Introduction
Childhood obesity is defined medically as body mass index (BMI) at or above the 95th percentile for age and sex, while childhood overweight is BMI between the 85th and 95th percentile for age and sex [1]. It is associated with an increase in body weight, more specifically fat tissue mass [2]. It occurs when energy intake is more than energy expenditure and is associated with increased fat cells size and number [2]. The sharp increase in the prevalence of overweight and obesity among children reflects a critical shift toward positive energy balance. Consequently, this upsurge is posing a major health threat worldwide. Risk factors for childhood obesity include modifiable and non-modifiable factors [2]. Non-modifiable factors such as genetics, hormonal disturbances, certain diseases, and medications [2]. Modifiable factors such as environmental and socioeconomic factors. There are many risk factors contributing to obesity in children, and the most important modifiable factors are poor diet, adverse dietary habits, and lack of physical activity [3, 4].
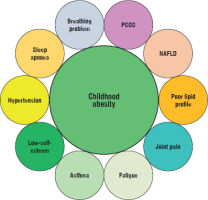
Children who are overweight at age 5 are 4 times more likely than their normal-weight peers to become obese later in childhood [5]. Obesity predisposes children to obesity-related health consequences such as type 2 diabetes, hypertension, metabolic syndrome, non-alcoholic fatty liver disease (NAFLD), and polycystic ovary syndrome [2]. It also leads to depression, low self-esteem, social discomfort, and ultimately social isolation [6], and as a result, the quality of life among obese children decreases significantly (Fig. 1). Obesity during adulthood can be partially explained by a decrease in metabolic rate. Thus, when people maintain a sedentary way of living, their energy output will decrease over time, and this causes weight gain [7]. A dramatic change in a child’s behaviour and environment towards sedentary lifestyle in modern societies may explain the sharp increase in the prevalence of childhood obesity worldwide [3]. Feeding behaviours are manipulated by mothers at an early stage of the child’s life [8, 9].
Figure 1
Common health risks associated with childhood obesity. Risks may include polycystic ovary syndrome (PCOS), non-alcoholic fatty liver disease (NAFLD), poor lipid profile, joint pain, fatigue, asthma, low-self-esteem, hypertension, sleep apnoea, and breathing problems
Risk factors for childhood obesity can help identify individuals at risk [2]. However, these factors are insufficient to explain the sharp increase in childhood obesity in Europe and developed countries, which occurred 3 to 5 decades ago [10]. This is because the westernised lifestyle and daily increase in high-caloric, high-fat diets started around the 1950s. Furthermore, the sharp increase in overweight and obesity also cannot be blamed on the availability of fast food either because it has already been presented during the 1950s and 1960s. Thus, even when all known causes of obesity have been taken into consideration, they do not provide a satisfactory explanation for such an increase in the prevalence of overweight and obesity among children worldwide. Although previous studies attempted to link children’s diets with the growing prevalence of obesity, none have been able to show a fundamental link between diet and child obesity [11, 12]. Underreporting of daily caloric intake and overreporting physical activity, which is something that normally occurs in childhood obesity studies, may deviate the results [13]. Another important factor that may explain the sharp increase in childhood obesity is a significant alteration in children’s behaviour [13].
One of the major challenges in the life of today’s children is linked to their parents [14]. Parents no longer spend as much time (as they used to do) with their children. The availability of one or both parents around the child has a positive impact on a child’s behaviour because it makes it easy for them to advise the child on what is good or bad [15, 16]. For example, when both parents work full time, there is rarely enough time to give the child the right direction. Parents try to compensate for the lack of attention by offering more food, more games, or more money, which will ultimately worsen the issue instead of solving it. Understanding how children’s behaviours affect childhood obesity can provide an opportunity to focus resources, interventions, and research in the direction that would be most beneficial in addressing the problem. This review discusses factors that influence child behaviour and the relationship between child behaviour and childhood obesity.
