, and other potential biases were unclear for this included RCT [15] (Figure 2). Newcastle-Ottawa scale scores between 7 and 8 were found for the retrospective studies (Table II).
Table II
Characteristics of the treatment outcomes
| Study | Groups | ΔTBIL [µmol/l] | Stent dysfunction | Patency | Cholangitis | Pancreatitis | Survival |
|---|---|---|---|---|---|---|---|
| Cao [11] | Stent | Not given | 3/6 (50%) | Not given | Not given | Not given | Not given |
| Stent + HIFU | Not given | 1/5 (20%) | Not given | Not given | Not given | Not given | |
| Niu [12] | Stent | Not given | 3/7 (42.9%) | Not given | Not given | Not given | Not given |
| Stent + HIFU | Not given | 2/9 (22.2%) | Not given | Not given | Not given | Not given | |
| Xia [13] | Stent | 106.6 | 9/42 (21.4%) | Not given | Not given | Not given | 145 d |
| Stent + HIFU | 105.6 | 6/38 (15.8%) | Not given | Not given | Not given | 209 d | |
| Yang [14] | Stent | 103.1 | 13/41 (31.7%) | 118 | 5/41 (12.2%) | 0/41 (0%) | 118 d |
| Stent + HIFU | 146.4 | 7/34 (20.6%) | 175 | 3/34 (8.8%) | 1/34 (2.9%) | 175 d | |
| Zhang [15] | Stent | 103.8 | 15/46 (32.6%) | 120 | 9/46 (19.6%) | 1/46 (2.2%) | 140 d |
| Stent + HIFU | 119.7 | 9/46 (19.6%) | 188 | 7/46 (15.2%) | 1/46 (2.2%) | 218 d |
Improvements in TBIL
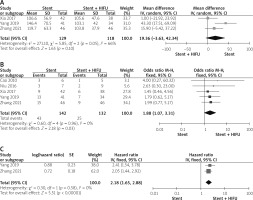
Three studies reported data on TBIL improvement [13–15]. The pooled ΔTBIL values were similar between the 2 groups (p = 0.10, Figure 3 A). These studies showed significant heterogeneity (I2 = 66%), which disappeared (I2 = 0%) after exclusion of Yang et al. [15]. The pooled ΔTBIL values between the groups remained comparable after the removal of the study (p = 0.26).
Stent dysfunction
Data on stent dysfunction were included in all studies. The pooled rate of stent dysfunction was significantly greater in the stenting alone group (30.3% vs. 18.9%, p = 0.03, Figure 3 B). No significant heterogeneity was seen among these studies (I2 = 0%).
Stent patency
Two studies reported data on the duration of stent patency [14, 15]. The pooled HR for stent patency duration indicated that the patency duration was longer in the stenting with HIFU ablation group (HR = 2.18; 95% CI: 1.65–2.88, p < 0.0001, Figure 3 C). No significant heterogeneity was observed among these studies (I2 = 0%).
OS
Three studies reported OS data [13–15]. The pooled HR for OS indicates that the OS was longer in the stenting with HIFU ablation group (HR = 2.37; 95% CI: 1.87–3.01, p < 0.0001, Figure 3 D). No significant heterogeneity was found among these reports (I2 = 0%).
Clinical response to HIFU
All studies reported data on clinical response to HIFU. We found HIFU ablation to be associated with an 80% pooled clinical response rate (Figure 3 E). These reports showed no significant heterogeneity (I2 = 0%).
Complications
Two studies reported data on the rates of cholangitis and pancreatitis [14, 15]. The pooled cholangitis rates were comparable between the 2 groups (16.1% vs. 12.5%, p = 0.47, Figure 3 F), with no significant heterogeneity observed between the studies (I2 = 0%). The pooled pancreatitis rates were comparable between the 2 groups (1.1% vs. 2.5%, p = 0.56, Figure 3 G), again with no significant between-study heterogeneity (I2 = 0%).
Discussion
Here, we assessed the clinical efficacy of biliary stenting with HIFU ablation in patients with distal MBO caused by PC. The results indicated that the patients’ stent dysfunction, stent patency duration, and OS were significantly improved by the HIFU ablation.
Initially, we observed similar pooled ΔTBIL values between the 2 groups, indicating that HIFU ablation does not influence the short-term effectiveness of biliary stenting.
Biliary stents have previously been reported to be associated with 50% cumulative 6-month re-obstruction rates [18]. While some studies have found that covered stents have longer patency in distal MBO patients than uncovered stents [6, 9], these covered stents do not slow the cancer progression. Covered stent insertion has also been related to higher rates of cholecystitis and pancreatitis in treated patients [6, 7].
Here, the stent patency function was assessed by calculating the rate of stent dysfunction and the duration of stent patency. We found that both the pooled stent dysfunction rate (p = 0.03) and the stent patency duration (p < 0.0001) were favourable in the stenting with HIFU group. These results indicate that HIFU ablation can effectively halt tumour progression and prolong stent patency. However, in these included studies, although the stent dysfunction rates were lower in the stenting with HIFU group, this difference was not significant [11–15]. When these rates were pooled by the meta-analysis, the statistical power was increased and the difference became significant.
All the included studies used 8 mm diameter metal stents [11–15]. Metal stents appear to be superior to plastic in achieving long-term patency duration [3]. Several studies have used 10 mm stents for MBO patients [19, 20]; however, a recent report showed comparable stent patency, survival duration, and complication rates for 8 mm and 10 mm stents in MBO [21].
We found significantly longer pooled OS rates for patients receiving stenting with HIFU ablation compared to stenting alone. This is consistent with prior studies that have found that anticancer treatment can prolong survival in patients who have undergone stent insertion [8, 9, 22]. HIFU ablation can improve stent patency and OS in patients with distal MBO caused by PC because PC is a mass-like tumour. In contrast to distal MBO caused by the lumen-like cholangiocarcinoma, PC can be treated using specialized equipment to focus the ultrasound energy on a specific target within the body, thereby driving thermally induced apoptosis and necrosis [23]. We also determined that HIFU ablation was associated with an 80% pooled clinical response rate. This finding, together with the OS-related results, suggests that HIFU ablation may be well-suited to the treatment of distal MBO caused by PC.
No differences in cholangitis and pancreatitis rates were detected between the 2 patient groups, suggesting that HIFU ablation is not associated with an increased complication rate. However, only 2 of the included studies included data on cholangitis and pancreatitis rates, indicating the necessity of further studies to confirm these results.
The study has several limitations. Firstly, the retrospective nature of many of the included studies may introduce bias. Second, although this meta-analysis only included the studies that focused on distal MBO caused by PC, several studies did not provide the details of the tumour stage and the Eastern Cooperative Oncology Group performance status, which may increase bias risk. Third, the included studies were all conducted in China. These results, therefore, need to be verified in other populations.