Introduction
Calprotectin is a leukocyte protein of the S100 family found in the granulocytes and neutrophil cytosol, as well as in monocytes and activated macrophages. Released into the extracellular space, calprotectin induces migration of neutrophils to the inflammatory lesion and stimulates their phagocytic activity. Moreover, due to its ability to inhibit zinc-dependent bacterial metalloproteinases, calprotectin prevents the growth of bacteria within the intestinal lumen and their adhesion to the intestinal epithelium. The protein also has the ability to induce apoptosis, both in normal and cancerous cells [1, 2].
Calprotectin belongs to the group of acute phase reactant proteins, which means that inflammation leads to its significant increase in the blood serum, other body fluids, and in the stool. Therefore, calprotectin has been used as a marker of inflammatory processes in the gastrointestinal tract, such as inflammatory bowel disease (IBD). The concentration of faecal calprotectin (FC) is much higher than in the blood serum [3–7]. That is why FC-labelled immunoenzymatic methods are used as a cheap and rapid test to assess IBD activity. It also serves as a marker of mucosal healing (MH) and disease recurrence [8–13].
However, despite the increasing incidence of IBD in paediatric patients, data on the diagnostic value of FC in this group are still limited. FC concentrations > 50 µg/g are considered to be associated with increased intestinal permeability [14, 15]. One study has shown that this cut-off point has 100% sensitivity and 67% specificity in detecting IBD in paediatric patients [16].
A good correlation between FC and clinical markers of IBD activity has also been demonstrated [17, 18].
However, there are still too few data on the correlation between FC and MH in paediatric patients with IBD. Our preliminary results show that the cut-off point for FC, which can be used as a marker of MH in this group, was 233 µg/g. However, this study included a relatively small group of patients (n = 46), and there were patients with both Crohn’s disease (CD) and ulcerative colitis (UC) [19]. Therefore, we decided to perform the study to assess the value of FC as a marker of MH on a larger and more homogenous group (only UC patients).
Aim
The main goal of this study was to assess the correlation between FC and endoscopic activity of inflammation in paediatric UC patients. The secondary aims were as following:
Material and methods
This retrospective study included 81 patients with UC with a median age of 15 years (range: 3–18 years) who had been treated in the Children’s Memorial Health Institute (CMHI) in the period between 2013 and 2015. There were 43 (53%) girls and 38 (47%) boys. Mean age of diagnosis was 12 years. The majority of patients (93%) had been treated with 5-ASA, 65% of them had a medical history of steroid treatment, and 12% needed biological therapy. The most common disease location was the distal part of the large intestine (42%), and the majority of patients had a mild course of their disease. Both groups (Baron score 0 vs. ≥ 1) were demographically and medically comparable.
Table I presents patients’ detailed characteristics.
Table I
Demographic, anthropometric, and clinical characteristics of the study participants
The study protocol was approved by the Local Bioethical Committee of the CMHI, and the children’s caregivers gave informed written consent for their participation in the project.
The level of FC was measured using the Buhlmann Quantum Blue Calprotectin immunoenzymatic test according to the manufacturer’s instructions. In addition, elective endoscopic examination of the lower gastrointestinal tract was performed in all patients within 7 days of admission to the hospital.
The activity of the large intestine mucosal inflammation was assessed using the Baron scale. Based on the endoscopic examination two subgroups of patients were created: patients with Baron score 0 and patients with Baron score ≥ 1 point. The following parameters were determined and compared between the groups: FC levels, demographic characteristics (gender, age at the time of the study), and anthropometric (height and body mass, BMI), clinical (age at diagnosis of UC, past and current medications, disease activity according to PUCAI score, disease severity according to the Paris scale), and laboratory (C-reactive protein concentration, ESR, haematocrit, platelet count) parameters (Tables I and II).
Table II
Values of selected laboratory parameters in the study participants
Statistical analysis
The normality of the distribution of continuous variables was assessed using the Kolmogorov-Smirnov test. Statistical characteristics of continuous variables are presented as arithmetic means and standard deviations (SD) or median and quartiles. Depending on the type of distribution, Student’s t test or Mann-Whitney U test were used for comparisons of intergroup statistical characteristics of continuous variables. Statistical characteristics of step and quality variables were presented as numerical and percentage distributions, which were compared between groups using the Pearson χ2 test or Fisher’s exact test.
Variables whose values differed significantly between the compared groups were analysed by ROC. For each of these variables, the area under the ROC curve (AUC) was calculated with its 95% confidence interval (95% CI); cut-off points were determined to be optimal in differentiating between patients with Baron scores 0 and ≥ 1 points with their sensitivity and specificity.
A two-dimensional logistic regression analysis was used to calculate the expected values in order to determine the overall diagnostic validity of the identified variables. The AUC values for the various parameters and their combinations were compared using the Z-test. The results of the ROC analysis were verified using the discriminant analysis method.
Moreover, Spearman’s (R) rank correlation coefficients were calculated between FC and the other identified markers of MH. All calculations were made using the Statistica 10 software (StatSoft, USA) and the value of p ≤ 0.05 was established as a significance level.
Results
In the study group there were 34 (42%) and 47 (58%) patients with Baron scores = 0 and ≥ 1, respectively. Table I presents patients’ detailed characteristics.
In patients with Baron score ≥ 1 significantly higher FC levels and PUCAI scores were found in comparison to the patients with Baron score 0. Moreover, there was close statistical significance of the intergroup difference in terms of BMI (Tables I and II). Therefore, these three variables were included in the ROC analysis. Table III presents these results. Because the cut-off point for BMI in the ROC analysis had zero-sensitivity, this parameter was not included in the subsequent analyses.