Size of the problem
Childhood obesity has witnessed a sharp increase in developed and many developing countries [2]. Globally, the mean standardised BMI has been increased by 0.32 kg/m2 per decade [1]. Multiple factors contribute to this increase, including genetic, environmental, and socioeconomic factors [2–4]. Nevertheless, well-known risk factors are not the only culprits for the growing prevalence of childhood obesity, but rather what controls child behaviour to be under the exposure to such risk factors. Thus, addressing childhood obesity requires a comprehensive approach that addresses not only biological and environmental factors but also behavioural factors influencing children’s eating habits, physical activity levels, sleep patterns, and emotional well-being. As a result, effective strategies for preventing and managing childhood obesity require a comprehensive, multi-sectoral approach that addresses individual, family, community, and educational institutes.
Children’s behaviour plays a significant role in the epidemic of obesity [14–16]. Compared to children with normal weight, obese children are at risk for developing certain health conditions such as poor lipid profile, NAFLD, asthma, sleep apnoea, bone, and joint problems (Fig. 1). Other chronic health consequences that an individual may face during young adulthood include type 2 diabetes, atherosclerosis, and cardiovascular diseases, which can develop with a longer period of exposure to obesity. More importantly, obesity seems to ‘track’ from adolescence to adulthood [17]; thus, early intervention to manage and prevent overweight and obesity at younger ages is a high priority from a public health point of view. Obesity in general, and abdominal obesity specifically, is strongly associated with insulin resistance. Insulin resistance is a key factor in the development of type 2 diabetes and is also associated with other metabolic abnormalities, including dyslipidaemia, hypertension, and polycystic ovary syndrome [18].
What controls child behaviour?
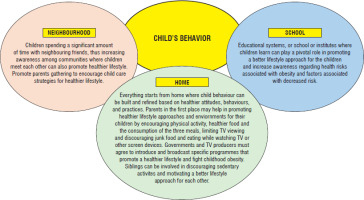
A child’s behaviour is a way of communicating their genuine needs, desires, and feelings. Generally, there are many factors contributing to that behaviour, including age, personality, and the environment [19, 20]. During childhood, behaviour can be considered normal or problematic depending on whether it matches the outline expectations of the family, society, and religion and/or certain beliefs. Nevertheless, providing healthy lifestyle environments for children and adolescents is crucial [20–22]. The significant increase in the prevalence of childhood obesity in the last 3 decades could be due to alterations in child behaviour [23]. Child behaviour can be influenced mainly by 3 essential factors, and these are homes where parents play a major role, school, and neighbourhood (Fig. 2).
The role of parents
A child’s behaviour, development, and growth are embedded within a multifaceted system of relationships. Among the most important relationships that influence children’s behaviour is the one that exists between the parents and child [24]. Parents are children’s first guide to help them build healthy behaviours. A child’s behaviour at home can be promoted by one or both parents. The impact of parents on a child’s behaviour is highly important because it may promote or prevent childhood obesity [22, 23, 25]. Thus, acknowledgement of the crucial importance of early parent-child relationship quality for children’s socioemotional, intellectual, neurobiological, and better health outcomes has contributed to a shift in efforts to identify relational determinants of child outcomes [24].
Before the birth of an infant, there are important roles that mothers can take part in to prevent the unborn child becoming obese later on [26]. Obese parents tend to have obese children [26, 27]. A child has a 3.68-fold increase in the risk of obesity if his/her mother has BMI >30 kg/m2 [27]. Previous [28, 29] and most recent available studies [30] have shown that the mother’s weight gain during pregnancy is associated with increased birth weight. Furthermore, overweight and obese mothers who have gained weight before and throughout pregnancy are at high risk of metabolic syndrome, type 2 diabetes mellitus, and gestational diabetes [29, 31, 32]. Compared with normal-weight women, pre-pregnancy body mass index and gestational weight gain are associated with greater maternal and infant complications [29, 31, 32]. Weight gain and overeating during pregnancy places mothers and their children at an increased risk for obesity [27, 29–33]. Mothers also play important roles after a child’s birth. Indeed, what children eat is directly dependent on the knowledge, perceptions, and practices of their parents and other caregivers [34]. The method that mothers choose to feed the child is important. Previous studies show that breastfeeding is associated with a protective trend against child obesity [35–38]. In contrast, using infant formula is associated with increased risk of overweight and obesity [39–42]. Mothers in westernised countries are less likely to breastfeed their children than they were 5 decades ago [43].
