Introduction
Appendicitis represents a prevalent surgical emergency globally, posing a significant risk of severe complications. These complications encompass a spectrum of conditions, including ileus, peritonitis, abscess formation, and, in extreme cases, mortality [1]. Furthermore, the management of appendicitis imposes a substantial burden on healthcare systems worldwide [2]. The annual incidence of appendicitis is approximately 233 cases per 100,000 individuals, with a lifetime risk ranging from 6.7% to 8.6% [3]. While Western nations experienced a decline in appendicitis incidence during the mid-twentieth century, newly industrialized countries have witnessed a rising trend in the twenty-first century [4, 5].
Additionally, there is substantial variability in the presentation, severity, radiological evaluation, and surgical approach to patients with acute appendicitis, which is often linked to the economic status of the country [6]. The perforation rate of appendicitis ranges from 16% to 40%, with a lower incidence observed in younger age groups (40–57%) and individuals older than 50 (55–70%) [7].
The clinical diagnosis of acute appendicitis presents significant challenges and requires a comprehensive assessment of clinical, laboratory, and radiological findings. The diagnostic process could be enhanced by using clinical scoring systems that incorporate physical examination findings and inflammatory markers [8]. Numerous simple and user-friendly scoring systems have been employed as structured algorithms to predict the risk of acute appendicitis; however, no single system has achieved widespread acceptance [9]. The role of diagnostic imaging modalities, such as ultrasound (US), computed tomography (CT), or magnetic resonance imaging (MRI), plays a key role [10].
Current evidence supports laparoscopic appendectomy (LA) as the most effective surgical treatment, demonstrating a lower incidence of wound infection, reduced postoperative morbidity, shorter hospital stays, and improved quality of life scores compared to open appendectomy (OA) [11]. The most common postoperative complications, including wound infection, intraabdominal abscess, and ileus, exhibit varying frequencies between OA and LA, with an overall complication rate of 11.1% for OA and 8.7% for LA [12].
The clinical presentation of acute appendicitis is influenced by various factors, including patient age, symptom duration, and anatomical variations in appendiceal position [13].
The classic presentation of appendicitis in adults involves migratory right iliac fossa pain, anorexia, nausea with or without emesis, fever, and localized muscular rigidity or generalized guarding [14, 15]. The classic symptom progression of appendicitis involves initial vague periumbilical pain followed by anorexia, nausea, and intermittent vomiting, subsequently migrating to right lower quadrant pain, and culminating in low-grade fever [16].
Historically, the Alvarado score and its modified version have been the most prominent scoring systems in this context. While these systems were developed in Western populations, their application to other populations, particularly those in Asia, has demonstrated reduced sensitivity and specificity [17]. To stratify the risk of acute appendicitis among Asian populations, the Raja Isteri Pengiran Anak Saleha Appendicitis (RIPASA) score system, developed in Brunei Darussalam in 2008, has demonstrated significant utility [18]. The RIPASA grading system comprises parameters that sum to a total score of 17.5. This system requires only two routine investigations (white blood cell count and urine analysis), which are readily available, yielding results with a high negative predictive value. This has the potential to reduce healthcare costs by decreasing the rate of unnecessary appendectomies [19].
Aim
The present study aimed to assess the association of existing risk scores for the diagnosis of acute appendicitis, and patient characteristics with the diagnosis of acute appendicitis, the odds of operative vs. non-operative management, and postoperative outcomes.
Material and methods
A retrospective analysis of patients presenting with right lower quadrant (RLQ) pain was conducted at a single tertiary surgical center in Greece between 2020 and 2023. Baseline demographic data, including age, sex, comorbidities, and presenting symptoms, were systematically collected to characterize the study population. This study aimed to identify factors associated with the diagnosis of appendicitis versus other types of abdominal pathology and assess the association of risk scores with operative management and postoperative complications. A comprehensive statistical analysis was conducted to assess the significance of various clinical and laboratory parameters. All consecutive, adult patients presenting with RLQ pain assessed for possible acute appendicitis were included in the analysis. Pregnant women are excluded from the present study due to differences in clinical examination techniques and restrictions in imaging as well as ultimate treatment approaches. Therefore, those with a positive pregnancy test were removed from the dataset. The data set initially contained 150 patients, and it was found that 41 of them were pregnant. Therefore, 109 patients remained in the dataset.