Table III
Results of ROC analysis for predictors of mucosal healing in UC patients
The comparison of areas under the ROC curve showed better accuracy of FC (than the PUCAI score) in differentiation between patients with Baron score 0 and ≥ 1 (Z = –1.73, p = 0.082). Inclusion of PUCAI score in the analysis did not significantly increase FC accuracy as a marker of MH (Z = 0.15, p = 0.881) (Figure 1).
Figure 1
ROC curve for faecal calprotectin ≤ 105 μg/g and PUCAI score ≤ 7.5 points as predictors of mucosal healing in ulcerative colitis patients
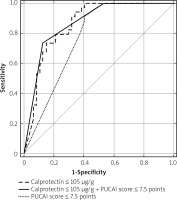
Discriminant analysis demonstrated that only FC had significant value in selecting patients with more severe endoscopic disease activity (FC: F (1.78) = 6.98, p = 0.010; PUCAI scale F (1.78) = 2.01, p = 0.161).
A significant correlation between PUCAI score and FC (R = 0.55, p < 0.001) was found.
Discussion
Recently, FC as a noninvasive marker of intestinal permeability has been used to assess and monitor disease activity, MH, and reccurence of the disease in patients with IBD [1–3].
However, data on the correlation between FC and MH in paediatric IBD are still limited.
Levels > 50 µg/g are considered to be associated with increased intestinal permeability, but the cut-off point for MH has not been established yet, although certain studies on that issue have been performed [14, 15, 19]. Our preliminary results have demonstrated that the cut-off point for FC, which can be used as a marker of MH in the paediatric IBD group, was 233 µg/g [19]. However, almost half of the participants in this pilot study (22/46 patients) were patients with CD.
According to some authors, UC and CD may differ when it comes to the FC level, and this marker seems to be more accurate in assessing UC activity [9]. Moreover, different diagnostic criteria of MH are used in these two disease entities (Baron vs. SES-CD scale; UC vs. CD, respectively).
Results from this study are more reliable due to the greater number and homogeneity of the study group (only UC patients).
In the literature, cut-off points for FC as a marker of MH in IBD patients differ significantly: from 50 µg/g to 250 µg/g, with sensitivity and specificity comparable to those in our study [20–24].
In the study by Ricciuto et al. performed on a paediatric population with IBD-PSC, the cut-off point associated with MH was 93 µg/g [25]. While in the study by Walsh et al., which included only UC patients, as in our study, the level of FC ≥ 72 µg/g indicated histological inflammation and ≥ 187 µg/g indicated endoscopically active disease [26]. Hart et al. demonstrated in their study on a large UC cohort (185 patients) that FC ≥ 170 µg/g predicted endoscopic activity and FC ≥ 135 µg/g predicted histological activity [27]. These levels are significantly lower than in our study. However, we should take into consideration differences in the study population (UC vs. UC-IBD in the Ricciuto study) and methods used to determine FC concentration, which may have influenced the results.
In our study, the PUCAI score was another, clinical marker of MH. Nonetheless, FC showed better accuracy in identifying endoscopic disease activity. These results are consistent with previously published studies demonstrating significant correlation between PUCAI score and MH [28].
Our findings demonstrating a correlation between PUCAI score and FC are also consistent with other published reports. These data have confirmed the great value of FC as a marker of disease activity [17, 18].
However, total assessment of both PUCAI score and FC did not significantly increase the specificity of FC as a marker of MH, which is consistent with data published by Schroder et al. [29]. The authors also demonstrated that inclusion of other inflammatory parameters did not significantly increase the specificity of FC as a MH marker.
Since FC correlates with increased intestinal permeability, not with a specific disease entity; its concentration may be elevated also in other gastrointestinal diseases, which may potentially be the limitation of FC as a marker of IBD activity. So far, elevated concentrations of FC have been found in large intestine carcinoma, in patients taking non-steroid anti-inflammatory drugs (NAID), and during steroid-therapy [5, 30, 31]. Nonetheless, Henderson et al. in their study assessing diagnostic accuracy of FC during investigation of suspected paediatric IBD demonstrated that there were much higher FC concentrations in children with IBD than in the control group [32].
Our study has certain limitations. First, all study patients were treated in one, referral, tertiary Hospital, and therefore our results may not be representative for the whole paediatric UC population. Also, the study group, although quite numerous for a paediatric population, is still not big enough and does not have good statistical power. Another important issue is the identification of the most optimal cut-off point for FC as MH marker; whether maximal AUC or the value with 100% specificity should be used to establish it. The first one is consistent with the ROC analysis approach and has been used as a method in all studies. However, from the clinical point of view the optimal marker of MH should identify patients who may not need endoscopic examination to verify complete remission. Therefore, the cut-off point with the highest specificity should be used.
Nonetheless, even with these limitations, our study confirmed that FC may be used as an isolated marker of both MH and disease activity in children with UC.
To sum up, the majority of our results (significant correlation between FC and clinical and endoscopic remission, inclusion of other inflammatory parameters did not significantly increase the specificity of FC as a MH marker) are consistent with data published by other authors. However, the cut-off point of FC indicating MH is significantly different in each study – in our study it is higher than in other authors findings.
Therefore, further studies on this issue should be performed.
Conclusions
Our study has provided more evidence that FC is an important marker of UC activity in paediatric patients. In particular, we have demonstrated the following:
–FC ≤ 105 µg/g is a marker of MH, characterised by 74% sensitivity and 85% specificity;
–using this cut-off point, the diagnostic validity of FC as a marker of MH is slightly higher than the diagnostic accuracy of the PUCAI score;
–FC correlates with clinical activity of UC based on the PUCAI score;
–the accuracy of FC as a marker of MH does not increase when this parameter is assessed together with the PUCAI score.