Parents are responsible for helping their children develop healthy habits, such as healthy sleep, the consumption of healthy food, and eating breakfast and other main daily meals on time. Poor sleep is associated with higher BMI among children compared with children with normal sleep duration (8 to 9 hours per day) [44–46]. Others reported that sleep timing behaviour is also associated with higher BMI [47–49]. A previous study [48] found that late bedtimes and late wake-up times are associated with poorer diet quality (dense caloric and poor nutrition value diet). Furthermore, bedtime was found to be associated with breakfast partaking. Thus, bedtime was significantly earlier in children consuming breakfast every day (08:30 vs. 09:00 PM, p < 0.01); and was later (09:15 vs. 09:30 PM) in children who went to bed late and snacked rather than eat breakfast [49].
Other important factors that have a crucial impact on child behaviour and weight gain include parental relationship, their education level, their maternal status, and whether they are employed [50–52], as shown in Table I. A previous study [50] showed that, compared with children and adolescents whose mothers stay at home, those with employed mothers have a 2.6-fold increase in the risk of being obese (OR = 2.60 [95% Cl: 1.18–5.70]). Parental education level may also affect child weight in 2 different directions. In developed and industrial countries, the parental educational level is mostly associated with decreased risk of overweight and obesity [53]. In contrast, in developing and less developed countries, parental educational level is considered as a risk factor for overweight and obesity in children [51]. This could be because higher education is associated with increased purchasing power, which correlates with more food on the table. In low- and middle-income countries, childhood obesity is predominantly a problem of the rich [52].
Table I
The Association between selected socioeconomic variables and childhood obesity
| Authors, year, country | Targeted variable | Outcome |
|---|---|---|
| Mekonnen et al. 2022 [58] Norway | Parents’ education | Children of low-educated parents had a higher risk of overweight and obesity at 5, 8, and 14 years compared to children of high-educated parents. |
| Börnhorst et al. 2023 [59] EUROPEAN COHORT | Parents’ education | Significant differences in childhood overweight and obesity risk factors are due to differences in educational level of parents |
| Nasreddine et al. 2014 [50] Lebanon | Parents’ education | Compared with low education, mothers and fathers with higher education have 2.12 (0.5–8.85) and 2.20 (0.56–8.64) risk increase of childhood obesity, respectively |
| Ding et al. 2021 [53] China | Father’s education | Compared with the lowest education level (primary school or less), the ORs for fathers who had completed junior high school, senior high school and junior college or higher provide 0.77 (95% CI: 0.64–0.92) and 0.72 (95% CI: 0.55–0.93) protection, respectively |
| Reis et al. 2020 [60] USA | Parents’ income | Children of low-income parents were twice as likely to have increased BMI scores compared to children from higher income families |
| Nasreddine et al. 2014 Lebanon [50] | Working mother | Compared with not-working, working mothers associated with 2.60 [1.18–5.70] risk increase of childhood obesity |
| Biehl et al. 2014 [56] Norway | Divorced parents | Overweight and obesity is 54% more prevalent among school’s children of divorced parents compared with children of married parents (RR = 1.54 [95% CI: 1.21–1.95]) |
| Di Maglie et al. 2022 [61] Italy | Physical activity | There was a significant decrease in BMI (−2.4 ±0.6 kg/m2) in the intervention group compared to control group (3.01 ±1.8 kg/m2) |
| Mitchell et al. 2017 [62] USA | Physical activity | Physical activity was independently associated significantly with lower body mass index (BMI) and waist circumference (WC) in children and adolescents |
Childhood obesity can also be triggered by parental obesity [2]. Previous studies found that the odds of being an obese child is 2 to 3 times greater when both parents are obese [50, 54]. Besides the high probability of obesity-related genetics, obese parents encourage sedentary lifestyles, and such an environment promotes weight gain among family members and increases the risk of childhood obesity. A child has a 50% risk of being obese if one of his/her parents is obese, and the risk jumps to 80% when both parents are obese. A previous study [55] reported that the probability of a pre-school child being overweight is increased more than 2-fold when parents are overweight (OR = 2.43 [95% CI: 0.78–6.59]). Genetics can explain some of the observed intergenerational association, because parents and their offspring share at least 50% of their genetic perception [55].