Statistical analysis
Statistical analyses were performed using R software (version 4.3.2). Continuous variables were summarized using means and standard deviations (SD) or medians and interquartile ranges (IQR) based on their distribution, which was assessed using the Shapiro-Wilk test. Categorical variables were summarized using frequencies and percentages. Group comparisons were made using the χ2 test or Fisher’s exact test for categorical variables, and the Wilcoxon rank-sum test for non-normally distributed continuous variables. Risk ratios (RR) and odds ratios (OR) with 95% confidence intervals (CI) were calculated to assess associations between variables. Data were visualized using density plots and boxplots. A significance level of p < 0.05 was used throughout the analysis.
Results
In total, 109 patients assessed for acute appendicitis were included in this study. The baseline patient characteristics as well as the studied parameters at the time of diagnosis can be summarized in Table I.
Table I
Baseline characteristics of patients by diagnosis
Diagnosis of acute appendicitis
Sex (p = 0.99, OR = 1.01, 95% CI: 0.87–1.17) and age (p = 0.23, OR = 1.01, 95% CI: 0.98–1.04) were not found to be significantly associated with the diagnosis of appendicitis.
Patients with radiating pain were significantly less likely to be diagnosed with appendicitis compared to those with localized pain (p = 4.05 × 10–6, RR = 0.0918, 95% CI: 0.039–0.217). The duration of symptoms did not significantly influence the diagnosis (p = 0.12, RR = 1.04, 95% CI: 0.98–1.11).
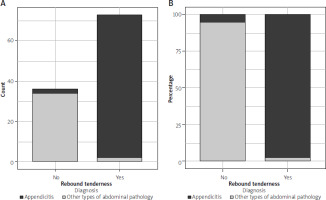
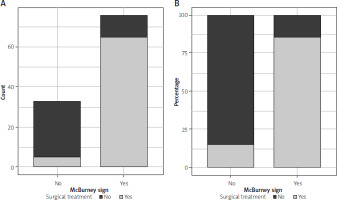
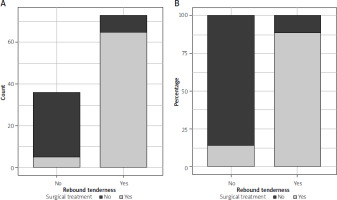
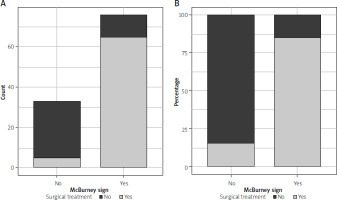
Patients with rebound tenderness (Figure 1), McBurney’s sign (Figure 2), and Rovsing’s sign were much more likely to be diagnosed with appendicitis compared to those without these findings (p < 0.01 for all).
Patients with white blood cells (WBC) levels above 10,000/ml were less likely to have appendicitis compared to those with WBC levels below 10,000/ml (p = 0.0063, RR = 0.45, 95% CI: 0.23–0.88). Similarly, patients with C-reactive protein (CRP) levels above 0.7 mg/dl were less likely to have appendicitis compared to those with CRP levels below 0.7 mg/dl (p = 0.0017, RR = 0.41, 95% CI: 0.20–0.85). Procalcitonin (PCT), amylase, and TKE levels were not significantly associated with the diagnosis of appendicitis.
CT findings, such as direct or indirect signs of appendiceal inflammation, were strongly associated with appendicitis (p = 4.4 × 10–5). However, due to data imbalance, odds and risk ratios were difficult to interpret.
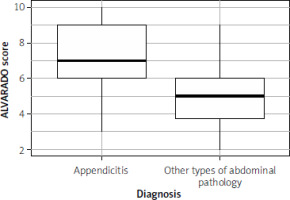
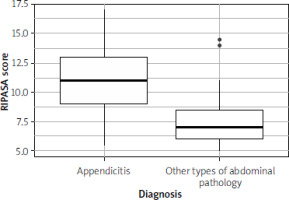
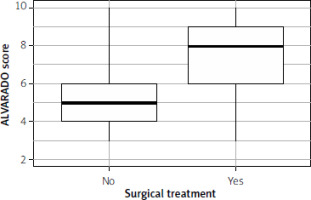
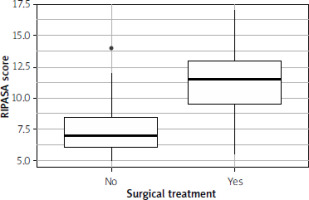
The ALVARADO score (p = 9.02 × 10–10) (Figure 3) and the RIPASA score (Figure 4) (p = 1.05 × 10–10) were significantly higher in patients with appendicitis.
Differences in the management of acute appendicitis
Within the scope of this study, we investigated whether patient-level characteristics, biochemical markers, and risk scores were correlated with the decision to undergo surgical treatment, in favor of conservative management. An overview of the parameters studied and their differences between conservatively and surgically treated patients can be seen in Table II.
Table II
Univariable associations of patient factors and operative vs. non-operative management
In contrast, patients with radiating and generalized pain had much higher odds of being managed surgically, compared to patients with localized pain (OR = 59.6), an association also observed with rebound tenderness, which was an independent predictor of patients having appendicectomy as opposed to conservative management (OR = 50.37) (Figure 5). Pyrexia was also significantly associated with operative management, with an OR of 3.66 for patients with a temperature of more than 37.3°C.
Clinical signs elicited in patients were also significant predictors of operative management in the univariable association analysis; McBurney’s sign-positive patients had an odds ratio of 33.09 to receive an operation (Figure 6), and patients with a positive Rovsing sign had 41.14 times higher odds of undergoing operative management.
There were statistically significant correlations between traditional inflammatory markers and odds of undergoing operative management; Patients with a WBC of more than 10 × 103 had 3.05 times higher odds of undergoing an appendicectomy. A similar association can be seen with PCT (OR of 6.65 for elevated levels) and CRP (OR of 2.74 for CRP > 0.7 mg/dl). Amylase and TKE were not significantly associated with operative treatment approaches.
Increased ALVARADO scores were significantly associated with operative treatment, with patients receiving an appendicectomy having a mean score of 7.56 (SD = 1.91) and patients undergoing conservative management having a mean score of 4.92 (SD = 1.56) (p-value < 0.001) (Figure 7).
The same observation can be made for the RIPASA score (Figure 8), with patients receiving an appendicectomy, having significantly higher mean scores (11.32 vs. 7.48, p-value < 0.001).
Outcomes following management of acute appendicitis
Baseline patient characteristics, duration of pain before presentation, and pain localization were not significantly associated with the occurrence of postoperative complications. Pyrexia, migrating pain, and rebound tenderness as clinical signs were also not significantly correlated with postoperative complications following appendicectomy.
Similarly, clinical signs including McBurney’s and Rovsing’s signs revealed no statistically significant association with the development of postoperative complications.
Baseline risk scores at presentation were also non-significantly associated with developing complications following either appendicectomy or conservative management of the underlying diagnosis. The mean RIPASA score for patients with uneventful recovery was 9.89 (SD = 3.1), while patients with complications had a mean score of 11.5 (SD = 5.26); the difference in means, however, was not statistically significant (p = 0.52).