This influence is weak when the relationship between parents is strained, e.g. in the case of divorce or when parents are forced to work late or during weekends. Observations from a previous study [56] indicate that, compared with children of married parents, those with divorced parents are 54% more likely to be overweight and/or obese [56]. Overweight and obesity are 54% more prevalent among school children of divorced parents compared with children of married parents (RR = 1.54 [95% CI: 1.21–1.95]), while abdominal obesity increased by 89% (RR = 1.89 [95% CI 1.35–2.65]) in the same group of children [56]. In other words, the failure of the parents’ relationship may have a negative impact on child psychology and promote food intake. Even though parents usually make time to take their children to the nearest shopping mall, or to a dentist clinic, they rarely teach their children healthy eating habits or how to maintain a healthy weight [57].
Towards a better child environment
At home, the environment surrounding the child is under the responsibility and the control of parents [51]. A simple, healthy environment can be created by exposing children to preventive factors and reducing their exposure to risk factors. For example, excessive weight gain during pregnancy is a well-known risk factor for obesity during childhood [2]. Excessive gestational weight gain is a risk factor for higher weight gain at birth [27–33, 63, 64]. This means that controlling weight gain during pregnancy within the recommended range for pregnant women can help in preventing and managing obesity during early childhood. Excessive weight gain during pregnancy can also cause serious health consequences to the mother throughout the pregnancy [26, 65, 66] and afterwards [67–69]. It has been estimated that a quarter of pregnancy complications are due to overweight and obesity. Thus, to avoid these complications, it is vital to have strict follow-up and adherence to the institute of medicine instructions regarding weight gain during pregnancy [66, 69]. Indeed, weight gain within recommended ranges improves both neonatal and maternal health outcomes.
Parents can promote healthy lifestyle behaviours such as physical activity, a healthy diet, and a healthy way of eating (Table II). This is of great importance because healthy behaviours that children develop early in their life may persist into adulthood [50]. If children do not learn healthy eating habits early on, they will soon become overweight, with a greater chance of becoming obese children [51, 55]. Parents must encourage their children to develop good, healthy habits such as regular physical exercise.
Table II
The relationship between feeding choices and childhood obesity
| Authors, year, country | Targeted variable | Outcome |
|---|---|---|
| Oddy et al. 2014 [70] Australia | Breastfeeding | From 1 to 8 years, children breast-fed for ≤4 months compared to ≥ 12 months had a significantly greater probability of exceeding the 95th percentile of weight |
| Zaqout et al. 2018 [71] Belgium | Breastfeeding | Exclusive breastfeeding had a significant improvement on physical fitness test performances in childhood |
| Giannì et al. 2014 [72] Italy | Breastfeeding vs other choices | Exclusively breastfed boys at 6 months of age had higher fat mass content compared to exclusively formula-fed infants |
| Li et al. 2020 [73] USA | Breastfeeding vs other choices | Choices of infant diets (i.e. breastfed, milk formula fed, soy formula fed) may have long-term and sex-specific effects on the cortical development and executive function and behaviour of children's brains |
| Fernández-Alvira et al. 2017 [74] European cohort | Diet pattern | Compared with processed food eaters, children who ate a healthy diet were less prone to have increased BMIs and waist circumferences |
| Jiang et al. 2006 [55] China | Food restriction | There was a 2.68 increase in child overweight with food restriction (OR = 2.68 [95% CI: 1.64–4.29]) |
| Papoutsou et al. 2017 [75] European cross-sectional | Solid food introduction | Compared with late solid food introduction (≥ 7 months of age), early solid food introduction (< 4 months of age) was associated with a 37% protection against overweight/obesity among children that ceased exclusive breastfeeding earlier (OR = 0.63 [95% CI: 0.47–0.84]) |
| Magriplis et al. 2021 [76] Greece | Added sugars | When ≥ 10% of total energy derived from added sugars, the risk of being overweight and/or obese was 2.57 (p = 0.002) and 1.77 (p = 0.047) times greater compared to < 10%, when accounting for food groups and macronutrient intakes, respectively |
Limiting TV viewing and internet usage, avoiding processed snacks, limiting sugary beverages, sweets, and junk food. Viewing TV for a long period is strongly associated with weight gain and child overweight/obesity independently of diet and exercise [55], while having a TV in the child’s bedroom makes it even worse [77]. A previous study [55] reported a 56% increase in child overweight when watching television > 2 hours/day (OR = 1.56 [95% CI: 1.17–2.09]). Watching television for long periods at a time not only restricts energy expenditure, but it also encourages snacking, and children may not stop eating even when they are full because of the distraction. Therefore, TV viewing should be limited as much as possible without allowing children to eat or drink while watching television or playing games [57].
The role of educational institutes
Schools and educational institutes play a significant impact on the development and shaping of child behaviour [78]. They serve as environments where children spend a considerable amount of time and interact with peers, teachers, and other adults. The impact of school on child behaviour can be profound and multifaceted, influencing various aspects of their social, emotional, cognitive, and behavioural development [79]. The environment that schools of today provide depends on whether the school is private, governmental, or mixed. While some schools provide food, processed snacks, and sugary beverages, others provide more sports activities on a daily basis. Parents are usually in charge of selecting the right school for their children. Through parental support, educational institutes may promote healthy dietary habits and physical activity, and prevent obesity in children [80, 81]. Furthermore, the opinion of children towards school these days is very different from their parents’ opinion in their school days.
School for a child is a good environment not just only to learn or to study, but also to exchange PlayStation CDs, movies, and games with other children. Negatively, even sharing or buying drugs, e.g. alcohol, cigarette smoking, marijuana, hashish (cannabis), crack, and other drugs (i.e. cocaine) are reported daily in high schools in developed and developing countries [82]. Previous [83] and recent available studies [84] have reported that high school students who use illicit drugs show deficits in family relationships. This shows how the behaviour of a child can be affected by other children’s behaviours. Furthermore, this also shows the size of the problem when the home effect is absent [84]. To decrease the prevalence of childhood obesity, parents and schools must come together with a preventive approach towards a better and, of course, a healthier environment for the benefit of their children [85].
The role of the neighbourhood environment
There has been an increase in attention regarding the role of neighbourhoods and residential environments in explaining differences in health outcomes [86]. Indeed, the neighbourhood environment can have a significant impact on child behaviour and development due to its influence on various aspects of a child’s life, including overweight and obesity [60]. The neighbourhood where a child grows up plays a crucial role in shaping child behaviours and overall development [86]. It moulds their experiences, opportunities, and interactions with the physical, social, and economic environment. Neighbourhoods with higher levels of safety and lower crime rates create a more conducive environment for children to engage in outdoor play, physical activity, and social interactions, and the opposite is also true [60]. Children in safer neighbourhoods are more likely to exhibit positive behaviours such as outdoor play, walking or biking to school, and socialising with peers. Those living in disadvantaged neighbourhoods (unsafe neighbourhoods) may experience heightened stress, fear, and avoidance behaviour. Children in neighbourhoods with limited access to recreational facilities may have fewer opportunities for physical activity and outdoor play, leading to sedentary behaviour patterns and increased risk of obesity and related health consequences [87]. Neighbourhoods with access to parks, playgrounds, recreational facilities, and green spaces provide opportunities for physical activity, sports, and outdoor play, which promote healthy behaviours and social interactions among children [55, 88].