Similarly, the baseline ALVARADO score was not significantly different between patients with complicated recovery and patients with an uneventful disease course. Patients with immediate recovery had a mean score of 6.62 (SD = 2.17) and patients with postoperative complications had a mean score of 6.5 (SD = 3.11). Of note, the sample size in the complicated group of patients was small (n = 5); therefore, the comparisons are difficult to interpret accurately and require further validation.
Discussion
The present study is a retrospective analysis of patients presenting with RLQ pain in a tertiary hospital in Greece, aiming to delineate the role of baseline prediction scores for acute appendicitis, supplemented by patient factors, clinical signs, and commonly used inflammatory biomarkers. Our study investigates the utility of each factor in predicting the diagnosis of acute appendicitis before imaging or exploratory laparoscopy as well as their association with the decision to operate or not, and their correlation with complications following operative or conservative management. Post-operative intra-abdominal abscess (PIAA) is the most serious complication after appendectomy and, despite its low incidence, is responsible for the majority of reported deaths after appendectomy [20–22].
The ALVARADO and RIPASA scores were both found to be significantly positively associated with the diagnosis of acute appendicitis, with patients with acute appendicitis having on average an increase of 2 and 2.8 points in these scores, respectively. Our findings are in line with the existing literature and validation studies of these scores [4, 12, 15] and confirm their role in non-invasive, baseline risk stratification of patients presenting in the emergency department with lower abdominal pain, often non-specific. The ALVARADO score has some shortcomings in prior studies on the prediction of acute appendicitis [5, 8, 13] as it may be less predictive in children, the elderly, and pregnant patients, where clinical presentation can differ from typical cases. In cases of intermediate scores or atypical presentations, imaging studies or complementary scoring systems, such as the Appendicitis Inflammatory Response (AIR) score, are often used to improve diagnostic accuracy.
Unlike the Alvarado score, the RIPASA score is more complex and includes additional parameters, which can make it more time-consuming to calculate. This complexity may reduce its practicality, especially in fast-paced emergency settings where simplicity and speed are critical. Some critics argue that while the score’s comprehensiveness is beneficial, the increased number of criteria may not always yield a proportionate improvement in diagnostic accuracy over simpler scoring systems. Although the RIPASA score generally demonstrates high sensitivity, its specificity has been criticized as being lower than desired in some studies. Lower specificity means a higher chance of false positives, which can lead to unnecessary surgical interventions. This is particularly concerning in populations with low overall appendicitis prevalence. In certain studies, the false-positive rate was found to be higher compared to other scoring systems, which could result in over-diagnosis and increase the number of negative appendectomies. As of the time of conducting this study, there is no consensus regarding the use of the RIPASA score, and its usefulness compared to the ALVARADO score.
One of the most important aspects of risk score assessment is to investigate the change in practice or change in decision-making. Although our study did not capture changes in surgeon decisions based on risk estimation, both clinical risk scores are significantly associated with patients undergoing operative in favor of non-operative management, as exhibited in our study population. Pain localization, diagnostic signs of acute appendicitis, peritonism, and pyrexia are all additional patient factors that were positively correlated with the decision to operate rather than manage conservatively. Many of the patient factors studied are part of clinical risk prediction scores; therefore, their weight in the context of decision-making can be assessed here.
Increased risk scores have been studied in relation to disease severity and potential prediction of complicated appendicitis with higher scores than uncomplicated appendicitis. Within our study, both the ALVARADO and RIPASA scores exhibited a positive correlation with complicated outcomes following the management of these patients, not reaching statistical or clinical significance levels. One of the shortcomings of the present study was the very small number of individuals with complicated post-management outcomes, which potentially prevented the detection of significant correlations between increased risk scores at presentation and higher odds of complicated outcomes.
Conclusions
The results of this study highlight the importance of clinical presentation, physical examination findings, and specific laboratory markers in the diagnosis of appendicitis. While demographic factors and certain biomarkers did not show significant associations, the combination of clinical and laboratory data can aid in accurate diagnosis and timely intervention.