Overall, the neighbourhood environment plays a critical role in shaping child behaviours by providing opportunities for physical activity, social interactions, access to educational resources, healthy food options, and supportive community networks. Creating supportive neighbourhood environments that promote safety, access to recreational facilities, educational opportunities, social cohesion, and healthy lifestyles is essential for promoting positive child behaviours and overall well-being.
What is needed?
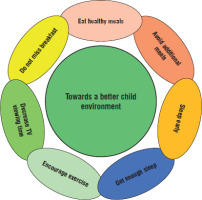
Creating a healthy environment around children is essential towards decreasing the prevalence of overweight and obesity (Fig. 3). In addition, promoting healthy behaviours, fostering supportive home and school environments, and addressing social determinants of health are essential for preventing and managing childhood obesity effectively [81]. The family environment, including parental caregiving practices, parental involvement, family dynamics, and household routines, significantly influences child behaviour [89, 90]. Warm, supportive care and greater communication between parents and their children, and a nurturing family environment promote positive child outcomes, including healthy attachment, social skills, emotional regulation, and academic achievement [90]. Educational institutes and/or schooling have a significant impact on child psychology, influencing various aspects of cognitive, social, emotional, and behavioural development. The characteristics of the community and neighbourhood environment, including access to resources, safety, social support networks, and neighbourhood cohesion, influence child behaviour. Positive community environments with access to parks, recreational facilities, and community programs promote physical activity, social engagement, and healthy development. Some children may have underlying behavioural disorders that affect their actions. Identifying and addressing these disorders is crucial for managing child behaviour. It is suggested that for better outcomes, local governments and educational institutes’ practitioners must focus on improving collaboration between school and home to optimise children’s subjective well-being by reducing their homework anxiety and increasing the harmonious family atmosphere. Thus, more family communication and support, more social interaction, and less parental-child interaction and family conflict [91].
Finally, to decrease childhood obesity, further approaches must be implanted. Parents must be considered as cornerstones in the application of any of these approaches. Figure 3 displays selected factors towards the creation of a healthy environment around children. Such interventions may promote healthy food choices, improve the psychosocial well-being of children, and support families to create a healthy environment for children.
Figure 3
Instructions for parents and caregivers towards the creation of a healthy environment for children. All parents must encourage a protective healthy environment at home to decrease the risk of overweight and obesity among their children. Under these circumstances, children will develop healthier habits, and the chances of decreasing childhood obesity will be increased. Eating a healthy diet, along with getting enough physical activity and restful sleep, can help children grow up healthy and prevent overweight and obesity
Conclusions
The prevalence of childhood obesity continues to increase globally, posing significant challenges for public health systems and underscoring the importance of comprehensive strategies to address this epidemic. Child behaviour plays a crucial role in the crisis of childhood obesity because it directly influences lifestyle habits, dietary choices, physical activity levels, and overall health outcomes. The combined influence of parents, schools, and the local community creates an environment that shapes a child’s behaviour, social skills, and overall development. Collaboration and coordination among these elements are essential for promoting positive behaviour and well-being in children. Finally, promoting healthy behaviours and creating supportive environments that encourage healthy eating and active living are essential strategies for addressing childhood obesity and promoting the health and well-being of children.

 ENGLISH
ENGLISH